Recommendations for Fully Vaccinated People
COVID-19 Homepage
Risk of Exposure to COVID-19
Racial and Ethnic Health Disparities
‹View Table of Contents
Conditions in the places where people live, learn, work, play, and worship affect a wide range of health risks and outcomes, such as COVID-19 infection, severe illness, and death. These conditions are known as social determinants of health.
Social determinants of health that may influence risk of exposure to COVID-19 include neighborhood and physical environment, housing, occupation, education, and economic stability. Discrimination, which includes racism, shapes the social and economic factors that put people at increased risk for COVID-19 infection.1,2,3,4,5 Unfortunately, discrimination exists in systems meant to protect well-being and health, such as housing, education, criminal justice, and finance.
Evidence for risk of exposure to COVID-19
COVID-19 is a new disease. A growing number of studies describe the factors that increase risk of exposure to COVID-19. Researchers have reported differences between racial and ethnic groups in the underlying factors that may increase risk of exposure. Some of the studies are from the entire United States; others are from specific cities and communities. Both types of studies consistently identify similar social factors associated with increased risk of exposure and COVID-19 illness. CDC will continue to monitor the latest evidence and provide updated information here.
Current evidence shows that the following factors are associated with increased risk of exposure to COVID-19. These factors disproportionately affect racial and ethnic minority groups:
- Neighborhood and physical environment: There is evidence that people in racial and ethnic minority groups are more likely to live in areas with high rates of new COVID-19 infections (incidence).2,6 Locally, the social factors associated with higher rates of new COVID-19 infections may vary between counties. One study found that local population-level factors related to racial and ethnic minority status, language spoken, housing, transportation, household composition and disability were associated with higher rates of new COVID-19 infections.7 These findings further support potential links between local social factors and COVID-19.
Another study found that geographic areas with higher social and economic inequities, indicating more deprived areas, had higher rates of infection compared with areas with lower social and economic inequities. Additionally, high-deprivation areas had higher proportions of Hispanic and non-White residents, persons working in manual, essential, and public-facing sectors, more crowded housing, and food and health care insecurity.6
- Housing: Crowded living conditions and unstable housing contribute to transmission of infectious diseases and can hinder COVID-19 prevention strategies like hygiene measures, self-isolation, or self-quarantine. Increasingly disproportionate unemployment rates for some racial and ethnic minority groups during the COVID-19 pandemic8 may lead to greater risk of eviction and homelessness or sharing housing. In some cultures, it is common for family members of many generations to live in one household. A previous report found that a higher percent of people from racial and ethnic minority groups lived in crowded housing (such as more than one person per room) compared to non-Hispanic White people.9 Among people with COVID-19, people in racial and ethnic minority groups were more likely to live in areas with higher population density and more housing units or inadequate housing (such as lack of indoor plumbing).10,11
COVID-19 outbreaks have been reported in settings such as correctional facilities, homeless shelters, and long-term care facilities, often referred to as shared and congregate housing. 12,13,14,15,16 Racial and ethnic minority groups are disproportionately represented in many of these settings.17,18 There are challenges in controlling the spread of COVID-19 in shared and congregate housing because of crowded, shared environments, increased potential introductions by staff members and new residents, and difficulty following distancing and hygiene measures.
- Occupation: Racial and ethnic minority groups are disproportionately represented in essential work settings such as healthcare facilities, farms, factories, warehouses, food processing, accommodation and food services, retail services, grocery stores, and public transportation.19,20,21,22 Some people who work in these settings have more chances to be exposed to COVID-19 because of several factors. These include close contact with the public or other workers, not being able to work from home, and needing to work when sick because they do not have paid sick days.23
Another study looked at differences in employment-related risk of infection by race and ethnicity to better understand racial and ethnic disparities in COVID-19-associated hospitalizations. The authors found that non-Hispanic Black adults were 60% more likely than non-Hispanic White adults to live in households with healthcare workers. The authors of the study also determined that a higher percentage of Hispanic or Latino adults (64.5%) lived in households with at least one worker who was unable to work from home (compared with 56.5% among non-Hispanic Black adults and 46.6% among non-Hispanic White adults).24
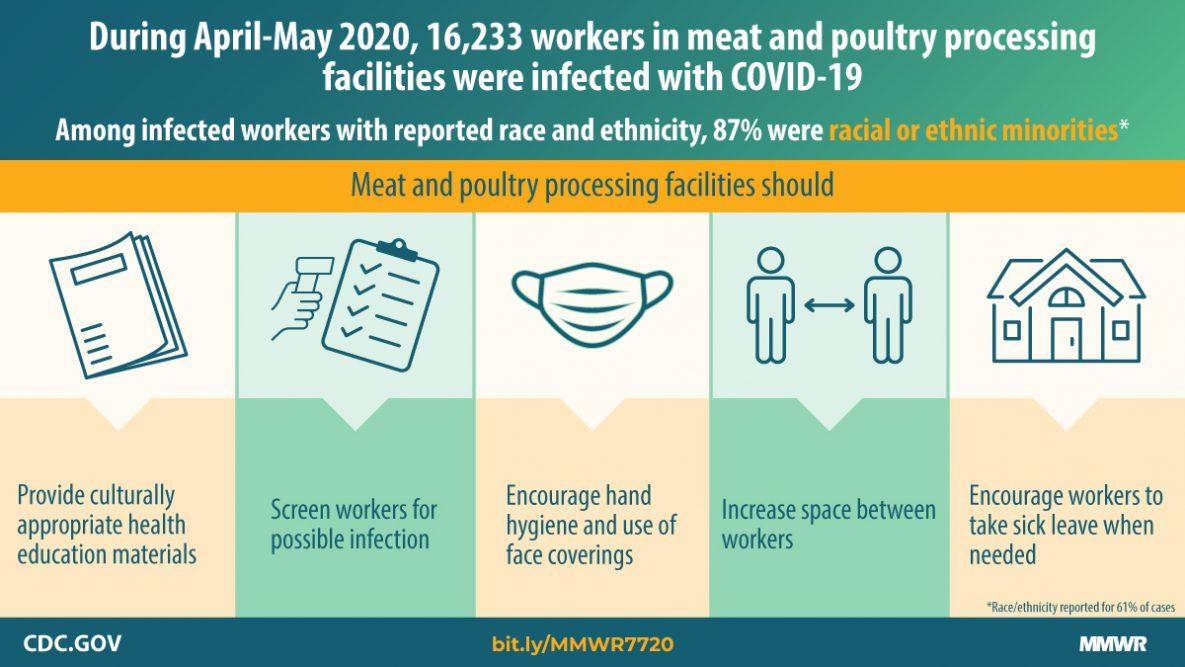
Data source: MMWR
During April-May 2020, 16,233 workers in meat and poultry processing facilities were infected with COVID-19. Among infected workers with reported race and ethnicity, 87% were racial or ethnic minorities*.
Meat and poultry processing facilities should:
- Provide culturally appropriate health education materials
- Screen workers for possible infection
- Encourage hand hygiene and use of face coverings
- Increase space between workers
- Encourage workers to take sick leave when needed
*Race/ethnicity reported for 61% of cases
- Education, income, and wealth gaps: Inequities in access to high-quality education can lead to lower high school completion rates and barriers to college entrance. This may limit future job options and lead to lower paying or less stable jobs. People with limited job options likely have less flexibility to leave jobs that may put them at higher risk of exposure to COVID-19.
Recent studies consistently found that non-Hispanic Black and Hispanic or Latino participants had lower levels of COVID-19-related knowledge about personal prevention practices, symptoms, and when to seek care, yet were more worried about and experienced more negative effects related to COVID-19.25,26,27 Additionally, one study found that among pregnant people with confirmed COVID-19, Hispanic or Latino people were more likely than non-Hispanic people to have lower incomes and public insurance.28
Access to testing
Social determinants of health may also influence access to testing. One study found that the median travel time to a COVID-19 testing site was 20 minutes in April 2020. Counties with a travel time of more than 20 minutes to a COVID-19 testing site had a higher percentage of the population that were from racial and ethnic minority groups, were uninsured, and had lower population density (were rural).29 While access to testing may have improved since April, differences in travel time may still limit access to, and use of, testing services for those who have limited access to transportation and who live in areas with fewer public transit services and schedules. Other factors that may affect both access to, and use of, testing services include lack of health insurance, concern about the costs or co-pays, occupational factors such as not being able to take time off of work and lack of paid leave, lack of accessible options for people with disabilities, and distrust of the government and healthcare systems.23,30,31,32 Delays in testing may also delay seeking care when sick as well as delays in self-isolation or implementing other mitigation measures that could reduce the spread of the virus to others.
To stop the spread of COVID-19, we need to work together to address the inequities in the social determinants of health that increase risk of exposure to COVID-19 for racial and ethnic minority groups. Learn more about what we can do to move towards health equity.
- COVID-19 Health Equity – Promoting Fair Access to Health
- CDC Social Determinants of Health: Know What Affects Health
- Environmental Public Health Tracking Network – Select “COVID-19” content area for options to view data on several factors related to increased risk of COVID-19
- CDC’s Social Vulnerability Index (SVI)
- CDC Office of Minority Health and Health Equity
- Robert Wood Johnson Foundation’s 2020 County Health Ranking State ReportsExternal
- National Association of County and City Health Officials’ COVID-19 Resources for Local Health DepartmentsExternal
- National Institute of Environmental Health Sciences COVID-19 Pandemic Vulnerability Index (PVI)
- S. House of Representatives Ways & Means Committee State and Territory Health Equity MapsExternal
- Price-Haygood EG, Burton J, et al. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. N Engl J Med. 2020. DOI: https://doi.org/10.1056/NEJMsa2011686External
- Millet GA, Jones AT, Benkeser D, et al. Assessing Differential Impacts of COVID-19 on Black Communities. Ann Epidemiol. 2020;47:37-44. DOI: https://doi.org/10.1016/j.annepidem.2020.05.003External.
- Paradies Y. A Systematic Review of Empirical Research on Self-reported Racism and Health. Int J Epidemiol. 2006; 35(4):888–901. DOI: https://doi.org/10.1093/ije/dyl056External.
- Simons RL, Lei MK, Beach SRH, et al. Discrimination, Segregation, and Chronic Inflammation: Testing the Weathering Explanation for the Poor Health of Black Americans. Dev Psychol. 2018;54(10):1993-2006. DOI: https://doi.org/10.1037/dev0000511External
- Cordes J, Castro MC. Spatial Analysis of COVID-19 Clusters and Contextual Factors in New York City. Spat Spatiotemporal Epidemiol. 2020;34:100355. DOI: https://dx.doi.org/10.1016%2Fj.sste.2020.100355External.
- Lewis NM, Friedrichs M, Wagstaff S, et al. Disparities in COVID-19 Incidence, Hospitalizations, and Testing, by Area-Level Deprivation – Utah, March 3 – July 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1369-1373. DOI: http://dx.doi.org/10.15585/mmwr.mm6938a4External.
- Karaye IM, Horney JA. The Impact of Social Vulnerability on COVID-19 in the U.S.: An Analysis of Spatially Varying Relationships. Am J Prev Med. 2020;59(3):217-325. DOI: https://doi.org/10.1016/j.amepre.2020.06.006External
- Galea S, Abdalla SM. COVID-19 Pandemic, Unemployment, and Civil Unrest: Underlying Deep Racial and Socioeconomic Divides. JAMA. 2020 Jul 21;324(3):227-228. DOI: https://doi.org/10.1001/jama.2020.11132External.
- U.S. Department of Housing and Urban Development Office of Policy Development and Research. Measuring Overcrowding in Housing. 2007 [cited 2020 Aug 29]. Available from URL: https://www.census.gov/content/dam/Census/programs-surveys/ahs/publications/Measuring_Overcrowding_in_Hsg.pdfPdfExternal.
- Okoh AK, Sossou C, Dangayach NS, et al. Coronavirus Disease 19 in Minority Populations of Newark, New Jersey. International Journal for Equity in Health. 2020;19:93. DOI: https://doi.org/10.1186/s12939-020-01208-1External.
- Rodriguez-Lonear D, Barcelo NE, Akee R, Carroll SR. American Indian Reservations and COVID-19: Correlates of Early Infection Rates in the Pandemic. J of Public Health Management and Practice. 2020;24(4):371-377. DOI: https://doi.org/10.1097/PHH.0000000000001206External
- Wallace M, Hagan L, Curran KG. COVID-19 in Correctional and Detention Facilities – United States, February-April 2020. MMWR Morb Mortal Wkly Rep 2020;69:587–590. DOI: http://dx.doi.org/10.15585/mmwr.mm6919e1External.
- Wallace M, Marlow M, Simonson S, et al. Public Health Response to COVID-19 Cases in Correctional and Detention Facilities — Louisiana, March–April 2020. MMWR Morb Mortal Wkly Rep 2020;69:594–598. DOI: http://dx.doi.org/10.15585/mmwr.mm6919e3External.
- Jiminez MC, Cowger TL, Simon LE, et al. Epidemiology of COVID-19 among Incarcerated Individuals and Staff in Massachusetts Jails and Prisons. JAMA Open Network. 2020;3(8):e2018851. DOI: https://doi.org/10.1001/jamanetworkopen.2020.18851External.
- Tobolowsky FA, Gonzales E, Self JL, et al. COVID-19 Outbreak Among Three Affiliated Homeless Service Sites — King County, Washington, 2020. MMWR Morb Mortal Wkly Rep 2020;69:523–526. DOI: http://dx.doi.org/10.15585/mmwr.mm6917e2External.
- McMichael TM, Clark S, Pogosjans S, et al. COVID-19 in a Long-Term Care Facility — King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:339-342. DOI: http://dx.doi.org/10.15585/mmwr.mm6912e1External.
- Federal Bureau of Prisons. Statistics [online]. 2020 [cited 2020 Aug 27]. Available from URL: https://www.bop.gov/about/statistics/External.
- US Department of Housing and Urban Development. The 2019 Annual Homeless Assessment Report (AHAR) to Congress [online]. 2020 [cited 2020 Aug 27]. Available from URL: https://www.huduser.gov/portal/sites/default/files/pdf/2019-AHAR-Part-1.pdfPdfExternal. Last accessed 8/22/2020.
- U.S. Bureau of Labor Statistics. Labor Force Characteristics by Race and Ethnicity, 2018 [online]. 2019 [cited 2020 Jun 24]. Available from URL: https://www.bls.gov/opub/reports/race-and-ethnicity/2018/home.htmExternal
- Hawkins D. Differential Occupational Risk for COVID-19 and Other Infection Exposure According to Race and Ethnicity. Am J Ind Med. 2020;1-4. DOI: https://doi.org/10.1002/ajim.23145External.
- Waltenburg MA, Victorroff T, Rose CE, et al. Update: COVID-19 Among Workers in Meat and Poultry Processing Facilities – United States, April-May 2020. MMWR;69(27):887-892. DOI: http://dx.doi.org/10.15585/mmwr.mm6927e2External.
- Bui DP, McCaffrey K, Friedrichs M, et al. Racial and Ethnic Disparities among COVID-19 Cases in Workplace Outbreaks by Industry Sector – Utah, March 6 – June 5, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(33):1133-1138. DOI: http://dx.doi.org/10.15585/mmwr.mm6933e3External.
- Economic Policy Institute. Black Workers Face Two of the Most Lethal Preexisting Conditions for Coronavirus—Racism and Economic Inequality [online]. 2020 [cited 2020 Jun 28]. Available from URL: https://www.epi.org/publication/black-workers-covid/External
- Selden TM, Berdahl TA. COVID-19 And Racial/Ethnic Disparities in Health Risk, Employment, and Household Composition. Health Affairs. 2020: DOI: https://doi.org/10.1377/hlthaff.2020.00897External.
- Alobuia WM, Dalva-Baird NP, Forrester JD, et al. Racial Disparities in Knowledge, Attitudes and Practices Related to COVID-19 in the USA. J Public Health. 2020;03:1-9. DOI: https://doi.org/10.1093/pubmed/fdaa069External
- Alsan M, Stantcheva S, Yang D, Cutler D. Disparities in Coronavirus 2019 Reported Incidence, Knowledge, and Behavior among US Adults. JAMA Network Open. 2020;3(6):e2012403. DOI: https://doi.org/10.1001/jamanetworkopen.2020.12403External.
- Jones J. Sullivan PS, Sanchez TH, et al. Similarities and Differences in COVID-19 Awareness, Concern, and Symptoms by Race and Ethnicity in the United States: Cross-sectional Survey. J of Med Internet Res. 2020;22(7):e20001 DOI: https://doi.org/10.2196/20001External.
- Goldfard IT, Clapp MA, Soffer MD, et al. Prevalence and Severity of Coronavirus Disease 2019 (COVID-19) Illness in Symptomatic Pregnant and Postpartum Women Stratified by Hispanic Ethnicity. Obstetrics & Gynecology. 2020;136(2). DOI: https://doi.org/10.1097/AOG.0000000000004005External.
- Rader B, Astley CM, Therese K, et al. Geographic Access to United States SARS-CoV-2 Testing Sites Highlights Healthcare Disparities and May Bias Transmission. Journal of Travel Medicine. 2020. https://doi.org/10.1093/jtm/taaa076External
- Berchick, Edward R., Jessica C. Barnett, and Rachel D. Upton Current Population Reports, P60-267(RV), Health Insurance Coverage in the United States: 2018, S. Government Printing Office, Washington, DC, 2019.
- Institute of Medicine (US) Committee on the Consequences of Uninsurance. Care Without Coverage: Too Little, Too Late. Washington (DC): National Academies Press (US); 2002 [cited 2020 Aug 27]. DOI: https://doi.org/10.17226/10367External.
- Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press. DOI: https://doi.org/10.17226/10260External.