Recommendations for Fully Vaccinated People
COVID-19 Homepage
Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19: Information for Healthcare Professionals
What You Need to Know
- An updated list of high-risk underlying conditions, along with their associated evidence, is provided below. The conditions are grouped by the level of evidence, with the highest level shown in the top section.
- The list of underlying medical conditions is not exhaustive and will be updated as the science evolves. CDC continually reviews additional underlying conditions, and some of these might have sufficient evidence to be added to the list.
- This list should not be used to exclude people with underlying conditions from recommended measures for prevention or treatment of COVID-19.
- The process used to update the list is found on CDC’s Systematic Review Process page.
This webpage provides an evidence-based resource for healthcare professionals caring for patients with underlying medical conditions who are at higher risk of experiencing severe outcomes of COVID-19. Severe outcomes of COVID-19 are defined as hospitalization, admission to the intensive care unit (ICU), intubation or mechanical ventilation, or death.
This page summarizes data from published reports, scientific articles in press, unreviewed pre-prints, and internal data that were included in literature reviews conducted by subject matter experts. Evidence used to inform the list of underlying conditions was determined by CDC reviewers based on available literature about COVID-19 at time of review. The information reflects evidence regarding underlying medical conditions and is intended to help healthcare professionals make informed decisions about patient care and to increase the awareness of risk among their patients.
The methods used to assess the conditions have changed during the pandemic as the amount of literature and types of studies increased. For instance, preliminary versions of this list focused on providing the latest information based on descriptive data. As the literature grew, CDC investigators categorized the literature by study design.
Since May 2021, the process has been updated to include a CDC-led review process that uses rigorous systematic review methods. To learn more about the process of CDC’s systematic reviews, see CDC systematic review process.
Background
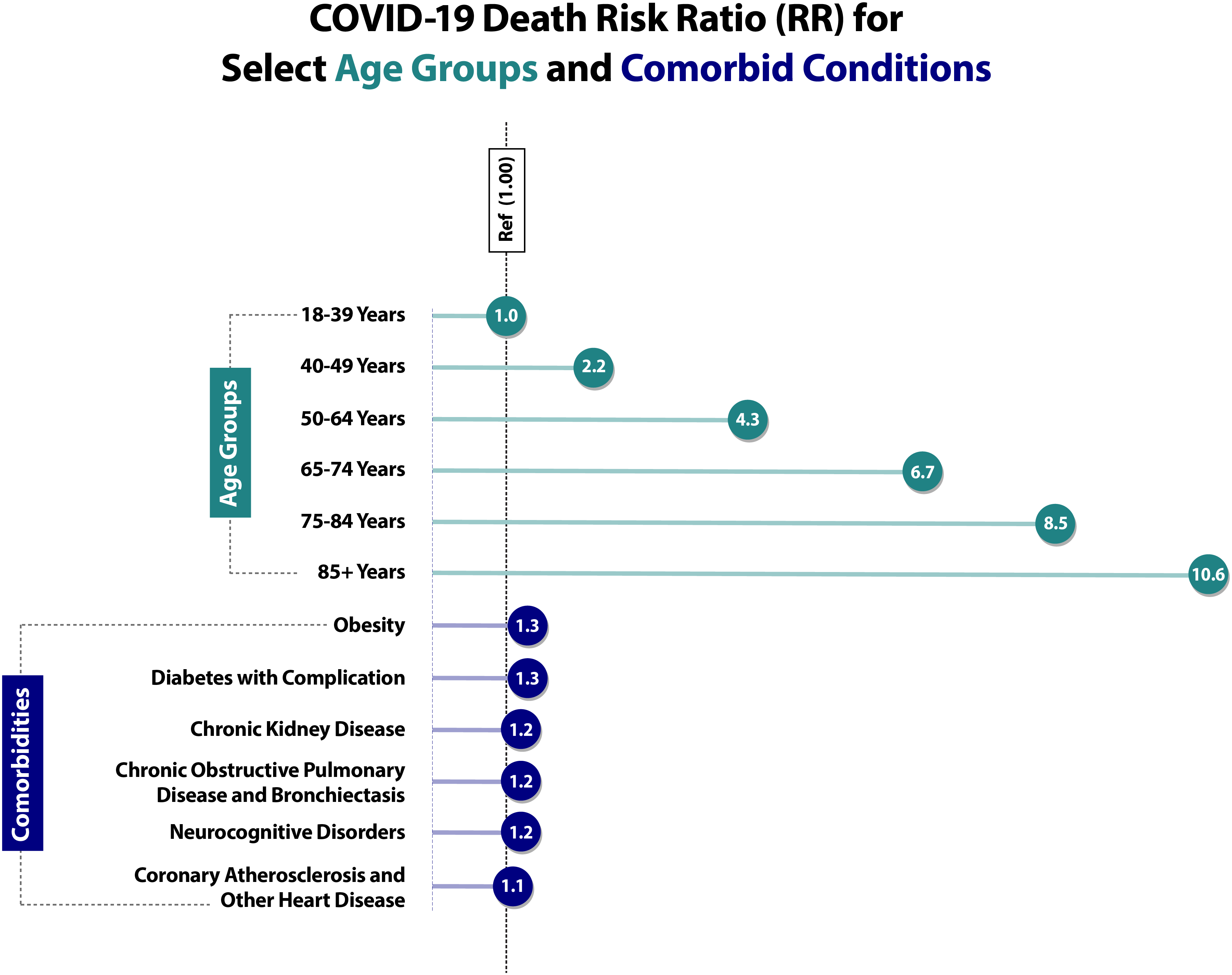
Age is the strongest risk factor for severe COVID-19 outcomes. Patients with one or multiple of certain underlying medical conditions are also at higher risk.(1–3)
Additionally, being unvaccinated or not being up to date on COVID-19 vaccinations also increases the risk of severe COVID-19 outcomes.
Providers should consider the patient’s age, presence of underlying medical conditions and other risk factors, and vaccination status in determining the risk of severe COVID-19-associated outcomes for any patient.
Demographic Factors
Studies have shown that COVID-19 does not affect all population groups equally. Three important factors are age, race, and ethnicity.
Age
Age remains the strongest risk factor for severe COVID-19 outcomes, with risk of severe outcomes increasing markedly with increasing age. Based on data from the National Vital Statistics System (NVSS) at NCHS (Risk for COVID-19 Infection, Hospitalization, and Death By Age Group), compared with ages 18–29 years, the risk of death is 25 times higher in those ages 50–64 years, 60 times higher in those ages 65–74 years, 140 times higher in those ages 75–84 years, and 340 times higher in those ages 85+ years. Notably, these data include all deaths in the United States that occurred throughout the pandemic, from February 2020 to July 1, 2022, including deaths among unvaccinated individuals.
Risk of severe outcomes is increased in people of all ages with certain underlying medical conditions and in people who are 50 years and older, with risk increasing substantially at ages >65 years.4,5 Residents of long-term care facilities are also at increased risk, making up less than 1% of the U.S. population but accounting for more than 35% of all COVID-19 deaths.6-10
Race and Ethnicity
The COVID-19 pandemic has highlighted racial, ethnic, and socioeconomic disparities in COVID-19 illnesses, hospitalizations, and deaths.11-13 Some racial and ethnic minority groups are also more likely to face multiple barriers to accessing health care including lack of insurance, transportation, child care, or ability to take time off from work.
Estimates of COVID-19 deaths in the U.S. show that people from racial and ethnic minority groups are dying from COVID-19 disproportionately, and studies have identified racial and ethnic differences in at-home COVID-19 test use, vaccination coverage, and access to outpatient therapeutics.14-16 Data has shown that compared to non-Hispanic White people, people from racial and ethnic minority groups are more likely to be infected with SARS-CoV-2 (the virus that causes COVID-19). Once infected, people from racial and ethnic minority groups are more likely to be hospitalized, be admitted to the ICU, and die from COVID-19 at younger ages.17
We are still learning about how the environments where people live, learn, and work can influence the risk for infection and severe COVID-19 outcomes.
Summary of Conditions with Evidence
Evidence used to inform the list of underlying medical conditions that increase a person’s risk of severe illness from COVID-19 is presented in alphabetical order by study design section. Conditions are categorized as higher risk, suggestive higher risk, and mixed evidence.
Higher Risk (conclusive)
Higher risk is defined as an underlying medical condition or risk factor that has a published meta-analysis or systematic review or underwent the CDC systematic review process. The meta-analysis or systematic review demonstrates a conclusive increase in risk for at least one severe COVID-19 outcome.
Condition
Condition
Evidence of Impact on COVID-19 Severity [Reference number]
Evidence of Impact on COVID-19 Severity [Reference number]
Asthma
Asthma
CDC Systematic Review [K]
CDC Systematic Review [K]
Cancer
- Hematologic Malignancies
Cancer
- Hematologic Malignancies
CDC Systematic Review [O]
Meta-Analysis/ Systematic Review 18-22
Cohort Study 23-25
Case Series 26-28
Case Control Study 29
CDC Systematic Review [O]
Meta-Analysis/ Systematic Review 18-22
Cohort Study 23-25
Case Series 26-28
Case Control Study 29
Cerebrovascular disease
Cerebrovascular disease
Meta-Analysis 30-33
Synthesis of Evidence 34
Cohort Study 35-37
Meta-Analysis 30-33
Synthesis of Evidence 34
Cohort Study 35-37
Chronic kidney disease*
- People receiving dialysis 38,39 ^
Chronic kidney disease*
- People receiving dialysis 38,39 ^
Meta-Analysis 33,40
Cohort Studies 36,41-62, 63*
Case Series 64-66
Meta-Analysis 33,40
Cohort Studies 36,41-62, 63*
Case Series 64-66
Chronic lung diseases limited to:
- Bronchiectasis
- COPD (Chronic obstructive pulmonary disease)
- Interstitial lung disease
- Pulmonary embolism
- Pulmonary hypertension
Chronic lung diseases limited to:
- Bronchiectasis
- COPD (Chronic obstructive pulmonary disease)
- Interstitial lung disease
- Pulmonary embolism
- Pulmonary hypertension
- CDC Systematic Review [A]
- CDC Systematic Review [L]
- CDC Systematic Review [D]
- CDC Systematic Review [G]
- CDC Systematic Review [G]
- CDC Systematic Review [A]
- CDC Systematic Review [L]
- CDC Systematic Review [D]
- CDC Systematic Review [G]
- CDC Systematic Review [G]
Chronic liver diseases limited to:
- Cirrhosis
- Non-alcoholic fatty liver disease
- Alcoholic liver disease
- Autoimmune hepatitis
Chronic liver diseases limited to:
- Cirrhosis
- Non-alcoholic fatty liver disease
- Alcoholic liver disease
- Autoimmune hepatitis
CDC Systematic Review [B]
CDC Systematic Review [B]
Cystic fibrosis
Cystic fibrosis
CDC Systematic Review [M]
CDC Systematic Review [M]
Diabetes mellitus, type 1
Diabetes mellitus, type 1
Meta-Analysis 67
Case Series 65
Cohort Study 35,68-73
Meta-Analysis 67
Case Series 65
Cohort Study 35,68-73
Diabetes mellitus, type 2*
Diabetes mellitus, type 2*
Meta-Analysis 74
Systematic Review 75*
Gestational Diabetes Systematic Review 76*
Case Series 65
Longitudinal Study 77
Cohort Study 67,71,77-82
Meta-Analysis 74
Systematic Review 75*
Gestational Diabetes Systematic Review 76*
Case Series 65
Longitudinal Study 77
Cohort Study 67,71,77-82
Disabilities‡, including Down syndrome
For the list of all conditions that were part of the review, see the module below
Disabilities‡, including Down syndrome
For the list of all conditions that were part of the review, see the module below
CDC Systematic Review [C]
CDC Systematic Review [C]
Heart conditions (such as heart failure, coronary artery disease, or cardiomyopathies)
Heart conditions (such as heart failure, coronary artery disease, or cardiomyopathies)
Meta-Analysis 83-85
Cohort Study 35,36
Meta-Analysis 83-85
Cohort Study 35,36
HIV (Human immunodeficiency virus)
HIV (Human immunodeficiency virus)
Meta-Analysis/ Systematic Review 86
Cohort Study 54,87-89
Case Series 90-92
Meta-Analysis/ Systematic Review 86
Cohort Study 54,87-89
Case Series 90-92
Mental health conditions limited to:
- Mood disorders, including depression
- Schizophrenia spectrum disorders
Mental health conditions limited to:
- Mood disorders, including depression
- Schizophrenia spectrum disorders
Meta-Analysis/ Systematic Review 93,94
Meta-Analysis/ Systematic Review 93,94
Neurologic conditions limited to dementia‡
Neurologic conditions limited to dementia‡
Meta-Analysis/ Systematic Review 95-98
Cross-Sectional Study 99
Cohort Study 36,100
Meta-Analysis/ Systematic Review 95-98
Cross-Sectional Study 99
Cohort Study 36,100
Obesity (BMI >30 kg/m2 or >95th percentile in children)
Obesity (BMI >30 kg/m2 or >95th percentile in children)
Meta-Analysis 101-103
Systematic Review 75*
Cohort 46,104-112; 63,113-116*
Meta-Analysis 101-103
Systematic Review 75*
Cohort 46,104-112; 63,113-116*
Physical inactivity
Physical inactivity
CDC Systematic Review [E]
CDC Systematic Review [E]
Pregnancy and recent pregnancy
Pregnancy and recent pregnancy
Meta-Analysis/ Systematic Review 75,117
Case Control 118,119
Case Series 120-122
Cohort Study 123-126
Meta-Analysis/ Systematic Review 75,117
Case Control 118,119
Case Series 120-122
Cohort Study 123-126
Primary immunodeficiencies
Primary immunodeficiencies
CDC Systematic Review [F]
CDC Systematic Review [F]
Smoking, current and former
Smoking, current and former
Meta-Analysis 83,127,128-135
Meta-Analysis 83,127,128-135
Solid organ or blood stem cell transplantation
Solid organ or blood stem cell transplantation
Meta-Analysis 108
Case Series 136-147
Cohort 148-151
Meta-Analysis 108
Case Series 136-147
Cohort 148-151
Tuberculosis
Tuberculosis
CDC Systematic Review [H]
CDC Systematic Review [H]
Use of corticosteroids or other immunosuppressive medications
Use of corticosteroids or other immunosuppressive medications
Meta-Analysis/ Systematic Review 152
Cohort Study 153
Cross-Sectional 154
Case Series 155-157
Meta-Analysis/ Systematic Review 152
Cohort Study 153
Cross-Sectional 154
Case Series 155-157
Suggestive Higher Risk
Suggestive higher risk is defined as an underlying medical condition or risk factor that did not have a published meta-analysis or systematic review or did not undergo the CDC systematic review process. The evidence is supported by mostly cohort, case-control, or cross-sectional studies. (Systematic reviews are available for some conditions for children with underlying conditions.)
Condition
Condition
Evidence of Impact on COVID-19 Severity [Reference number]
Evidence of Impact on COVID-19 Severity [Reference number]
Children with certain underlying conditions
Children with certain underlying conditions
Systematic Review 158,159
Cross-Sectional Study 99,160,161
Cohort Study 100,162-169
Case Series 170,171
Systematic Review 158,159
Cross-Sectional Study 99,160,161
Cohort Study 100,162-169
Case Series 170,171
Overweight (BMI >25 kg/m2 but <30 kg/m2)
Overweight (BMI >25 kg/m2 but <30 kg/m2)
Cohort Study111
Case Series110
Cohort Study111
Case Series110
Sickle cell disease
Sickle cell disease
Cohort170-173
Case Series 170,173-188
Cohort170-173
Case Series 170,173-188
Substance use disorders
Substance use disorders
Case-Control Study 189-191
Cohort Study 192,193
Case-Control Study 189-191
Cohort Study 192,193
Mixed Evidence (inconclusive: no conclusions can be drawn from the evidence)
Mixed evidence is defined as an underlying medical condition or risk factor that has a published meta-analysis or systematic review or underwent the CDC systematic review process. The meta-analysis or systematic review is inconclusive, either because the aggregated data on the association between an underlying condition and severe COVID-19 outcomes are inconsistent in direction or there are insufficient (or limited) data on the association between an underlying condition and severe COVID-19 outcomes.
- Limited: The evidence consists of one study, or several small studies with no comparison group, limiting the conclusions that can be drawn.
- Inconsistent: The evidence suggests no clear direction of association, meaning no firm conclusions can be drawn.
Condition
Condition
Evidence of Impact on COVID-19 Severity [Reference number]
Evidence of Impact on COVID-19 Severity [Reference number]
Alpha 1 antitrypsin deficiency
Alpha 1 antitrypsin deficiency
Limited: CDC Systematic Review [I]
Limited: CDC Systematic Review [I]
Bronchopulmonary dysplasia
Bronchopulmonary dysplasia
Limited: CDC Systematic Review [J]
Limited: CDC Systematic Review [J]
Hepatitis B
Hepatitis B
Inconsistent: CDC Systematic Review [B]
Inconsistent: CDC Systematic Review [B]
Hepatitis C
Hepatitis C
Limited: CDC Systematic Review [B]
Limited: CDC Systematic Review [B]
Hypertension*
Hypertension*
Inconsistent
Meta-Analysis 83,194-197
Systematic Review 198, 75*
Cohort Study 35,36,41,199-205
Case Series 206
Inconsistent
Meta-Analysis 83,194-197
Systematic Review 198, 75*
Cohort Study 35,36,41,199-205
Case Series 206
Thalassemia
Thalassemia
Limited: CDC Systematic Review [N]
Limited: CDC Systematic Review [N]
Footnotes:
* Indicates presence of evidence for pregnant and non-pregnant people
‡ Underlying conditions for which there is evidence in pediatric patients
^ Risk may be further increased for people receiving dialysis
Actions Healthcare Professionals Can Take
- Support vaccination with approved and authorized COVID-19 vaccines (primary series and boosters), which are safe and effective. Check out the Interim Clinical Considerations for Use of COVID-19 Vaccines as well as Stay Up to Date with your Vaccines and locations for COVID-19 vaccination for patients for more information.
- Consider therapies, such as antivirals, when treating patients with mild to moderate illness and risk factors for severe illness. These therapeutics have been shown to significantly decrease the risk of hospitalization and death, and outcomes are improved if therapeutics are started within the first days of illness.
- Encourage patients to keep appointments for routine care and adhere to treatment regimens for their medical conditions.
- Consider use of telehealth when appropriate.
- Encourage patients with underlying medical conditions, who are able to, to continue practicing preventive measures such as wearing a high-quality mask in order to decrease the risk of infection with the virus that causes COVID-19. This becomes even more important with increasing age and number and severity of underlying conditions.
- Check out additional information for your patients.
- EVUSHELDTM, a monoclonal antibody combination that was used for pre-exposure prophylaxis to protect against SARS-CoV-2 infection, is not currently authorized for emergency use in the United States because it is unlikely to be active against certain SARS-CoV-2 variants. According to the most recent CDC Nowcast data, these variants are projected to be responsible for more than 90% of current infections in the U.S. This means that EVUSHELDTM is not expected to provide protection against developing COVID-19 if exposed to those variants. Healthcare facilities and providers with EVUSHELDTM should retain all products in the event that SARS-CoV-2 variants that are neutralized by EVUSHELDTM become more prevalent in the U.S. in the future. For more information, see FDA’s announcement.
Considerations for Patients Within Racial and Ethnic Minority Groups
- Ask patients about their concerns about vaccines and therapy. Consider using an evidence-based and culturally sensitive approach, such as motivational interviewing. Try to provide trusted sources of information and other resources.
- Encourage testing, as well as early treatment, for patients who are eligible.
- Facilitate access to culturally and linguistically appropriate resources.
- Reduce barriers to accessing current outpatient treatments.
CDC strongly encourages healthcare professionals, patients and their advocates, and health system administrators to regularly consult the National Institutes of Health (NIH) COVID-19 Treatment Guidelines.
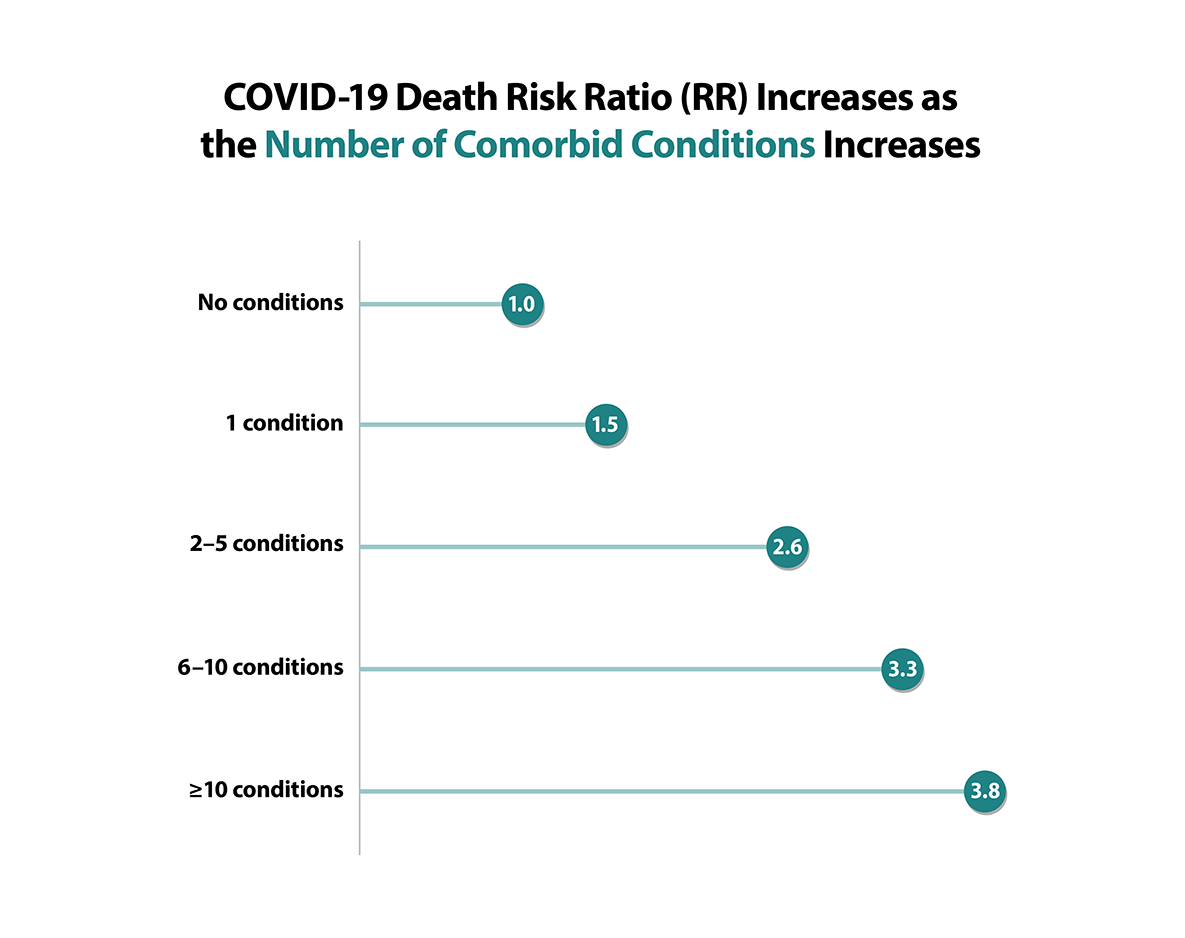
Key Findings from One Large Cross-Sectional Study
Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, March 2020–March 2021
This study used data from the Premier Healthcare Database, which represents approximately 20% of all inpatient admissions in the United States since 2000. This cross-sectional study of 540,667 adults hospitalized with COVID-19 included both inpatients and hospital-based outpatients with laboratory-diagnosed COVID-19 from March 1, 2020, through March 31, 2021. The database included reports from 592 acute care hospitals in the United States. The study was designed to examine risk factors associated with severe outcomes of COVID-19 including admission to an ICU or stepdown unit, invasive mechanical ventilation, and death.
Main Findings:
- Certain underlying medical conditions were associated with an increased risk for severe COVID-19 illness in adults.
- Having multiple conditions was also associated with severe COVID-19 illness.
- Obesity, diabetes with complications, and anxiety and fear-related disorders had the strongest association with death.
- The number of frequent underlying medical conditions (present in ≥10.0% of patients) increased with age.207
Adapted from Sources:
- Kompaniyets L, Pennington AF, Goodman AB, Rosenblum HG, Belay B, Ko JY, et al. Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, March 2020–March 2021. To learn more, visit the Preventing Chronic Disease article: https://www.cdc.gov/pcd/issues/2021/21_0123.htm
- Pennington AF, Kompaniyets L, Summers AD, Danielson ML, Goodman AB, Chevinsky JR, Preston LE, Schieber LZ, Namulanda G, Courtney J, Strosnider HM, Boehmer TB, Mac Kenzie WR, Baggs J, Gundlapalli AV, Risk of Clinical Severity by Age and Race/Ethnicity Among Adults Hospitalized for COVID-19—United States, March–September 2020, Open Forum Infectious Diseases, Volume 8, Issue 2, February 2021. To learn more, visit: https://doi.org/10.1093/ofid/ofaa638
Source: Kompaniyets L, Pennington AF, Goodman AB, Rosenblum HG, Belay B, Ko JY, et al. Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, March 2020–March 2021. To learn more, visit the Preventing Chronic Disease article: https://www.cdc.gov/pcd/issues/2021/21_0123.htm