CDC Kenya Surveillance

CDC Kenya supports the development and implementation of population and facility-based disease surveillance systems that are used for data collection, analysis, and reporting. These surveillance systems assess disease burden in communities, identify outbreaks, guide public health action and evaluate the impact of health interventions.


The prevalence of HIV among these fishing communities is high, estimated around one-third, making them a priority for HIV prevention and treatment.
Fishing communities on the shores of Lake Victoria in western Kenya are at high risk of HIV infection. Due to their geographic isolation, low literacy levels, high mobility, risk behaviors, and the near absence of a wide range of basic health services, these communities are particularly vulnerable to the HIV epidemic. Unfortunately, there have been limited population-based surveys among these communities that improve understanding of HIV epidemiology and inform interventions and services for this population.
In 2018, CDC Kenya in collaboration with the National AIDS and STI Control Program (NASCOP), Kenya Medical Research Institute (KEMRI), and University of California, San Francisco (UCSF) completed a household survey of fishing communities on eight island beaches of Lake Victoria. This study aimed to determine the prevalence of HIV, risk factors, and HIV service coverage among fishing communities. Data on demographics, behavior, home-based HIV and malaria rapid testing as well as viral load for HIV positive persons were collected from the participants.
Given the location remote location of the study sites, this study presented a number of challenges. “We almost capsized on our way to the islands!” recalled one of the study investigators. The team had to take one to three hour boat rides from the mainland across to the islands and back, facing harsh conditions such as the hot sun or rough waters. Despite the numerous challenges experienced, the team persevered and completed the study successfully.
Studies such as this one are critical to understanding the dynamics of the HIV epidemic and moving towards epidemic control. Due to untiring efforts of CDC researchers and their partners, Kenya’s public health community has an increased understanding of how to better serve these fishing communities and continue making gains towards achieving HIV epidemic control.

Malaba border crossing in western Kenya. Photo from Nation Media Group.
In light of recent infectious disease outbreaks in Africa, the Government of Kenya recognized the need to further improve port health services. Effectively mitigating the importation, or exportation, of infectious diseases and other public health threats requires strong national—and ports of entry (POE)—level preparedness and response capacity and cross-border collaboration. In 2018, the Kenya Ministry of Health’s Port Health Services (PHS) adapted and implemented CDC’s Division of Global Migration and Quarantine Border Health Capacity Discussion Guide. Through this process, tailored action plans were developed to address identified areas for improvement to strengthen services at two ground crossings (Busia and Malaba) and Jomo Kenyatta International Airport (JKIA). Busia and Malaba POE border Uganda and are the busiest with over 3,000 international travelers and 1,600 vehicles crossing daily. JKIA is Kenya’s main international airport with an average of 109 international and 55 domestic flights arriving every day and a total of 20,000 international travelers from Africa and other continents using the airport daily. The developed action plans included better characterization of cross-border population movement, enhancing inter-sectoral collaboration at POEs, improving community-based surveillance strategies around the POE and multisectoral and multi-agency disease preparedness and response plans at POEs. The next steps include mini-residency for PHS officers to learn about quarantine stations operating procedures and best practices, develop and finalize a multiagency public health emergency response plans for the three priority POEs and initiate cross-border experience exchange mechanisms through regular conference calls.
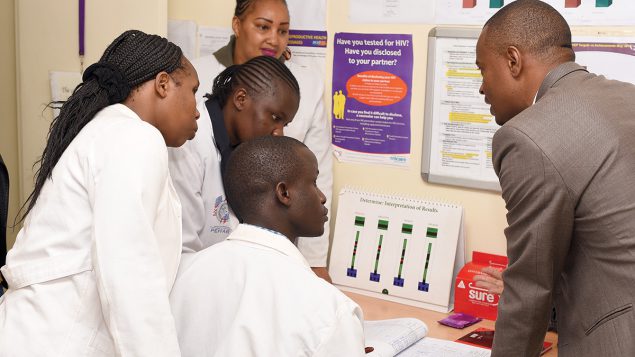
Through PEPFAR, CDC actively participated in the implementation of KENPHIA, the Kenya Populationbased HIV Impact Assessment. KENPHIA required teams to work extensively across the country, including with field-based laboratory work. KENPHIA has also provided opportunities to see how PEPFAR has improved lives for countless Kenyans.
In June 2018, Kenya’s Ministry of Health, in collaboration with ICAP, an organization within Columbia University, launched KENPHIA to measure the reach and impact of HIV programs in Kenya. KENPHIA included 20,000 randomly selected households and interviews from approximately 35,000 people across the country. Survey participants received household-based HIV counseling and testing conducted by trained survey staff. KENPHIA will—for the first time— record population-based HIV estimates for all 47 counties and provide a national rate for Hepatitis B and syphilis prevalence. The results will measure national progress toward UNAIDS’ 90-90-90* goals and guide policy and funding priorities.
The PEPFAR funding for KENPHIA is coordinated and managed through CDC. Staff from the CDC’s Division for Global HIV and TB (in headquarters) along with staff from CDC Kenya have worked together to:
- Advise on the protocol development,
- Facilitate weeks of training sessions for field staff,
- Provide technical assistance with survey implementation, and
- Serve as field monitors to ensure adherence to survey procedures.
Dr. Emily Zielinski-Gutierrez, chief of CDC Kenya’s Surveillance and Epidemiology Branch, explained that “observation of survey procedures occasionally allows monitors to hear an individual’s story of being diagnosed and receiving life-sustaining antiretroviral therapy, affirming the reasons behind all the work we do.”
Beyond serving as an expert advisor and key contributor to KENPHIA, CDC has demonstrated a strong commitment to supporting the survey teams that are largely responsible for implementing KENPHIA.
Data collection for KENPHIA wrapped up in February 2019. Preliminary survey findings are expected to be released in mid-2019 and will likely be a major reference for determining future HIV programming in Kenya.

KENPHIA field teams visited remote areas to gather data on HIV and other conditions

Anthony Waruru (white shirt), CDC Kenya epidemiologist, participates in the study as a field monitor and provides technical assistance and feedback to field staff.
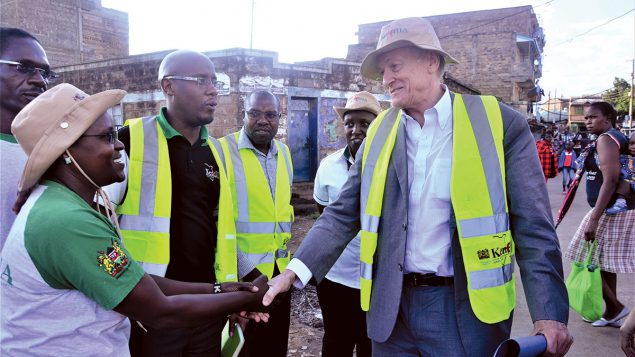
Dr. Kevin De Cock (R), CDC Kenya country director, makes it a priority to visit teams in the field and learn about how the study is being implemented and accepted.
*UNAIDS Fast-Track Targets: 90% of people living with HIV diagnosed; 90% of the diagnosed on antiretroviral therapy; and 90% of the treated virally suppressed by 2020.
On June 19, 2018, CDC and KEMRI laboratory staff at KEMRI’s Center for Global Health Research in Kisumu, Kenya were notified of a suspected case of viral hemorrhagic fever in a patient admitted to the Siaya County Referral Hospital. The patient, a fisherman, had developed a fever four days earlier and at the time of sample collection was bleeding from the mouth and nose. CDC tested the sample for Ebola, Marburg, Crimean-Congo, Yellow fever, Rift Valley fever (RVF) and dengue by a laboratory technique called polymerase chain reaction (PCR). The results identified RVF virus as the cause of the fisherman’s illness. Unfortunately, the patient died a few hours after the sample was collected.
Rift Valley fever, a mosquito-borne disease that primarily affects animals occurs in large outbreaks every few years, but these outbreaks have not previously affected the counties neighboring Lake Victoria. As RVF is not well known by the local population, two scenarios emerged during this period following the patient’s death. First, the deceased family blamed a neighbor for bewitching the victim following a recent physical altercation, leading to growing hostility in the village. Second, when the patient was admitted to the hospital, the healthcare workers who handled the case were quarantined for observation, but not before a number of them had had contact with the patient. Even though the patient did not have a history of travel outside of Kenya, other infectious disease threats such as Marburg which had been recently reported in Uganda were a concern. This made the confirmatory diagnosis all the more important. Due to the longstanding relationship with CDC’s work in western Kenya, the medical officer reached out to CDC and KEMRI to assist with laboratory testing. Within six hours, the sample had been
transported over one hour’s drive away, analysis completed, and the results of RVF were shared with the hospital. Quarantined staff were released under self-observation and the patient’s family was informed of the cause of death, thereby reducing tension in the village. CDC management in western Kenya also mobilized immediate outbreak support which included raising awareness across the entire county as well as an assessment of the extent that animals and people were affected in the area. Residents were informed on how to properly dispose of dead animals in cases of abortion in sheep and cattle – one of the main symptoms of the infection. Health officials also instituted mosquito vector control by removing, or cleaning, mosquito breeding sites such as used tires, plastic garbage, water storage or other receptacles that accumulate water where mosquitoes can breed. The results also enabled the Ministry of Health, the Ministry of Agriculture and Livestock, KEMRI and CDC to conduct contact tracing.
The timely diagnosis and intervention by CDC in western Kenya alleviated additional health and economic losses often associated with RVF outbreaks and limited further infections. It also served as an important reminder that infectious disease threats can emerge anywhere at any time, and become a threat everywhere.

Taking a blood sample from a camel in Marsabit County, Kenya to test for zoonotic pathogens including MERS-CoV.
Assessing the risk of disease emergence and spread is a key component of global health security. Resources and limited funds for detection, prevention and control need to be targeted to specific disease threats, either nationally, or to at-risk areas in Kenya, where threats are most likely to occur and spread. Moreover, risks present in one part of the world are informative for Kenya, but it cannot be assumed that the risks are the same. CDC Kenya, along with CDC Atlanta and partners, is supporting a wide range of risk assessment activities in Kenya, including for Zika, MERS-CoV, avian influenza, Rift Valley fever and cholera. To understand the current risk of Zika infection in Kenya, in October 2017, CDC Kenya initiated a cohort study of pregnant women in Mombasa.
Women enrolled in the study when they first come for antenatal care and are followed up monthly until delivery. They are then assessed for acute Zika infection and the newborns are screened for any congenital abnormalities. To date, after testing more than 1,000 women, CDC Kenya have not identified any cases of Zika infection, suggesting
that Zika is currently not a major threat to women in coastal Kenya.
In Marsabit County, the majority of camels show evidence of previous infection with MERS-CoV, yet no exposed camel handlers have been identified as infected to date. In order to understand the risk camels may pose to humans, CDC Kenya and partners initiated a longitudinal study in Marsabit County among camels and their herders. Young camels were enrolled and followed-up with bi-weekly testing to assess for acute infection with MERS-CoV and to detect the actual virus. To date over 200 camels and their handlers have been enrolled and testing is ongoing in the KEMRI laboratories with additional testing at CDC headquarters in Atlanta.
Avian influenza remains a global security threat to human and animal health. In 2017, influenza A/ H5N8 was detected among wild and domestic birds in on the shores of Lake Victoria in Uganda. CDC Kenya responded by conducting a survey of more than 3,000 samples of wild bird feces on the Kenyan shores of Lake Victoria which identifies low pathogen viruses of H5N2. A more comprehensive avian influenza surveillance was initiated in the main poultry (live bird) markets around Kenya. Samples are collected from poultry at the various markets and on symptomatic partners during monthly visits.
In 2018, based on previous risk assessments, health authorities initiated enhanced surveillance for RVF nationally when heavy rain was predicted in Kenya which is often linked with outbreaks. To support the RVF outbreak response, CDC Kenya, together with Global Health Security Agenda partners, supported the Government of Kenya in securing public diplomacy funds to provide communication outreach to 20 high-risk counties as well as providing training on sample collection to the affected counties. In particular, the CDC supported outbreak investigations in Siaya County and disease surveillance activities in the Kakuma refugee camp detected human RVF infections. This work expanded the number of counties now considered at risk for future RVF infections.
Lastly, cholera remains a constant epidemic threat in Kenya and has been a particular burden since 2014. Control and prevention fundamentally lies with improved WASH (water, sanitation and hygiene) practices, however, oral cholera vaccine (OCV) can help control outbreaks and provide valuable protection while longer-term infrastructure is put in place. Yet it is clear that some areas of Kenya are more vulnerable than others, leading to the concept of cholera “hotspots” where the use of OCV and focused WASH efforts would be most effective. CDC Kenya and the Division of Foodborne, Waterborne and Environmental Diseases are supporting WHO, UNICEF and the Ministry of Health to complete Kenya’s Cholera Elimination Plan. This plan will include a “hotspot” analysis of pre-existing data conducted by partners. The data will allow policy makers to target WASH and vaccine efforts to parts of Kenya considered at highest risk.
CDC Kenya is supporting ongoing infectious disease risk assessments though a variety of means including outbreak investigations, surveillance, research studies and analysis of pre-existing data. These efforts will
strengthen health security in Kenya by targeting resources where they are most needed.