Ugandan healthcare facilities make alcohol-based hand rub during COVID-19
Summary
- CDC launched a study in 2018 to see if health facilities making their own alcohol-based hand rub (ABHR) would improve hand hygiene among health workers.
- ABHR production supported by CDC’s office in Uganda and local partner IDI is saving the Ministry of Health and districts money related to infection prevention and control.
- During the COVID-19 pandemic, the success of the CDC’s locally-produced ABHR efforts in Uganda increased proper hand hygiene behaviors.

Sign mounted on tree in Amuru district in Uganda says, “Together we will kick COVID-19 out of Uganda.” Photo credit: IDI
As COVID-19 spread around the world in early 2020, countries quickly faced a global shortage of hand sanitizer. Alcohol-based hand rub (ABHR) can contribute to stopping the spread of many diseases. Some healthcare facilities (HCFs) in Uganda did not have to scramble to find hand sanitizer. That’s because they were already producing low-cost ABHR with support from the U.S. CDC office in Uganda and a local partner, the Infectious Diseases Institute (IDI). CDC and IDI also provided communications materials to promote good hand hygiene practices.
Keeping hands clean is essential to help prevent the virus that causes COVID-19 from spreading. This is particularly important to prevent healthcare workers (HCWs) from transferring germs from one patient to another.
Hand rubs are effective in the absence of a sink, according to the World Health Organization (WHO). In Uganda, ABHR is expensive and not readily available in poor and hard to reach communities.
Fortunately, a solution was already in place, thanks to a study that began in the Kabarole district of southwestern Uganda in 2018. That’s when CDC, IDI, and the International Water and Sanitation Centre (IRC WASH) collaborated to study the benefits of making ABHR locally, and whether it could improve hand hygiene among health workers.
Researchers found that hand hygiene was low due to limited access to water and soap. Over the next year, 30 health clinics received hand sanitizer made at an ABHR production unit at the highest-level community health facility, next to a district hospital

Locally produced alcohol-based hand rub filled in bottles that range from small to medium and large bottles are on display in production facility in Tororo, Uganda. Photo credit: IDI
“We sent two technical staff members to the facility to support production, distribution, and coordination of the locally produced hand rub. The technical officer, from our partner organization IDI, was responsible for internal quality control and trained district staff handled external quality control,” says Maureen Kesande, the senior Infection Prevention and Control (IPC)/WASH project officer at IDI.
“When the alcohol-based hand rub was delivered to each health care facility, we held hand hygiene sensitization meetings with facility management, supported them to set up or re-activate IPC committees, and trained designated staff to monitor use of the hand sanitizer and update stock cards, ” says Kesande.
Just as the ABHR study was reaching its halfway mark, Uganda registered a case of Ebola that crossed into the Kasese district, which borders the Democratic Republic of the Congo.
With more support from CDC’s Global Health Security program and the Division of Foodborne, Waterborne, and Environmental Diseases, IDI expanded the alcohol-based hand rub production model to the Kasese district to support the Ebola prevention and preparedness efforts in December 2019.
The team also trained two ABHR producers and set up a production unit at the district health offices that supplied the hand sanitizer to 150 public and government facilities as well as a few high-risk communities.
As a result, when Uganda had to stop COVID-19, these infection prevention measures were already in place in both the Kabarole and Kasese districts.
“The ABHR project not only increased availability, access, and acceptability of alcohol-based hand rub, it also improved hand hygiene compliance among healthcare providers—paving the way for the larger, $1.1m CDC/IDI WASH project today,” Kesande says.
Another benefit is that many healthcare workers were already practicing hand hygiene because of infection prevention control mentorship activities.
“Information, education, and communication materials on hand hygiene, which are one of the critical components of COVID-19 prevention and control, were also already in place and they were quickly adapted,” says Kesande.
With COVID-19 in Uganda, the team extended their project to two border districts—Tororo in the eastern part of the country (bordering Kenya) and Amuru in northwestern Uganda (bordering South Sudan). These districts were considered high-risk areas for COVID-19 because the neighboring countries had already registered cases. Indeed, a majority of the first confirmed cases in Uganda were truck drivers identified at border crossings.
CDC and IDI are the primary partners for Uganda’s Ministry of Health (MOH) during the COVID-19 response. Fred Tusabe, who is IDI’s ABHR Project Technical Production Officer, says the alcohol-based hand sanitizer project saves MOH and districts a lot of money related to infection prevention and control.
“A liter of commercial sanitizer is about $7. When we produce it locally, we almost cut that price in half—down to about $4,” Tusabe explains. “We use the WHO standard protocols for local production of ABHR, and efficacy is guaranteed because the quality is monitored and tested before being placed on the shelf.”
Not surprisingly, demand for hand sanitizer increased a lot during the COVID-19 pandemic as did the costs for buying ABHR and production supplies, like ethanol.
“The price for a liter of commercial hand sanitizers rose to $54 from $7 before COVID,” Tusabe says. “Our ABHR project could not have been timelier.”
Project impact

ABHR Project Technical Production Officer, Fred Tusabe, tests locally produced hand rub as part of the internal quality control process after producing a batch of the alcohol-based hand sanitizer at the Kasangati model production/training unit.
Photo credit: IDI
Olive Tumuhairwe, the Kabarole District IPC Focal Person, says the ABHR project has increased their healthcare workers’ confidence in their ability to respond to disease outbreaks.
“Our healthcare workers did not panic. COVID-19 found us in a good place,” she says.
When COVID-19 struck, Uganda’s National Medical Stores — which by law must get, store, and distribute essential medical supplies — started distributing hand rub.
“All we got was 24 liters, which could only serve two big health care facilities for a month,” Tumuhairwe explains. “As such, use of the hand sanitizers was limited to senior healthcare workers. However, with the ability to now produce their own hand rub, everyone is covered.”
“We have enough stock now,” she adds, noting that they are able to produce 40 liters of hand sanitizer in just 10-20 minutes.
IDI also trains staff in two regional referral hospitals: Jinja and Mubende—and has a model ABHR production unit in Kampala.
In mid-2021, the team started ABHR production to the high risk, hard to reach border districts in the Karamoja region in northeastern Uganda. Now, 19 health facilities in Uganda’s Moroto district and 21 health facilities in the Kotido district can make alcohol-based hand rub.
This expansion makes alcohol-based hand rub for 276 locations, including health facilities and community meeting points. Nearly 800,000 more people now have access to alcohol-based hand rub. The districts also receive training, materials, and mentorship from IDI with support from CDC to produce hand rub. When more hand rub is made than needed, it is distributed to other places in need.
Dr. Amy Boore, who leads CDC’s disease outbreak and emergency response efforts in Uganda commits to continuing support of this model and roll-out of ABHR programs as a key IPC outbreak preparedness package.
“Our CDC technical teams have continued advocating with health leaders to strengthen the model—production and distribution of ABHR—and hope to strengthen it more through the MOH infection prevention and control pillar.”
The success of the CDC’s ABHR efforts in Uganda can be seen in the Kabarole district, where the first study to produce ABHR locally was launched. During the COVID-19 pandemic, nine times as many people practiced proper hand hygiene with locally produced hand sanitizer than before the project began.
“I’m happy that our efforts are helping to strengthen preparedness and response for outbreaks, as it has been with COVID-19,” says Tusabe.
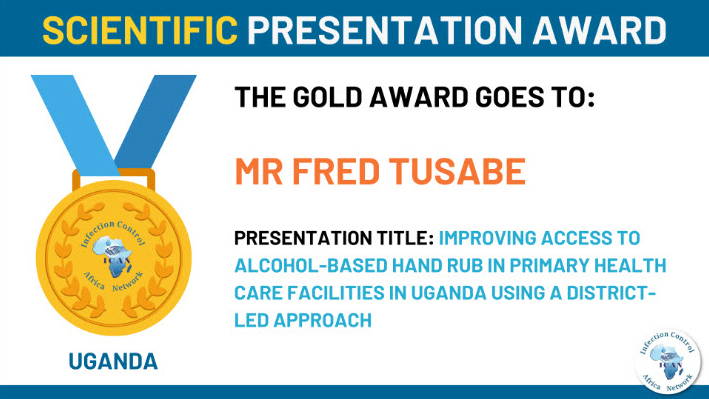
He presented research about IDI and CDC’s ABHR work at the Infection Control Africa Network scientific conference in November 2021. The organization recognized CDC and IDI’s work by presenting Tusabe with a gold award for scientific presentation.