
Lead

Lead is a heavy, low melting, bluish-gray metal that occurs naturally in the Earth’s crust. However, it is rarely found naturally as a metal. It is usually found combined with two or more other elements to form lead compounds.
Metallic lead resists corrosion (in other words, it is not easily affected by air or water). When exposed to air or water, thin films of lead compounds form and protect the metal. Lead is easily molded and shaped, and it can be combined with other metals to form alloys. Lead and lead alloys are commonly found in pipes, storage batteries, weights, shot and ammunition, cable covers, and sheets used to shield us from radiation. Storage batteries in cars and other vehicles use the largest amounts of lead.
Lead compounds are used as pigments in paints, dyes, and ceramic glazes and in caulk. In recent years, the amount of lead used in these products has been reduced to minimize lead’s harmful effects on people and animals. Lead was once added to gasoline to increase octane rating, but it was phased out in the 1980s, and banned in gasoline for motor vehicles beginning January 1, 1996. Lead still can be used in gasoline for off-road vehicles and airplanes. It also is still used in some developing countries. Lead used in ammunition, which is the largest non-battery use, has remained fairly constant. However, even in bullets and shot and in fishing sinkers, lead is being reduced because of its harm to the environment.
Most lead used by industry comes from mined ores (“primary”) or from recycled scrap metal or batteries (“secondary”). In the United States, lead is mined mainly in Alaska and Missouri. However, most lead today is “secondary” lead obtained from lead-acid batteries. Ninety-seven percent of these batteries reportedly are recycled.
Lead occurs naturally in the environment. However, most of the high levels found in the environment come from human activities.
Lead use increased the most during 1950–2000 and reflected increasing worldwide use of leaded gasoline. Lead can enter the environment through releases from mining lead and other metals and from factories that make or use lead, lead alloys, or lead compounds. Lead is released into the air when coal, oil, or waste is burned. Before leaded gasoline was banned, most lead released into the U.S. environment came from vehicle exhaust. In 1979 in the United States, cars released 208.1 million pounds (94.6 million kilograms) of lead into the air. In 1989, when lead was limited but not banned, cars released only 4.8 million pounds (2.2 million kilograms). Since the U.S. Environmental Protection Agency (EPA) banned leaded gasoline for highway transportation in 1996, the amount of lead released into the air has decreased further. Before the 1950s, another way lead got into the environment was through pesticides applied to fruit orchards. Once lead gets into the atmosphere, it can travel long distances if the lead particles are very small. Lead is removed from the air by rain and by particles falling to land or into surface water.

Sources of lead in dust and soil include lead that falls to the ground from the air and from weathering and chipping of paint that contains lead (lead-based paint) from buildings, bridges, and other structures. Landfills can contain waste from lead ore mining; ammunition manufacturing; and other industrial activities, such as battery production. Disposal of lead-containing products contributes to lead in municipal landfills. Past uses of lead—such as in gasoline—are a major contributor to lead in soil, and higher levels of lead in soil are found near roadways. Most lead in inner city soils comes from old houses with lead-based paint and previous automotive exhaust emitted when gasoline contained lead.e who has had lead poisoning.
Once lead falls onto soil, it sticks strongly to soil particles and stays in the upper layer of soil. That is why past uses of lead, such as in gasoline, house paint, and pesticides, are so important in the amount of lead found in soil.
Small amounts of lead can enter rivers, lakes, and streams when rainwater moves soil particles. Small amounts of lead from lead pipe or solder can be released into water when the water is acidic (or “soft”). Lead can stick to soil particles or sediment in water for many years. Movement of lead from soil particles into groundwater is unlikely unless the rain falling on the soil is acidic. Movement of lead from soil also depends on the type of lead compound and on the physical and chemical nature of the soil.
Sources of lead in surface water or sediment include deposits of lead-containing dust from the atmosphere, wastewater from industries that handle lead (mainly iron and steel industries and lead producers), urban runoff, and mining piles.
Sunlight, air, and water can change some lead compounds into other forms of lead. However, elemental lead cannot be broken down.
Levels of lead can build up in plants and animals from areas where air, water, or soil are contaminated with lead. If animals eat contaminated plants or animals, most of the lead they eat will pass through their bodies.
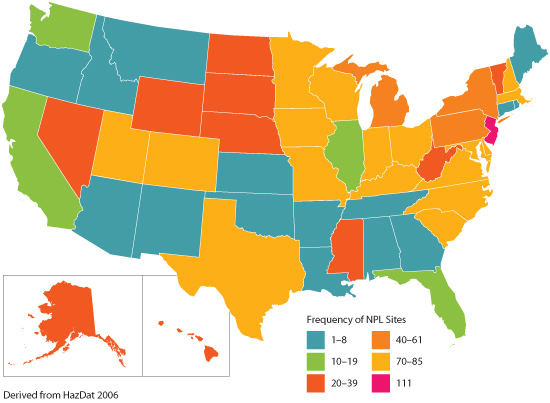
Lead is commonly found in soil, especially near roadways, older houses, old orchards, mining areas, industrial sites, power plants, incinerators, landfills, and hazardous waste sites.

People living near hazardous waste sites can be exposed to lead and chemicals that contain lead by breathing air, drinking water, eating food, or swallowing dust or dirt that contains lead. Tap water in houses that have lead pipes can contain lead, especially if the water is acidic. If you are not certain whether an older building contains lead pipes, you should let the water run a while before drinking it so that any lead formed in the pipes can be flushed out. People living in areas where old houses were painted with lead-based paint can be exposed to higher levels of lead in dust and soil. Likewise, people who live near busy highways or on old orchard land where lead arsenate pesticides were once used can be exposed to higher levels of lead. People who work in jobs where lead is used or who have hobbies in which lead is used, such as making stained glass, also can be exposed to lead.
Food can contain small amounts of lead. However, lead solder is no longer used in cans, so very little lead is found in food. Therefore, the chance of exposure to lead in canned food from lead-soldered containers was greatly reduced. (Some other nations still use lead-soldered cans.) In the most recent studies, lead was not detectable in most foods, and the average dietary intake was about 1 microgram of lead (a microgram is a millionth of a gram) per kilogram of body weight (µg/kg) per day. Leafy fresh vegetables grown in lead-containing soils can have lead-containing dust on them. Lead also can enter foods put into improperly glazed pottery or ceramic dishes or into leaded-crystal glassware. Illegal whiskey made using stills that contain lead-soldered parts (such as truck radiators) also can contain lead.
In addition, cigarette smoke contains small amounts of lead. Also, children can be exposed to lead by putting their hands that have touched lead-containing soil or dust into their mouths.

In general, very little lead is found in lakes, rivers, or groundwater used to supply the public with drinking water. More than 99% of all publicly supplied drinking water contains less than 0.005 parts of lead per million parts of water (ppm). However, the amount of lead taken into your body through drinking water can be higher in communities with acidic water supplies. Acidic water makes it easier for the lead found in pipes, leaded solder, and brass faucets to be dissolved and to enter the water we drink. Public water treatment systems are now required to make water less acidic. Plumbing that contains lead can be found in public drinking water systems and in houses, apartment buildings, and public buildings that are more than 20 years old. However, as buildings age, mineral deposits form a coating on the inside of the water pipes that insulates the water from lead in the pipe or solder, thus reducing the amount of lead that can leach into the water. Since 1988, regulations require that drinking water coolers must not contain lead in parts that come into contact with drinking water.
Breathing or swallowing dust and dirt in the air is another way you can be exposed to lead. In 1984, burning leaded gasoline was the largest source of lead emissions. Now, very little lead in the air comes from gasoline. Other sources of lead in the air include releases to the air from industries involved in iron and steel production, lead-acid-battery manufacturing, and nonferrous (brass and bronze) foundries. Lead released into air also can come from burning of solid waste that contains lead, windblown dust, volcanoes, exhaust from workroom air, burning or weathering of lead-painted surfaces, fumes and exhaust from leaded gasoline, and cigarette smoke.
Skin contact with dust and dirt containing lead occurs every day. For example, inexpensive cosmetic jewelry pieces sold to the general public might contain high levels of lead that can be transferred to the skin during routine handling. However, not much lead can get into your body through your skin.
At home, you or your children might be exposed to lead if you take certain home remedy medicines that contain lead compounds. Lead compounds are in some non-Western cosmetics, such as surma and kohl. Some types of hair colorants, cosmetics, and dyes contain lead acetate. Read the labels on hair coloring products, use them with caution, and keep them away from children.
Exposure to lead occurs in many jobs. People exposed at work are usually exposed by breathing air that contains lead particles. People who work in lead smelting and refining industries, brass/bronze foundries, rubber products and plastics industries, soldering, steel welding and cutting operations, battery manufacturing plants, and lead compound manufacturing industries can be exposed to lead. Construction and demolition workers and workers at municipal waste incinerators, pottery and ceramics industries, radiator repair shops, and other industries that use lead solder also can be exposed. Painters who sand or scrape old paint can be exposed to lead in dust. Between 0.5 million and 1.5 million workers are exposed to lead in the workplace every year. In California alone, more than 200,000 workers are exposed to lead. Families of workers can be exposed to higher levels of lead when workers bring home lead dust on their work clothes.
You also can be exposed to lead at home if you work with stained glass as a hobby, make lead fishing weights or ammunition, or are involved in home renovation that involves removing old lead-based paint.
Some of the lead that enters your body comes from breathing dust or chemicals that contain lead. Once this lead gets into your lungs, it travels quickly through your blood to other parts of your body.
Particles that are too large to get into your lungs can be coughed up and swallowed. You also can swallow lead by eating food and drinking liquids that contain it. Most lead that enters your body comes through swallowing, even though very little of the amount you swallow actually enters your blood and other parts of your body. The amount that gets into your body from your stomach partly depends on when you ate your last meal. It also depends on how old you are and how well the lead particles dissolved in your stomach juices. Experiments using adult volunteers showed that, for adults who had just eaten, the amount of lead that got into the blood from the stomach was only about 6% of the total amount of lead taken in. In adults who had not eaten for a day, about 60%–80% of lead in the stomach got into their blood. In general, if adults and children swallow the same amount of lead, more will enter the blood of children than of adults. Children absorb about 50% of the lead they ingest.
Dust and soil that contain lead may get on your skin, but only a small portion of the lead will pass through your skin and enter your blood if it is not washed off. You can, however, accidentally swallow lead that is on your hands when you eat, drink, smoke, or apply cosmetics (for example, lip balm). More lead can pass through skin that has been damaged (for example, by scrapes, scratches, and wounds). The only kinds of lead compounds that easily penetrate the skin are the additives in leaded gasoline. Because leaded gasoline is no longer sold to the general public, you are not likely to encounter lead that can enter through the skin.
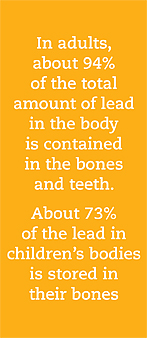
Shortly after lead gets into your body, it travels in the blood to the soft tissues and organs (such as the liver, kidneys, lungs, brain, spleen, muscles, and heart). After several weeks, most of the lead moves into your bones and teeth. In adults, about 94% of lead in the body is contained in the bones and teeth. About 73% of lead in children’s bodies is stored in their bones. Some lead can stay in your bones for decades; however, some lead can leave your bones and reenter your blood and organs under certain circumstances (during pregnancy and periods of breast feeding, after a bone is broken, and during advancing age.
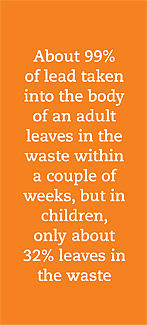
Your body does not change lead into any other form. Once it is taken in and distributed to your organs, the lead that is not stored in your bones leaves your body in your urine or your feces. About 99% of lead taken into the body of an adult leaves in the waste within a couple of weeks, but in children, only about 32% of the lead leaves in the waste. For people who are continuously exposed, not all of the lead that enters the body is eliminated, which can result in accumulation of lead in body tissues, especially bone.
The effects of lead are the same whether it enters the body through breathing or swallowing. Lead can affect almost every organ and system in your body.
Lead toxicity mainly affects the nervous system. In adults, long-time exposure to lead at work has caused low scores on some tests that measure nervous system function. Lead exposure can cause weakness in fingers, wrists, or ankles and small increases in blood pressure, particularly in middle-aged and older people. Lead exposure also can cause anemia. At high levels of exposure, lead can severely damage the brain and kidneys in adults and in children and ultimately cause death. In pregnant women, high levels of exposure can cause miscarriage. High-level exposure in men can damage the organs that produce sperm. There is evidence that these effects may persist beyond childhood.
Children with high blood lead levels do not have specific symptoms. However, health workers can find out whether a child may have been exposed to harmful levels of lead by taking a blood sample. They can also find out how much lead is in a child’s bones by taking a special type of x-ray of the finger, knee, or elbow. This type of test, however, is not routine.

We have no certain proof that lead causes cancer in humans. Kidney tumors have developed in rats and mice that had been given large amounts of some lead compounds. The U.S. Department of Health and Human Services has determined that lead and lead compounds are reasonably anticipated to be human carcinogens based on limited evidence from studies in humans and sufficient evidence from studies in animals, and EPA has determined that lead is a probable human carcinogen. The International Agency for Research on Cancer (IARC) has determined that inorganic lead is probably carcinogenic to humans. IARC determined that the carcinogenicity in humans of organic lead compounds cannot be classified because evidence from studies in humans and animals is inadequate.
Studies by CDC show that the levels of lead in the blood of U.S. children have been getting lower.
The reason for decreasing blood lead levels is decrease in use. For example, lead is banned from gasoline, residential paint, and solder used for food cans and water pipes. However, about half a million U.S. children 1–5 years old are believed to have levels equal or greater than 5 micrograms of lead per deciliter of blood (μg/dL), the level used to identify children with blood lead levels that are much higher than most children’s levels.
Compared with adults, children are more easily exposed to lead. Children are exposed throughout their lives. They can be exposed in the womb if their mothers have lead in their bodies. Babies can swallow lead when they breast feed or eat foods and drink water that contains lead. Babies and children can swallow and breathe lead in dirt, dust, or sand while they play on the floor or ground. The dirt or dust on children’s hands, toys, and other items can have lead particles in it. In some cases, children swallow nonfood items, such as paint chips, which can contain very large amounts of lead, especially in and around older houses that were painted with lead-based paint. The paint in these houses often chips off and mixes with dust and dirt. Some old paint contains as much as 50% lead. Also, compared with adults, a bigger proportion of the amount of lead swallowed enters the blood of children.
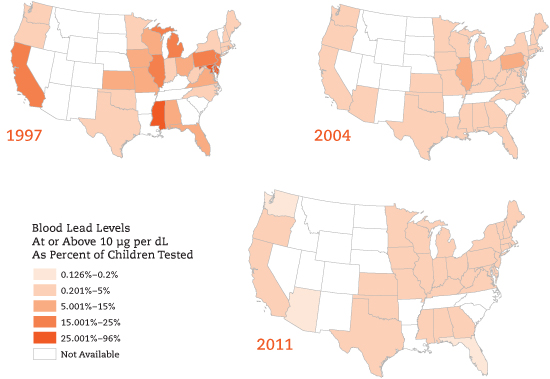
Source: CDC
Children are more sensitive than adults to the health effects of lead. No safe level of lead in blood has been determined for children. Lead affects children in different ways depending on how much lead they swallow. A child who swallows large amounts of lead can develop anemia, kidney damage, colic (severe “stomach ache”), muscle weakness, and brain damage, which ultimately can kill the child. In some cases, the amount of lead in the child’s body can be lowered by giving him or her drugs that help eliminate lead from the body. If a child swallows smaller amounts of lead, such as dust containing lead from paint, much less severe but still important effects on blood, development, and behavior can occur. In this case, recovery is likely once the child is removed from the source of lead exposure, but there is no guarantee that the child will completely avoid all long-term effects of lead exposure. At still lower levels of exposure, lead can affect a child’s mental and physical growth. Fetuses whose mothers had a lot of lead in their bodies can be born prematurely and have lower weights at birth. Exposure in the womb, in infancy, or in early childhood also can slow mental development and cause lower intelligence later in childhood. Evidence shows that these effects might persist beyond childhood.
Children with high levels of lead in their blood do not have specific symptoms. However, health workers can find out whether a child might have been exposed to harmful levels of lead by taking and testing a blood sample. They can also find out how much lead is in a child’s bones by taking a special type of x-ray of the finger, knee, or elbow. This type of test, however, is not routine.
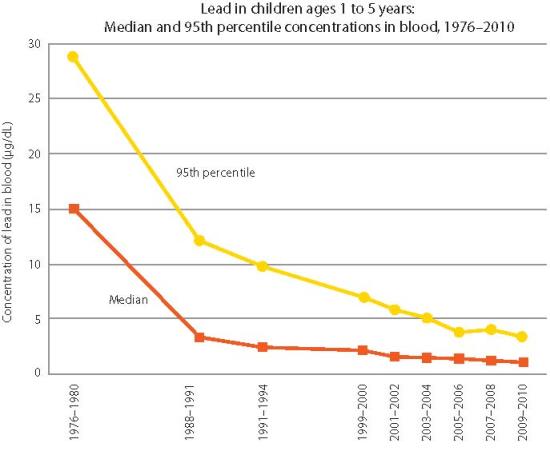
The EPA reports that the largest decrease in blood lead levels was observed between 1970 and 1990, when lead was removed from gasoline. Additional decreased in blood lead levels from 1990-2000 and 2009-2010 are attribute the focus on removing lead-based paints in homes.
Data: Centers for Disease Control and Prevention, National Center for Health Statistics and National Center for Environmental Health, National Health and Nutrition Examination Survey
America’s Children and the Environment, Third Edition

If your doctor finds that you have been exposed to substantial amounts of lead, ask whether your children might also have been exposed. Your doctor might need to ask your state health department to investigate.
The most important way your family can lower exposures to lead is to know about the sources of lead in your home and avoid exposure to these sources. Some homes or day-care facilities may have more lead in them than others. Families who live in or visit these places can be exposed to higher amounts of lead. These places include homes built before 1978 that might have been painted with lead-based paint. If you are buying a home that was built before 1978, you might want to know whether it contains lead-based paint. Federal government regulations require a person selling a home to tell the real estate agent or person buying the home of any known lead hazards on the property. Adding lead to paint is no longer allowed. Houses built before 1978 still might have lead-based paint on interior walls, floors, ceilings, and window sills or on the outside walls of the house. Even if a previous owner scraped off the paint, paint chips and lead-containing dust still could be in the yard soil. Decaying, peeling, or flaking paint can introduce lead into household dust, so such areas should be repainted. In some states, homeowners can have the paint in their homes tested by their local health departments. The National Lead Information Center (1-800-424-5323) lists approved risk assessors (people who are qualified to assess the possible risks of a site) and of approved testing laboratories (for soil, paint, and dust).
Sanding surfaces painted with lead-based paint or using heat to peel the paint can expose you to high levels of lead. Many cases of lead poisoning have resulted from do-it-yourself home renovations. Therefore, any renovations should be performed by a licensed contractor who will minimize exposure to household members. The area being renovated should be isolated from the rest of the house to lessen exposure to lead-containing dust. The federal government requires that contractors who test for or remove lead must be certified by the EPA or an EPA-approved state program. Ask to see certifications of potential contractors. Your state health department or environmental protection division can help identify certified contractors for you. Additional information can be found at http://www2.epa.gov/lead/evaluating-and-eliminating-lead-based-paint-hazards#contractor .

You can lower the possibility of your children swallowing paint chips by discouraging them from chewing on or putting these painted surfaces in their mouths and by making sure that they wash their hands often, especially before eating. Areas where levels of lead in dirt and dust might be especially high are near old houses, highways, or old orchards. Some children eat dirt (the term for this activity is pica). Discourage your children from eating dirt and from participating in other hand-to-mouth activities.
Non-Western folk remedies used to treat diarrhea or other ailments can contain substantial amounts of lead. Examples of these include Alarcon, Ghasard, Alkohl, Greta, Azarcon, Liga, Bali Goli, Pay-loo-ah, Coral, and Rueda. If you give these substances to your children or if you are or nursing or pregnant, you could expose the children or fetus to lead. You should know the ingredients of any medicines that you or your children use.
Older homes that have plumbing with lead can have higher amounts of lead in drinking water. Interior plumbing installed before 1930 is most likely to contain high levels of lead. Copper pipes now have replaced lead pipes in most residential plumbing. You cannot see, taste, or smell lead in water, and boiling your water will not get rid of lead. Therefore, if your house has a water-lead problem, EPA recommends that anytime you have not used water in a particular faucet for 6 hours or longer, you should flush the cold water pipes by running water until it is cold (5 seconds–2 minutes). Because lead dissolves more easily in warm water than in cold water, you should use only cold water for drinking, cooking, and preparing baby formula. Contact your local health department or water supplier to find out about testing your water for lead. If these tests show a major presence of lead, consult your water supplier or local health department about possible solutions.
If you work in a place where lead is used, you can bring lead home in the dust on your hands or clothes. Lead dust is likely to be found in places where lead is mined or smelted; where car batteries are made or recycled; or where electric cable sheathing, crystal glass, or certain types of ceramic pottery are made. Pets can bring lead into the home in dust or dirt on their fur or feet if they spend time in places that have high levels of lead in the soil.
In children, swallowing lead in house dust or soil is a very important path of exposure. Regularly washing the hands and face to remove lead dusts and soil, especially before meals, can lessen the possibility that lead on the skin will be accidentally swallowed during eating. Your family can lower exposure by regularly cleaning the home of dust and tracked-in soil. Door mats can help decrease the amount of soil tracked into the home; removing your shoes before entering the home also helps. By planting grass and shrubs over areas of bare soil in the yard, you can lower contact by children and pets with soil and lower the amount of soil tracked into the home.

If you are exposed to lead dusts at work, you can keep these dusts away from your children by showering and changing your clothes before leaving work and by bagging your work clothes before you bring them home for cleaning. Proper ventilation and cleaning during and after hobby activities, home or auto repair activities, and hair coloring with products that contain lead will decrease the possibility of exposure.
Dust that contains lead can be deposited on plant surfaces, and the roots of some edible plants can take up lead from the soil. Therefore, home gardening also can contribute to exposure if the produce is grown in soils that have high concentrations of lead. To remove surface deposits of lead, you should wash vegetables very well before eating them. Certain hobbies and home or car repair activities like radiator repair also can add lead to the home. These activities include soldering glass or metal, making bullets or slugs, or glazing pottery. Some types of paints and pigments that are used as facial make-up or hair coloring contain lead. Cosmetics that contain lead include surma and kohl, which are popular in some Asian countries. Read the labels on hair coloring products, and keep hair dyes that contain lead acetate away from children. Do not allow children to touch hair that has been colored with lead-containing dyes or any surfaces that have come into contact with these dyes because lead compounds can rub off onto their hands and be transferred to their mouths.
Children need to have proper nutrition and eat a balanced diet of foods that supply adequate amounts of vitamins and minerals, especially calcium and iron. Good nutrition lowers the amount of swallowed lead that passes into the bloodstream and might lower some of the toxic effects of lead.
The amount of total lead in the blood can be measured to determine whether you have been exposed to lead.

This test shows whether you have been recently exposed to lead. Lead can be measured in teeth or bones by x-ray techniques, but these methods are not widely available. These tests show long-term exposures to lead. The primary screening method is measurement of lead in blood. Exposure also can be evaluated by measuring erythrocyte protoporphyrin (EP) in blood samples. EP is a part of red blood cells that increases when the amount of lead in the blood is high. However, the EP level is not sensitive enough to identify children who have elevated blood lead levels below about 25 μg/dL. These tests usually require special analytical equipment that is not available in a doctor’s office, but your doctor can draw blood samples and send them to appropriate laboratories for analysis.
The federal government develops regulations and recommendations to protect public health. Regulations can be enforced by law.

The EPA, the Occupational Safety and Health Administration (OSHA), and the Food and Drug Administration (FDA) are some federal agencies that develop regulations for toxic substances. Recommendations differ from regulations in that they provide valuable guidelines to protect public health but cannot be enforced by law. The Agency for Toxic Substances and Disease Registry (ATSDR) and the National Institute for Occupational Safety and Health (NIOSH)—both part of CDC—are two federal organizations that develop recommendations for toxic substances.
Regulations and recommendations can be expressed as “not-to-exceed” levels. This means that levels of a toxic substance in air, water, soil, or food that are not higher than a critical value that is usually based on levels that affect animals; these levels are then adjusted to levels that will help protect humans. Sometimes these not-to-exceed levels differ among federal agencies because the exposure times (an 8-hour workday or a 24-hour day), animal studies, or other factors they use differ.
These agencies update their recommendations and regulations as more information becomes available. For the most current information, check with the federal agency or organization that provides it.
The most important step parents, doctors, and others can take is to prevent lead exposure before it occurs. CDC recommends focusing on primary prevention of lead exposure. Experts now use a reference level of 5 micrograms per deciliter to identify children with blood lead levels that are much higher than most children’s levels. This new level is based on the U.S. population of children ages 1-5 years who are in the highest 2.5% of children when tested for lead in their blood. This reference value is based on the 97.5th percentile of the National Health and Nutrition Examination Survey (NHANES)’s blood lead distribution in children. CDC will update the reference value every four years using the two most recent NHANES surveys. Chelation therapy is recommended for children with levels above 45 µg/dL. Medicaid and most private health insurance plans cover blood tests to measure lead in children’s blood.
EPA requires that the concentration of lead in air be no higher than 1.5 micrograms per cubic meter (μg/m3) averaged over 3 months. The Clean Air Act Amendments (CAAA) of 1990 banned the sale of leaded gasoline as of December 31, 1995.
Under the Lead Copper Rule, EPA requires testing of public water systems. If more than 10% of the samples at homes contain lead levels higher than 0.015 milligrams per liter of water (mg/L), actions must be taken to lower these levels. Testing for lead in drinking water in schools is not required unless a school is regulated under a public water system. The 1988 Lead Contamination Control Act (LCCA) was created to help reduce lead in drinking water at schools and day-care centers. The LCCA created lead monitoring and reporting requirements for schools and the replacement of fixtures that contain high levels of lead. However, the provisions in the LCCA are not enforceable by the federal government, and individual states can voluntarily comply with these provisions or create their own.
To help protect young children, the Consumer Product Safety Commission requires that the concentration of lead in most paints available through normal consumer channels be not more than 0.06%. The Federal Hazardous Substance Act bans children’s products containing hazardous amounts of lead.
The U.S. Department of Housing and Urban Development (HUD) develops recommendations and regulations to prevent exposure to lead. HUD requires that federally funded housing and renovations, public and Indian housing be tested for lead-based paint hazards and that such hazards be fixed by covering or removing the paint. EPA and HUD have determined that paint should be removed or otherwise treated if it contains lead levels equal to or more than 1.0 milligram of lead per square centimeter (mg/cm2) of surface area on interior or exterior surfaces of dwellings. HUD is determining the best ways of covering or removing lead-based paint in housing.
EPA has developed standards for lead-paint hazards, lead in dust, and lead in soil. To educate parents, homeowners, and tenants about lead hazards, lead poisoning prevention in the home, and the process of decreasing lead, EPA has published several general information pamphlets. Copies of these pamphlets are available from the National Lead Information Center or from various Internet sites, including http://www2.epa.gov/lead .
OSHA regulations limit the concentration of lead in workroom air to 50 μg/m3 for an 8-hour workday. If a worker has a blood lead level of 50 μg/dL or higher, then OSHA requires that the worker be removed from the workroom where he or she is being exposed to lead.
FDA includes lead on its list of poisonous and harmful substances. FDA considers food packaged in cans that contain lead solders to be unsafe. For example, tin-coated lead foil has been used to cover the cork and neck areas of wine bottles for decoration and to prevent insect infestations. Because lead could become a component of the wine, the use of such foil violates the Federal Food, Drug, and Cosmetic Act. FDA has determined that several ingredients, such as food dyes, that are directly added to human food are “generally recognized as safe” when used in accordance with current good manufacturing practices. Some of these ingredients contain allowable concentrations of lead that range from 0.1 ppm to 10 ppm.
ATSDR also can tell you the location of occupational and environmental health clinics. These clinics specialize in recognizing, evaluating, and treating illnesses that result from exposure to hazardous substances.
Agency for Toxic Substances and Disease Registry
Division of Toxicology and Human Health Sciences
1600 Clifton Road NE,
Mailstop F-57
Atlanta, GA 30333
Toll-free information and technical assistance:
1-800-CDCINFO (1-800-232-4636)
Sources
ATSDR Toxicological Profile for Lead
CDC National Center for Environmental Health, Lead Program
Environmental Protection Agency, Lead Program
