Overdose Deaths and the Involvement of Illicit Drugs
Urgent Need for Overdose Prevention Interventions


More than 80% of drug overdose deaths involved opioids.

Nearly 85% of overdose deaths involved illicitly manufactured fentanyls,* heroin, cocaine, or methamphetamine (alone or in combination)

Potential opportunities to link people to care or to implement life-saving actions were present for more than 3 in 5 people who died from drug overdose.
* Illicitly manufactured fentanyls, or IMFs, include both fentanyl and fentanyl analogs
Overview
Illicitly manufactured fentanyls, heroin, cocaine, or methamphetamine (alone or in combination) were involved in nearly 85% of drug overdose deaths in 24 states and the District of Columbia during January–June 2019. More than 3 out of 5 overdose deaths involved at least one potential opportunity to link people to care before an overdose or to implement life-saving actions when an overdose occurred. These opportunities can be targeted to both prevent overdoses and improve response to overdoses to prevent deaths.
Problem: Most overdose deaths involve illicitly manufactured fentanyls
More than 80% of overdose deaths involved opioids, and most of these deaths specifically involved IMFs. IMFs put people at an increased risk for overdose death:
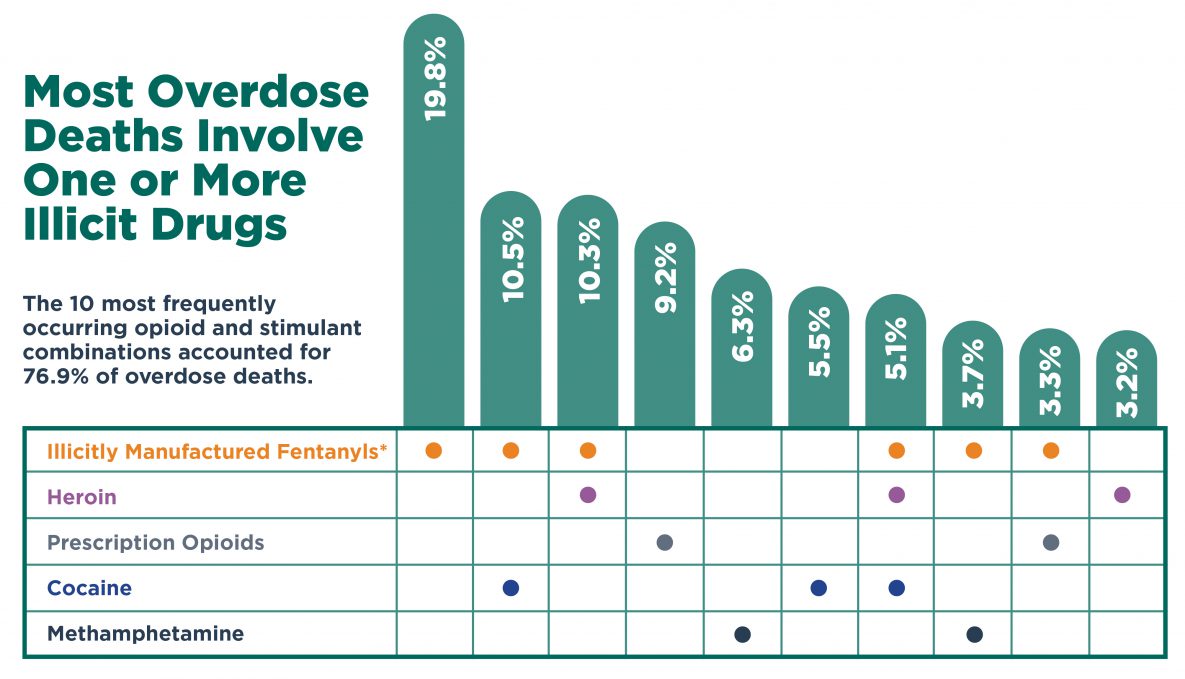
*IMFs include fentanyl and fentanyl analogs
Source: CDC's State Unintentional Drug Overdose Reporting System (SUDORS) 24 states and the District of Columbia reporting, January-June 2019
See more detailed info about the chart.
Opportunity: Insights for prevention and response efforts
Circumstances around overdose deaths provide insight into opportunities for prevention, treatment, and response efforts. In most overdose deaths, for example, at least one of the following circumstances were identified to be present, and each of these can impact the risk of overdose and represents a potential touchpoint for linkage to care:
- Recent release from an institution: Among the people who died from overdoses involving opioids, about 10% had had recently been released from an institution (such as jails/prisons, inpatient rehabilitation facilities, psychiatric hospitals).
- Previous overdose: Among the people who died from overdoses involving opioids, about 10% had had a previous overdose.
- Mental health diagnosis: Among all the people who died of a drug overdose, one quarter had a documented mental health diagnosis (percentage varied by type of drug overdose).
- Substance use disorder treatment: Among the people who died from overdoses involving opioids, nearly 20% had previously been treated for substance use disorder.
- Bystander present: Nearly 40% of opioid and stimulant overdose deaths occurred while a bystander was present.

More than 3 in 5 people who died from drug overdose had an identified opportunity for linkage to care or life-saving actions.
CDC is:
- Funding health departments through the Overdose Data to Action program, which includes expansion of programs linking people at risk for overdose to treatment and risk reduction programs.
- Working to improve communication and collaboration between public health and public safety.
- Collecting and analyzing data on drug overdoses to better identify opportunities for intervention, and to evaluate prevention efforts.
States and communities can:
- Initiate or continue medications for opioid use disorder among people leaving prison.
- Implement and track linkage to and retention in care, targeting people treated for a nonfatal overdose.
- Expand community naloxone distribution and increase naloxone prescribing and dispensing from pharmacies.
- Enhance coordination and integration of treatment for people with both mental health and substance use disorders.
Healthcare providers can:
- Identify mental health, social services, and substance use disorder treatment needs in order to provide appropriate care for patients.
- Link patients to appropriate care and treatment options.
- Follow the CDC Guideline for Prescribing Opioids for Chronic Pain.
Everyone can:
- Talk to a doctor if you or someone close to you needs help for substance use.
- Learn about naloxone, a life-saving drug that can reverse the effects of an opioid overdose when administered in time. You can also ask your doctor or pharmacist for a naloxone prescription if you or a loved one are taking high-dose opioids, have a substance use disorder, or have other risk factors for opioid overdose.
- Explore resources available to help with overdose prevention.
- Share on social media and help raise awareness.
When risk factors for drug overdose are present, overdose deaths can be prevented by using the following strategies:
- Enhancing linkage to care, including to mental health and substance use disorder treatment and support services.
- Increasing access to risk reduction services.
- Increasing distribution of and access to naloxone, especially for bystanders who may be able to reverse an opioid overdose.
- Reducing high-risk drug use by improving prescribing practices, preventing initiation of drug use, and addressing use of multiple drugs.
Related Pages and Resources
- Morbidity and Mortality Weekly Report (MMWR): Vital Signs: Characteristics of drug overdose deaths involving opioids and stimulants — 24 states and the District of Columbia, January–June 2019
- Vital Signs, 2019: Life-Saving Naloxone from Pharmacies
- Vital Signs, 2018: Opioid Overdoses Treated in Emergency Departments: Identify Opportunities for Action
- CDC Drug Overdose Website
- CDC’s Rx Awareness Campaign
- CDC’s Drug-Free Communities
- CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016
- Syringe Services Programs (SSPs)
- COVID-19 Questions and Answers: For People Who Use Drugs or Have a Substance Use Disorder
Other Sites
- Find Treatment Providers Near You
- U.S. Department of Health & Human Services Guidance on Naloxone Co-Prescribing [PDF]
- Office of National Drug Control Policy
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Surgeon General (SG)
- U.S. Food and Drug Administration (FDA) Special Report
- National Institute on Drug Abuse (NIDA)