CDC’s Innovation
‹View Table of Contents
Improving Specimen Transport through Repurposing Advanced Cold Chain Technology

Poor specimen transport networks can take days to move biological samples from the collection site to the testing laboratory and lead to sample deterioration, which may affect the sample testing results. Through an innovative collaboration, CDC partnered with the Association of Public Health Laboratories and the technology company, Global Good, to modify existing vaccine storage technology to support laboratory sample transport in resource poor environments. These modifications are designed to provide cold chain stability for up to 30 days and triple packaging of the samples within a lockable chamber, therefore maintaining the integrity of laboratory samples during transit and improving the laboratory’s ability to protect the world from dangerous pathogen outbreaks.
Building Sustainable Whole Genome Sequencing Capacity for Surveillance, Advanced Diagnostics and Pathogen Discovery
Whole Genome Sequencing (WGS) may be the most important advance in infectious disease laboratory technology of our time. This tool is set to integrate pathogen diagnostics (viral, bacterial, parasitology and mycology), pathogen characterization (AMR, virulence, and subtyping) and pathogen identification (outbreak etiology and molecular epidemiology) in the public health laboratory. CDC is working with partners in multiple countries to develop this expertise among host-country laboratorians. Through hands-on work, laboratorians are empowered to become self-sufficient without external expertise, to make this vision a reality.
For example, in only five years, CDC and the Government of Indonesia built WGS capacity at the Eijkman Institute for Molecular Biology in Jakarta. The state-of-the-art Emerging Virus Research Unit (EVRU) laboratory is one of the leading facilities in Southeast Asia and, for the first time, provides the fourth most populous country in the world with the capacity to detect emerging vector-borne pathogens using WGS. EVRU scientists have been able to sequence the first Zika virus isolated in the country, characterize the whole genome of a neuroinvasive dengue virus, and identify Rickettsia felis in fatal neurological disease cases. The success of the team led to the institute being named as the National Genomic Research Center in 2018 by the Government of Indonesia. In addition to the WGS advances and success, the EVRU, with CDC support, has trained more than 1,500 clinicians in the diagnosis of vector-borne diseases and more than 400 laboratorians in advanced biosafety techniques.
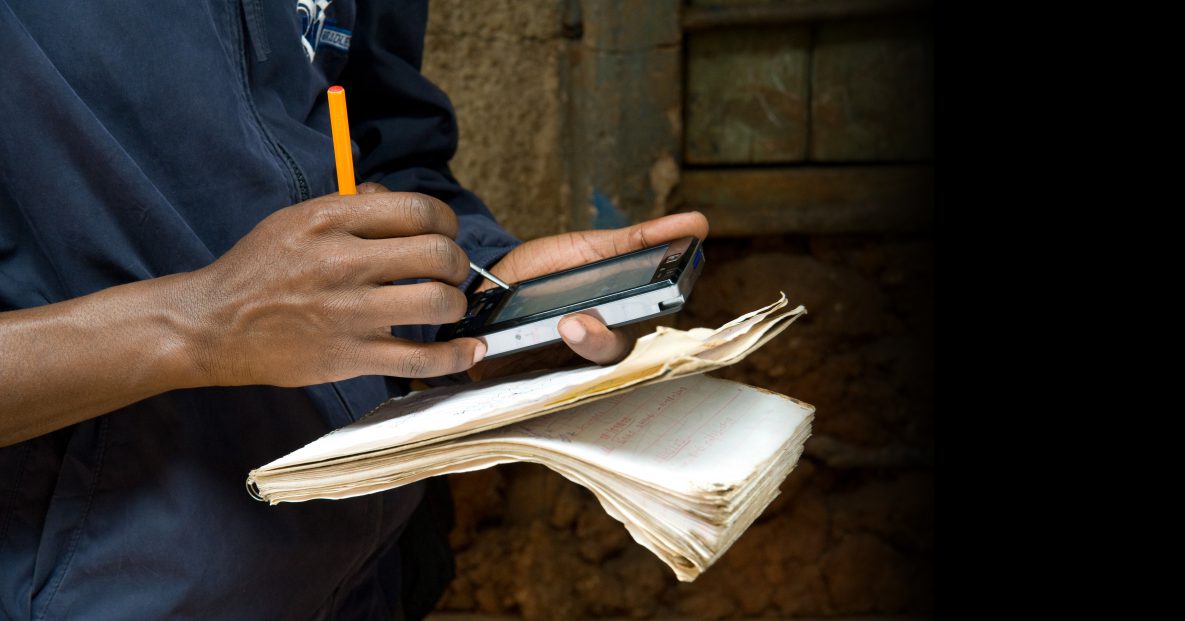
Rolling Out an Improved Surveillance App
In May 2018, the Western Area rural district of Sierra Leone, with CDC technical assistance, launched a program that enables workers to report critical health information to the country’s surveillance network via a smartphone app. Health workers use the app to submit weekly reports to the country’s electronic Integrated Disease Surveillance and Response system, which is designed to capture data on any device, including desktops, laptops, tablets, and smartphones. Most systems also have the capability to be used offline, which is especially helpful in rural areas with poor connectivity. Fast and accurate information from local health facilities can help us get ahead of diseases and stop outbreaks.
Crowdsourcing to Report and Respond to Zoonotic Diseases
CDC’s Farmer & Rabies smartphone app allows people who work with poultry and swine to report human and animal sicknesses or deaths with the click of a few buttons. Recognizing that those who are regularly in close contact with animals are often the first affected when a zoonotic disease strikes, the Thai Ministry of Public Health’s (MOPH) Bureau of Epidemiology partnered with CDC in 2017 to develop a new app and website for use by farmers, local health volunteers, and health officers. The reporting tool quickly informs the MOPH of increases in animal illness and deaths, illness in people possibly linked to animals, or other abnormal events. A provincial One Health team monitors the reports and initiates rapid response to control outbreaks. In its pilot year, the app led to successful investigations of potential Strepotococcus suis infection and Japanese encephalitis. In 2018, the app was expanded to include reporting of dog and cat bites to help detect rabies outbreaks. By putting surveillance in the hands of the community, the app helps contain zoonotic diseases before they spiral into epidemics.
Testing Technology in the Field
In all regions of the world, measles cases are on the rise. Many countries have declared outbreaks. Especially risky for young children, measles can have serious health consequences. Yet the disease is preventable through vaccination. Since measles spreads rapidly, having technology that can provide immediate results in the field is a radical innovation for health security. To help stop measles in its tracks, CDC is testing an innovative new technology, the Measles-Rubella Box (MR Box). The field study which takes place in the Democratic Republic of the Congo (DRC) was planned and executed by CDC laboratorians. The technology, developed by scientists from the University of Toronto, has the potential to confirm active measles and rubella infections in the field to help quickly stop outbreaks before they spread beyond borders.
In the DRC, measles and rubella tests have to be sent to the national laboratory for confirmation. DRC is a large country, and transporting blood samples can be difficult. It takes a minimum of a week to get results from a sample. The MR Box has the potential to solve this issue.
The MR Box is portable, easy to use, and—at less than a 25 cents per test—affordable. It is also compact, weighing less than 11 pounds. The technology inside each box, called digital microfluidics- enzyme-linked immunosorbent assay (DMF-ELISA), or “ELISA on a chip,” has some distinct advantages over other technologies used to detect measles and rubella. It can test samples from up to four people at the same time and yields results in less than an hour—much more efficient than transporting blood samples to the national lab and waiting for laboratory results. Because measles is highly infectious, delaying public health response by several days can lead to significant expansion of outbreaks.
Disease detectives from DRC’s CDC-supported FETP were integral to the testing process, which involved long days going from house-to-house in Kinshasa. FETP residents and graduates tirelessly knocked on doors, getting up early and working late, to collect blood samples and fill out electronic data forms. Though additional work is required, FETP’s work in DRC is a first step. Without urgent efforts to address measles, outbreaks like the ones occurring around the world will continue, and innovations like the MR Box are an important step toward containing these threats.
Participatory Epidemiology to Understand Human Migration Patterns
The Population Connectivity Across Borders (PopCAB) method, is a CDC-developed tool kit designed to engage multi-sectoral stakeholders at national, intermediate, and community levels in focus group discussions with participatory mapping. A PopCAB implementation team has trained Ministries of Health (MOH) and partners on how to analyze and create a visual representation of the gathered information to tailor public health surveillance, preparedness, and response efforts as well as cross-border collaboration strategies that respond to population mobility dynamics. In 2018, CDC PopCAB experts trained the Ugandan MOH and their country partners to conduct population movement and connectivity mapping to identify potential high-risk areas where Ebola could spread from the Ebola outbreak in DRC. Uganda has since used the results from their mapping to strengthen cross-border public health collaboration and to inform social mobilization, infection, prevention, and control, and vaccination activities in high-priority districts along the Uganda-DRC border.