CDC surge capacity in action
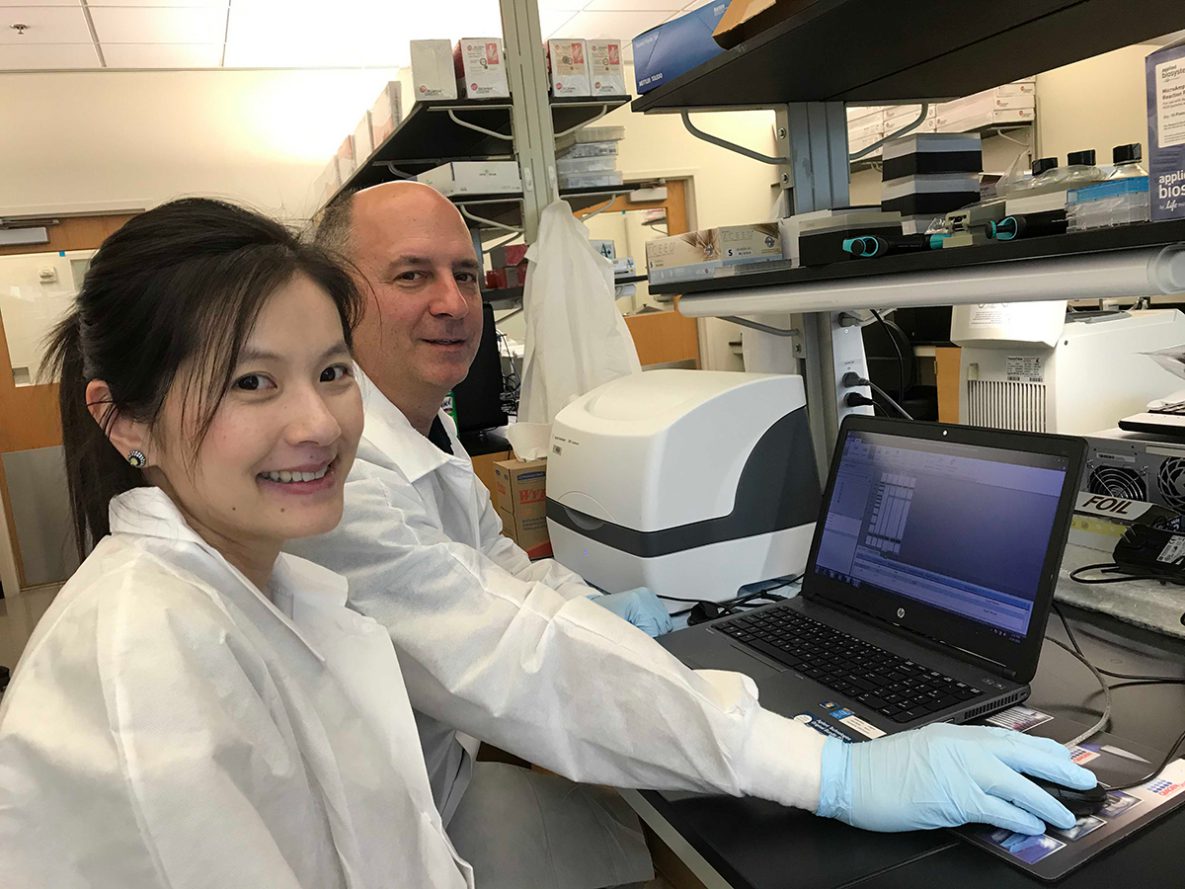
CDC microbiologists Gerald Pellegrini and Po-Yi Ho purify sample DNA for sequencing. Photo taken by: Yulin Lin (NCHHSTP)
Approximately 25 states across the country have reported outbreaks of hepatitis A. When hearing about hepatitis A, many people think of contaminated food or water. However, most people don’t know that in the United States, hepatitis A is more commonly spread from person to person, which is how people are getting infected in the current outbreaks. While hepatitis A can affect anyone, certain groups are at greater risk of being infected in these outbreaks, including people who use drugs, men who have sex with men, and those experiencing homelessness. Since 2016, more than 20,000 cases and 200 deaths have been reported nationally. Unfortunately, hospitalization rates in this outbreak are more than 50 percent and are suspected to be a result of high rates of people with other health problems, including hepatitis C. West Virginia and Kentucky are among the states most affected by the hepatitis A outbreak.
To support the additional response capacity needs of states, in March 2017, CDC’s Division of Viral Hepatitis (DVH) stood up the Incident Management System to assist health departments with response efforts. They collaborated with CDC experts across the agency in the Immunization Services Division, the Division of State and Local Readiness, and the newly-established Global Emergency Alert and Response Service (GEARS) to provide a coordinated effort. GEARS manages CDC’s Global Disease Detection Operations Center and Global Rapid Response Team (GRRT). “While CDC’s GRRT was initially set up to deal with international public health emergencies following the large-scale Ebola outbreak in West Africa, we are equally capable of supporting domestic missions should CDC programs have a need for our on-call rostered staff. It was in line with our rapid response mission to support the domestic hepatitis A outbreak needs,” stated GRRT lead Brian Wheeler.
The hepatitis A response required multiple areas of expertise, including epidemiology, laboratory, and management and operations. GRRT rosters approximately 400 surge staff, with more than 50 ready to deploy on short notice. These highly trained CDC responders are able to deploy within 72 hours as needed for domestic or global responses to support a variety of needs. “We’ve been fortunate to have colleagues in GRRT who can identify the right candidates for laboratory, epidemiology, and public health advisory activities,” said CDC’s Hepatitis A response chief of staff Kevin O’Connor.
CDC epidemiologist Anne Purfield was deployed to assist with vaccine implementation and logistics in West Virginia from December 2018 to January 2019. Purfield collaborated with state and local health departments to hold hepatitis A vaccination clinics at medication assisted treatment centers. She faced many challenges while working with a marginalized population in a low-resource setting and learned how to best support communities dealing with drug addiction. Recognizing the difficulty in reaching the affected population with health care-related services, Purfield seized on an opportunity to positively impact the health and well-being of patients attending medication assisted treatment centers. She worked with local epidemiologists, nurses, and CDC public health associates to vaccinate current patients and engaged treatment centers to incorporate hepatitis A vaccination during new patient intake assessments. Family members and friends of center patients were also offered the vaccine. By the end of Purfield’s deployment, 600 high-risk individuals had been vaccinated through six vaccination clinics in one month.
In addition to providing epidemiology expertise, the GRRT also deployed laboratory experts to meet the increased demand for testing patient specimens. Since November 2018, four CDC laboratory experts have assisted the CDC Division of Viral Hepatitis Laboratory in Atlanta, Georgia, through 30-day or 60-day assignments to process the backlog of samples from this hepatitis A outbreak. Support provided by CDC GRRT experts allowed for a more comprehensive response to the hepatitis A outbreaks in West Virginia and also in Kentucky. O’Connor noted, “Collaboration with GRRT is ongoing and has been critical to ensuring needed additional capacity in both the CDC lab and in the impacted jurisdiction.” Catherine Lewis, lead epidemiologist for the West Virginia State Health Department vaccine initiative added, “During the outbreak in West Virginia, a number of CDC support staff came to aid our hepatitis A response. These individuals played an integral part in our work and our success, and we are very grateful to have had them on our team.”

Staff prepare for the first Hepatitis A vaccination clinic held at a methadone treatment center. Pictured are three vaccinators — a nurse from the health department, a volunteer nurse, and a medical student volunteer. Photo taken by: Anne Purfield (NCHHSTP)

Caitlin Cohen, a PHAP assigned to the West Virginia Bureau for Public Health (WVBPH), takes a break from recruiting and registering treatment center patients for Hepatitis A vaccination. The vaccine team often left Charleston, WV at 3:00 a.m. to open vaccination clinics at 5:00 a.m. Photo taken by: Anne Purfield (NCHHSTP)
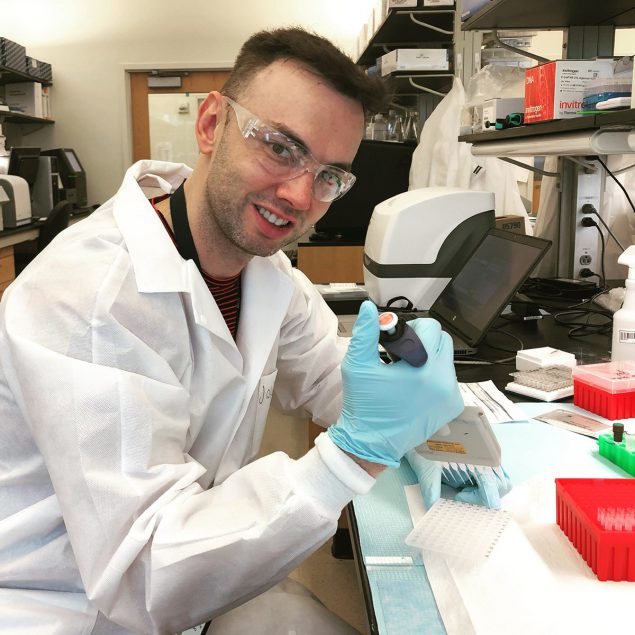
Laboratorians supported the CDC’s Hepatitis A Response. Laboratory support includes molecular testing using RT-PCR and Next Generation Sequencing platforms. This type of testing help identify outbreak clusters and chains of transmission and then would help determine interventions for the affected populations which we know to be one with special needs regarding homelessness/drug use. Photo taken by: Yulin Lin (NCHHSTP)