Operational Considerations for the Identification of Healthcare Workers and Inpatients with Suspected COVID-19 in non-U.S. Healthcare Settings
The U.S. Centers for Disease Control and Prevention (CDC) is working closely with international partners to respond to the coronavirus disease 2019 (COVID-19) pandemic. CDC provides technical assistance to help other countries increase their ability to prevent, detect, and respond to health threats, including COVID-19.
This document is provided by CDC and is intended for use in non-US healthcare settings.
Summary of Recent Changes
Key Points
- This guidance is for non-US healthcare facilities to identify healthcare workers and inpatients with Suspected COVID-19.
- Different surveillance strategies are provided along with considerations for each strategy.
1. Overview
This document provides guidance on the identification or screening of healthcare workers1 and inpatients with symptoms of suspected COVID-19. Rational, requirements, and considerations will be discussed for three broad case identification strategies:
- Passive strategies: Reporting/alerts are initiated by the data source (e.g., healthcare worker or treating clinician) based on a known set of rules or regulations.
- Enhanced passive strategies: Reporting/alerts are initiated by the data source with an added mechanism to prompt data collection, review, and reporting.
- Active strategies: Reporting/alerts are initiated by the centralized health authority (e.g., Ministry of Health, facility infection preventionist, facility administration) using a known set of rules or regulations.
Additional guidance on managing visitors to healthcare facilities, triage of suspected COVID-19 patients, and management of healthcare workers exposed to or with suspected or confirmed COVID-19 in non-US healthcare settings are also available.
While, epidemiologic, virologic, and modeling reports support the possibility of transmission of SARS-CoV-2, the virus that causes COVID-19, transmission from people who are presymptomatic (SARS-CoV-2 detected before symptom onset) or asymptomatic (SARS-CoV-2 detected but symptoms never develop), critical knowledge gaps remain regarding the benefit of routine or repeated screening of healthcare workers and inpatients without symptoms for prevention of COVID-19 spread within health facilities outside of an outbreak response scenario.2 Therefore, discussion around optimal testing strategies for the identification of healthcare workers with presymptomatic and asymptomatic SARS-CoV-2 infection are outside the scope of this guidance.
2. Signs and Symptoms Consistent with COVID-19
Presenting signs and symptoms of COVID-19 vary, limiting the definition of a generalizable set of characteristic signs and symptoms for COVID-19. At best, current evidence suggests substantial variability ranging from mild to severe and based on only partially described patient-level factors. The WHO interim guidance for clinical management of COVID-19 provides a summary of published COVID-19 symptom descriptions and observed frequency.
Among persons who develop symptoms, most experience fever (83%–99%), cough (59%–82%), fatigue (44%–70%), anorexia (40%–84%), shortness of breath (31%–40%), and myalgias (11%–35%). Other non-specific symptoms, such as sore throat, nasal congestion, headache, diarrhea, nausea, and vomiting, have also been reported. Loss of smell (anosmia) or loss of taste (ageusia) preceding the onset of respiratory symptoms has also been reported.
Older people and immunosuppressed patients in particular may present with atypical symptoms such as fatigue, reduced alertness, reduced mobility, diarrhea, loss of appetite, delirium, and absence of fever.
Symptoms such as dyspnea, fever, gastrointestinal (GI) symptoms or fatigue due to physiologic adaptations in pregnant women, adverse pregnancy events, or other diseases such as malaria, may overlap with symptoms of COVID-19.
Children might not have reported fever or cough as frequently as adults.
Given the variability in COVID-19 symptoms, facilities should define a standardized set of signs and symptoms (e.g., fever and/or cough/shortness of breath) to screen healthcare workers and patients for suspected COVID-19. A is critical to ensure cases do not go unrecognized due to a substantial proportion of patients and healthcare workers presenting with atypical or minimal symptoms.
3. General Best Practices
In addition to a specific strategy for the identification of suspected COVID-19 cases, there are general best practices that will improve both healthcare worker and inpatient COVID-19 screening. Some examples include:
Considerations on COVID-19 Vaccination
- To protect vital healthcare infrastructure, many countries have prioritized the vaccination of healthcare workers.
- Because COVID-19 vaccination is not 100% effective against symptomatic disease and vaccination coverage within the larger population is often incomplete, efforts to identify healthcare workers and inpatients with COVID-19 remain of value in most healthcare facilities.
Monitor and Manage Ill and Exposed Healthcare Workers
- Facilities and organizations providing healthcare should implement sick leave policies for healthcare workers that are non-punitive, flexible, and consistent with public health guidance.
- Movement and monitoring decisions for healthcare workers with exposure to COVID-19 should be made in consultation with public health. Operational considerations for the management of healthcare workers exposed to COVID-19 in non-US healthcare settings are available.
Train and Educate Healthcare Workers
- Provide healthcare workers with job- or task-specific education and training on identifying and preventing transmission of infectious agents, including refresher training.
- Ensure that healthcare workers are educated, trained, and have practiced the appropriate use of personal protective equipment (PPE) prior to caring for a patient.
- Provide job-aids and up-to-date reference materials.
- Encourage and support a high index of suspicion in healthcare workers regarding suspect COVID-19 cases.
Establish Reporting Within and Between Healthcare Facilities and to Public Health Authorities
- Implement mechanisms and policies that promote situational awareness for facility staff about confirmed or suspected COVID-19 patients and facility plans for response, including:
- Infection control
- Healthcare epidemiology
- Facility leadership
- Occupational health
- Clinical laboratory
- Frontline staff
- Communicate and collaborate with public health authorities.
- Communicate information about confirmed or suspected COVID-19 patients to appropriate personnel before transferring to other departments in the facility and to other healthcare facilities.
4. Surveillance Capacities
Facility-based surveillance for healthcare-associated infections (HAIs), including infections in healthcare workers and inpatients, is one of the WHO’s eight core components of infection prevention and control (IPC). While surveillance is a critical component of providing safe healthcare, it is important to recognize that it requires expertise, good quality data, and an established IPC program and thus, may require time to set up. For this reason, during public health emergency response, healthcare facilities are encouraged to initially implement facility-based, suspect COVID-19 patient case finding (surveillance) that is feasible with existing surveillance capacities.
Health facility surveillance capacity varies greatly even within health systems. A realistic appraisal of capacity can help identify the best strategy for a given context. A general description of surveillance capacities based on existing HAI surveillance activity is provided for guidance.
| Surveillance capacity | Standardized HAI case definitions / methods | Dedicated surveillance staff3 | Patient-level data available / accessible |
|---|---|---|---|
| High: Resources needed for detailed patient interviews and/or chart reviews are readily available | YES | YES | YES |
| Medium: Some experience with standardized data collection with limitation in staff and data availability | YES | PARTIAL | PARTIAL |
| Low to Very Low: Little to no experience with patient-level collection of standardized data, limited availability of staff and data for reassignment for case finding activities | PARTIAL | NO | NO |
5. Identification of Healthcare Workers with Suspected COVID-19
Objective: Prevent exposure of at-risk patients and staff to symptomatic COVID-19 positive healthcare workers.

Figure: Passive identification of healthcare workers with suspected COVID-19
Passive Strategy
All healthcare workers self-assess for fever and/or a defined set of newly present symptoms indicative of COVID-19. If fever or respiratory symptoms are present, healthcare workers:
- Should remotely report this information4,
- Should not go to their health facility, and
- Should be provided with immediate medical assessment and follow-up actions.
Rationale:
Establishes procedures for the identification of healthcare workers at increased likelihood of infection with minimal resource requirements.
Requirements:
- List of symptoms and thermometer for self-assessment.
- Staff and mechanism (e.g., telephone line) for remote reporting of temperature/fever and/or presence of symptoms consistent with COVID-19. Ideally this system is always available for quick medical assessment. If reporting system is not available, symptomatic healthcare workers should not report to their facility until they can be evaluated.
- Decision algorithms for response to healthcare worker reports and the results of secondary assessment.
- Standardized medical assessment forms and movement and monitoring forms..
Considerations:
- Adherence is highly dependent on healthcare worker motivation and appropriate self-assessment of risk.
- Can result in reduction in work force, particularly among some critical staffing categories.
- COVID-19 vaccination status can be an additional consideration in response to symptom reports. However, healthcare workers with fever and/or respiratory symptoms should be tested and excluded from work regardless of COVID-19 vaccination status.
- Provision of paid sick leave/compensation for all healthcare workers not allowed to work is often critical for success, requiring substantial resources.
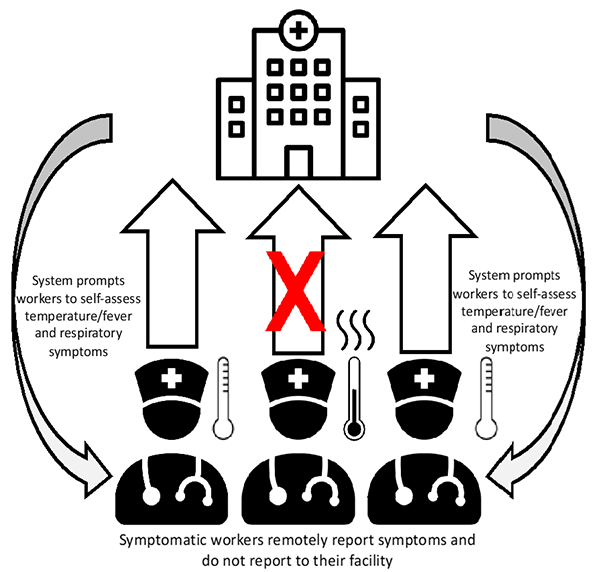
Figure: Enhanced passive identification of healthcare workers with suspected COVID-19
Enhanced Passive Strategy
Supplements a passive strategy with a plan to remind or prompt workers to self-assess for symptoms consistent with COVID-19. Common reminders include automated text messages or phone calls.
Rationale:
Evidence suggests that simple automatic reminders can increase adherence.
Requirements:
- All requirements of Passive Strategy
- Automated (e.g., mass texting service) or manual system (e.g., direct messaging or phone calls) to contact healthcare workers as prompt for self-assessment
Requirements (Automated System):
- Mass text messaging services capable of sending text messages to groups of people simultaneously. Mass text messaging services are sometimes provided by independent internet-based service companies or are sometimes provided by cellular service providers.
- Database of contacts (i.e., healthcare workers under monitoring). In addition to contact number, database fields may include name, position, work unit or area, and monitoring end date.
- An effective and informative text message including frequency of messaging, timing of delivery, and any interactivity of interventions5.
Requirements (Manual System):
- Database of contacts (i.e., healthcare workers under monitoring). Because of the effort required in manual systems, this database should be carefully targeted to minimize workload and maximize benefit. Considerations for targeting might include:
- Documented COVID-19 exposure,
- Serving a population at high-risk for severe illness from COVID-19, and
- Serving a population at increased risk of being COVID-19 positive cases.
- Staff available to contact monitored healthcare workers with reminders.
- Phone and phone credit to support messaging and or calls.
Considerations:
- Same as Passive Strategy.
- Funding may be required to support mass text messaging.
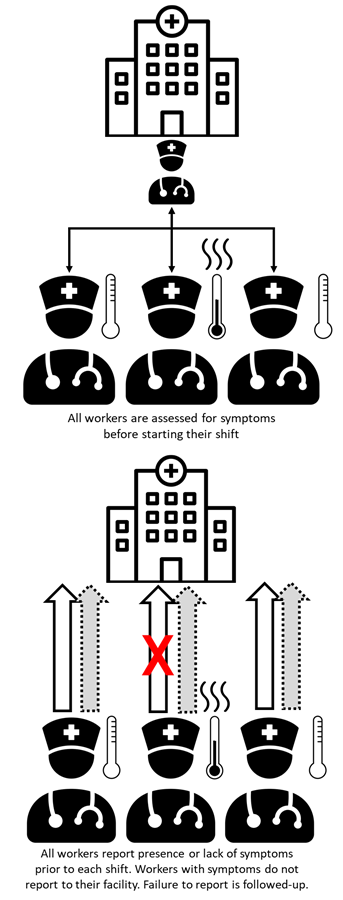
Figure: Active identification of healthcare workers with suspected COVID-19
Active Strategy
All healthcare workers present for in-person evaluation of symptoms and fever prior to each shift. If symptoms consistent with COVID-19 are reported or observed, healthcare workers are provided with immediate follow-up actions.
Remote Active Strategy
All healthcare workers report (e.g., by call or text) the absence or presence of symptoms consistent with COVID-19 remotely each day. Staff that fail to report or report symptoms are followed up.
Rationale:
While there is limited evidence for additional benefit from active healthcare worker monitoring, active strategies will theoretically result in increased healthcare worker adherence to self-evaluation of symptoms, thus enhancing patient and healthcare worker protection.
Requirements (Active Strategy):
- All requirements of Passive Strategy.
- Dedicated staff to evaluate healthcare workers before their shift (active) or respond and monitor healthcare worker reports.
- Physical area for staff evaluations that will allow recommended physical distancing (i.e., at least one meter according to WHO recommendations (CDC recommendation is at least 6 feet [1.8 meters]) and includes adequate hand hygiene stations (soap and running water or alcohol-based hand rub).
- No touch thermometers.
- Implementation plan that includes a method to ensure that staff present at a given place for pre-shift evaluation.
- Accountability system to ensure all healthcare workers have been evaluated (e.g., work slip sign-off).
Requirements (Remote Active Strategy):
- All requirements of Passive Strategy
- Accountability system to ensure all healthcare workers report in remotely prior to their work shift
Considerations:
- Same as Passive Strategy.
- Active monitoring of healthcare workers can be highly resource-intensive. There is limited evidence of increased effectiveness in prevention of nosocomial transmission beyond passive strategies.
- Acceptance by staff can be limited by perceptions of mistrust in ability to monitor and appropriately report symptoms.
- Active monitoring can decrease the likelihood that healthcare workers self-monitor signs and symptoms. Ideally, healthcare workers would check their own temperature and symptoms and would not present if not indicated. Any action that weakens self-monitoring should be implemented with caution.
- To decrease workload, and if accountability can be maintained, the following can be delegated to unit or immediate supervisors (e.g., head or charge nurses, department heads):
- Responsibility for receiving symptom/temperature reports and
- Monitoring staff compliance for the remote active strategy.
6. Identification of Inpatients with Suspected COVID-19
The development of acute respiratory infection and healthcare-associated pneumonia are common complications of hospitalization. However, it is important that clinicians maintain a high level of suspicion for COVID-19 when there is a compatible presentation. Because healthcare facilities often represent a gathering of individuals at higher risk of infection and adverse outcomes, the potential for outbreaks and harm to patients requires special effort to ensure any inpatient COVID-19 cases are identified.
A goal of identifying inpatients with suspected COVID-19 is to inform IPC strategies to prevent or limit transmission in healthcare settings. See interim WHO guidance on infection prevention and control during health care when COVID-19 is suspected.
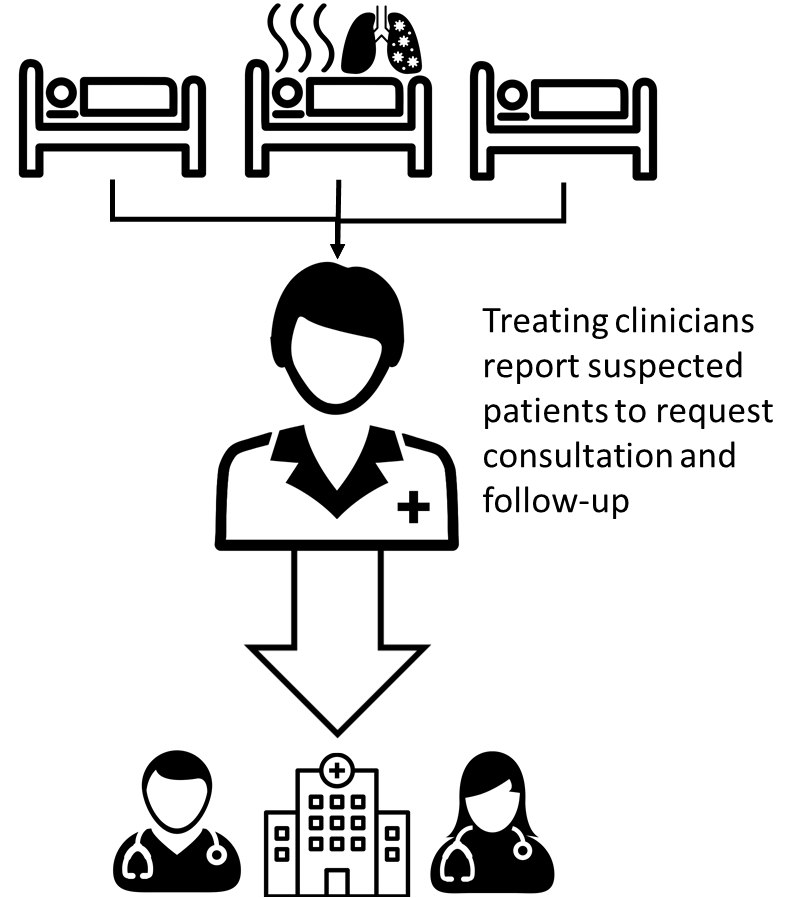
Figure: Passive strategy for identification of inpatients with suspected COVID-19
Passive Strategy:
Clinicians are kept informed6 on:
- Current COVID-19 case definitions,
- Latest description of COVID-19 clinical presentation, and
- Relevant local epidemiology, including at risk groups and association with travel or area of residence.
Clinicians are also made aware of what to do if they suspect COVID-19 in a hospitalized patient, including isolation precautions, PPE use, reporting/informing IPC focal point at the facility and public health authorities, and how to obtain testing, if available.
Applicable Surveillance Capacity Levels:
Applicable at all HAI surveillance capacity levels (i.e., very low to high)
Rationale:
Minimal disruption of existing clinical practice and no requirement for standardized data collection or form completion. Strategy seeks to encourage recognition and reporting by astute clinicians.
Requirements:
- Regular and up-to-date educational materials or job aids provided to and accessible by clinicians.
- COVID-19 case definitions.
- Standard operating procedure (SOP) for response to(e.g., isolation, cohorting, PPE).
- Acceptable reporting or communication channels to hospital administration and public health authorities.
Considerations:
- Strategy is dependent on participation and skill of available clinicians and an understanding of local epidemiology and clinical presentation of COVID-19, which may differ in different populations.
- Limited access to diagnostic testing will complicate this effort with the most conservative strategy being to treat all suspect cases as confirmed cases (empirical case determination) – potentially wasting resources, and if cases are cohorted, mixing positive and negative patients for extended periods.
- The degree of resource waste and case patient mixing will depend on the accuracy of empirical case determination.
- Supporting empirical case determination through clinician education and job aids (as described) can help improve accuracy of clinical diagnosis of COVID-19.
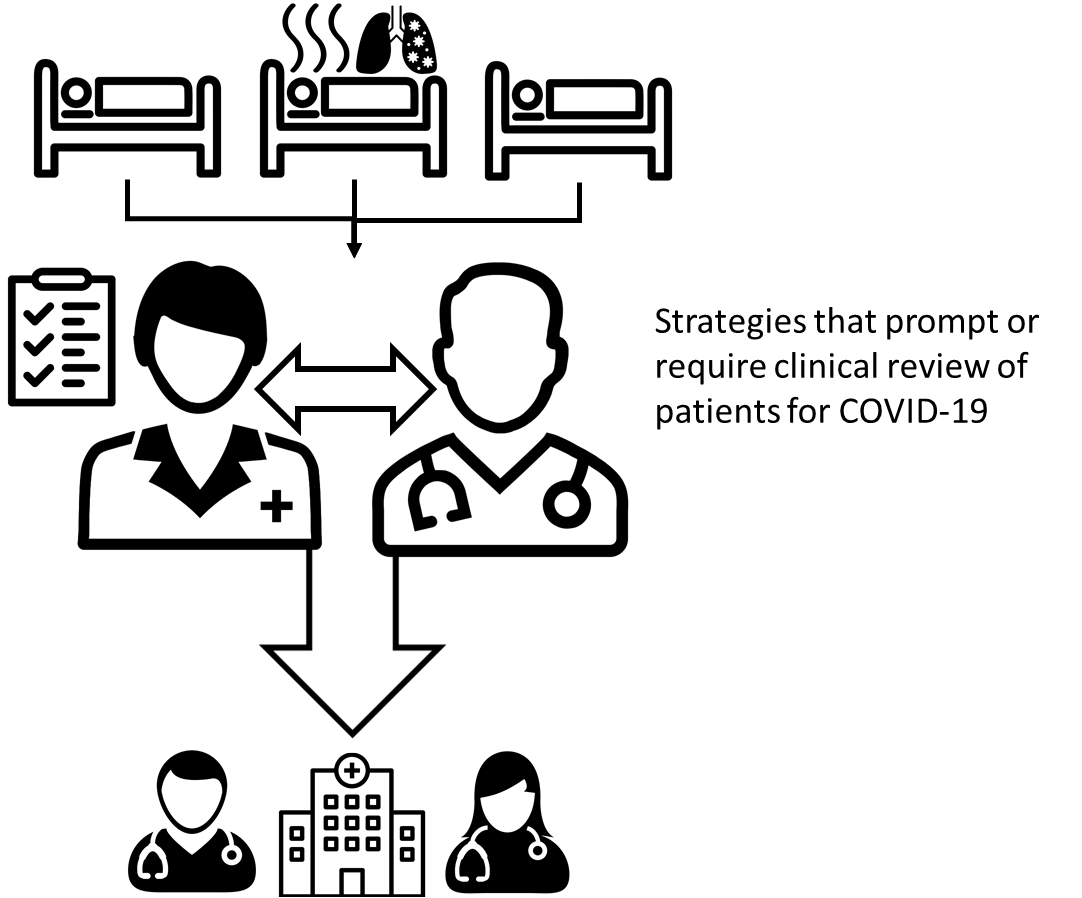
Figure: Enhanced passive strategy for identification of inpatients with suspected COVID-19
Enhanced Passive Strategy:
Enhancement of the passive strategy can be achieved through establishing systems that prompt or require clinicians to regularly review all patients for suspected COVID-19. Example enhanced passive strategies include:
- Incorporating consideration of COVID-19 into sign-out reporting.
- Requiring units to provide a daily clinician-generated list of suspected cases, including if there are zero cases.
- Sending specific daily requests to clinicians to report and discuss encountered patients with symptoms consistent with COVID-19.
Recommended Surveillance Capacity Level:
Applicable in most HAI surveillance capacity levels (very low to high)
Rationale:
Dialogue and accountability for case finding and reporting can improve empirical case determination, ensure patient evaluations are not missed, and help avoid clinician complacency over the long-term.
Requirements:
- All requirements of Passive Strategy.
- Strategy to prompt and/or ensure clinician review – requirements will depend on selected strategy.
Considerations:
- Effective strategies will be context specific and require thought and effort in design and implementation.
- May represent changes to current practice, which can limit acceptability.
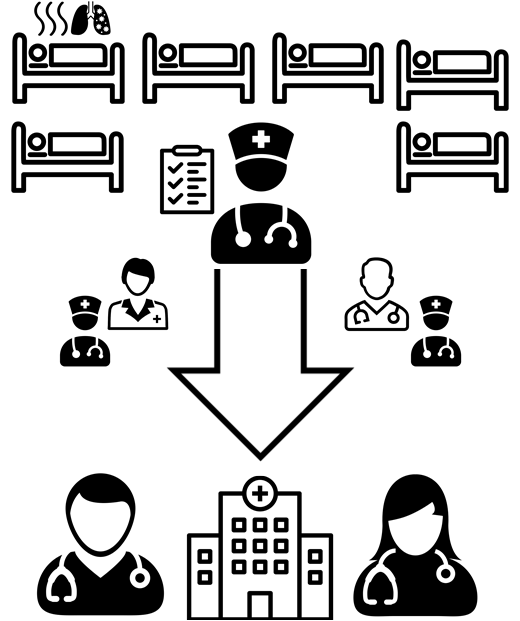
Figure: Active strategy for identification of inpatients with suspected COVID-19
Active Strategy:
Active case identification involves targeted data collection and review of patient information by groups specifically responsible for the identification of suspected COVID-19 cases. Examples of groups responsible for case identification and active case identification may include:
- Ministries of Health,
- Sub-national/local public health authorities, and
- Facility infection prevention and control teams.
Recommended Surveillance Capacity Level:
High existing surveillance capacity or medium capacity with the provision of additional resources.
Rationale:
Smaller more centralized team responsible for case identification can increase overall quality through dedicated training, improved engagement, limiting of competing priorities, and standardization of methods.
Requirements:
- Team with the information access, resources, and experience necessary for systematic review of patient information in order to appropriately apply standardized suspect case definitions.
- Group(s) with availability and responsibility for data collection, analysis/presentation, and information sharing.
- Group(s) with availability and responsibility for review of case-finding information with the authority and willingness to take appropriate action.
Considerations:
- Highly resource-intensive.
- Teams with the requisite skills can be difficult to build during outbreak response periods.
- Separates case finding activities from patient care activities, which can decrease acceptability and impact sustainability.
- Value of active inpatient case finding, especially the context of limited diagnostic testing, should be carefully considered.
Footnotes
[1] Healthcare workers are all people whose main activities are aimed at enhancing health. They include the people who provide health services — such as doctors, nurses, pharmacists, laboratory technicians — and management and support workers such as financial officers, cooks, drivers and cleaners.
[2] Furukawa NW, Brooks JT, Sobel J. Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg Infect Dis. 2020 Jul [Aug 2020]. https://doi.org/10.3201/eid2607.201595.
[3] Dedicated surveillance staff perform facility-based HAI surveillance as a regular part of assigned duties.
[4] In some settings, remote symptom reporting may represent a cost to healthcare workers that limits adherence. Any costs to healthcare workers caused by monitoring should be addressed in implementation planning.
[5] Hall, Amanda K., Heather Cole-Lewis, and Jay M. Bernhardt. “Mobile Text Messaging for Health: A Systematic Review of Reviews.” [In eng]. Annual review of public health 36 (2015): 393-415. https://doi.org/10.1146/annurev-publhealth-031914-122855.
[6] Methods to provide COVID-19 information may include dedicated trainings, in-services, educational conferences, job aid, web-sites, and written briefs.