Features from the Front Line: Mississippi
Spotlight on Mississippi State Department of Health
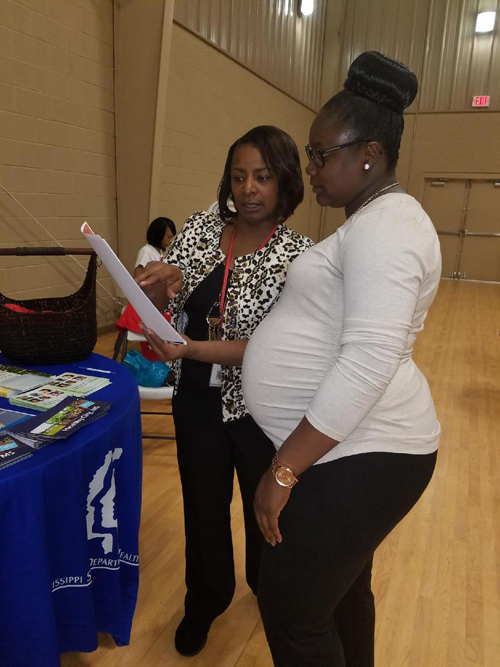
Lisa Moore, Community Health Director for District 1 (left) provides Zika prevention information during the Grenada Health Summit on April 1, 2017.
Embracing Communication Outreach to Fight Zika
With a population of nearly three million people, Mississippi faces many public health challenges, including a high poverty level and one of the country’s highest infant mortality rates — currently 9.2 infant deaths per 1,000 births. The Mississippi State Department of Health continues to focus on these health challenges, but in 2016 added another priority, raising awareness and building capacity to confront the threat of Zika virus (Zika) infections.
Relying on Local Outreach, Interpreters
As of March 2017, seven of Mississippi’s nine public health districts have accepted CDC Zika funding to do local outreach, says Alyce Stewart, DrPH, MPH, MCHES, director of Mississippi’s Bureau of Genetic Services, which oversees Zika funding directed to the Birth Defects Registry.
“One of the strategies the Birth Defects program initiated when we received Zika funding was to make sure we addressed multiple racial and ethnic groups,” says Stewart. “We have a system of interpreters throughout the state we work closely with to ensure that all information we provide is culturally and linguistically appropriate.”
Since April 2017, community health directors and public health educators have conducted dozens of outreach activities in the community at schools and universities, churches, health professional meetings, and health summits. The state has provided approximately 6,000 educational materials and more than 8,500 Zika coloring books to school-aged children.
Moving from a Passive to Active Birth Defects Registry
In addition to community outreach, Mississippi also used funding to hire a birth defects nurse consultant skilled in medical record data abstraction. Today, 13 regional coordinators, including nurses and social workers, received medical data abstraction training. In August 2017, CDC funded a full-time field assignee to provide Zika training to healthcare providers statewide.
“One of the main challenges we’ve had is taking our passive registry and building a more active one to get hospitals to send data to us,” notes Chana Winder, RN, MSN, the CDC-funded Birth Defects Nurse Consultant. Mississippi conducts follow-up care for Zika-positive infants and for infants without a positive test who have other diagnoses that may be related to congenital Zika syndrome.
“Through Chana’s work we have a true baseline of the birth defects in the general population so if there is ever a reason to believe we have a local transmission of Zika, we will be able to rapidly identify those cases,” explains Sheryl Hand, BSN, Pregnancy Registry/Arboviral Nurse Consultant. Hand plays a major role in the Mississippi Zika response by helping to guide activities through the CDC Epidemiology and Laboratory Capacity for Infectious Diseases (ELC) funding. According to her, the funding has enabled Mississippi to enhance the state lab to do molecular and serologic testing for both Zika and another mosquito-borne disease, chikungunya.
Faster Case Reporting
Mississippi also has strengthened its links with area hospitals. All but one of the state’s 43 “birthing” hospitals are now on board with providing patient data faster. Currently four hospitals provide remote access to patient records, but more will be providing these data in the future. “Our ultimate goal is to have community health records used by all hospitals so a physician in south Mississippi can see the health record of a patient who went to north Mississippi,” says Hand.
Mississippi also is moving toward a centralized database system to access both pregnancy and birth defects data and has expanded its mosquito surveillance to identify if Aedes aegypti mosquitoes (mosquitoes that can carry Zika) are present in various counties. Part of the mosquito control effort includes identifying areas at high-risk so municipalities can be prepared in the event of local Zika transmission. Their goal is to have an environment assessment around the home and a one-on-one consult with the patient within 48 hours of being notified of a case.
But the best aspect of the Zika response, emphasizes Stewart, is the collaboration that has resulted across the health department. “We were working in silos but were able to get to the table, talk and establish a foundation to fight Zika,” she concludes.