Innovative Medicine Delivery Models Improve ART Access in Mozambique
Summary
- Antiretroviral treatment (ART) saves lives of people living with HIV (PLHIV), but adherence to the daily medicine combination presents challenges.
- On average, three out of 10 people interrupt treatment in the first year due to various challenges.
- New medicine delivery models, called Differentiated Service Delivery (DSD), are giving options to make ART adherence easier and visit health facilities less often.
Antiretroviral treatment (ART) saves lives of people living with HIV (PLHIV), but adherence to the daily combination of medicines presents challenges. Compliance to treatment helps stop new infections and accelerates epidemic control. The Centers for Disease Control and Prevention (CDC) is working with the Ministry of Health (MOH) of Mozambique to implement interventions focused on the diverse needs of PLHIV to accelerate epidemic control in the country.
In the last decade, Mozambique has dramatically expanded the number of PLHIV receiving ART. With an HIV prevalence of 13% among its adult population, the country has increased ART coverage from 200,000 to more than 1.5 million individuals. The MOH has ensured that ART is available at more than 1,500 health centers, thanks to coordinated efforts with the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund to Fight AIDS, Tuberculosis, and Malaria (GF). Still, with about 2.1 million PLHIV, progress towards universal ART coverage remains a challenge.

Patients who are stable and have good treatment support can collect medications for a three-month period in a single visit to the pharmacy. Maputo, Mozambique. Photo by: Ricardo Franco/CDC.
PEPFAR estimates from January 2021 indicate that 82% of all PLHIV have been diagnosed in Mozambique, of which 81% are receiving ART, and of which 88% are virally suppressed. Becoming virally suppressed is essential for the health and quality of life of PLHIV and to prevent new HIV infections.
Despite progress, increased ART coverage has been hampered by a high rate of discontinuation of therapy. On average, about three out of 10 people interrupt treatment in the first year due to barriers to service uptake that include lack of transport, cost of travel to health facilities, waiting times, quality of health services, and stigma and discrimination associated with HIV.
To address this challenge, CDC and its partners support the implementation of evidence-based interventions to improve HIV services in about 470 large-volume health centers located in seven of the country’s 11 provinces. In total, these clinics provided ART to more than 930,000 PLHIV in early 2021, representing approximately 67% of the national treatment cohort.

Community Adherence and Support Groups reduce number of visits to health facilities that patients need for ART pick-ups. Maputo, Mozambique. Photo by Ricardo Franco/CDC.
To expand ART coverage, it is necessary to consider the challenges patients face. CDC supports MOH in the development and implementation of Differentiated Service Delivery (DSD) models that adapt HIV services to facilitate ART adherence.
The COVID-19 pandemic led the Mozambican health authorities to implement prevention measures to contain SARS-CoV-2 transmission. Community health workers started to distribute medications at client homes in some parts of the country.
MOH accelerated the implementation of DSD models, with the help of PEPFAR and its partners. The decentralization of ART delivery to the community level is a priority for MOH, as it allows patient-centered ART access and reduces the risk of COVID-19 transmission in health facilities.
DSD models help PLHIV adhere to ART
Service supply models allow patients to visit health facilities less frequently to receive medications. DSD models allow PLHIV to choose what best meets their needs. Simultaneously, DSD reduces the burden on the health system and allows health providers to focus on patients that require more support.

Differentiated Service Delivery models are innovative ways to make adherence to ART medications easier. Maputo, Mozambique. Photo by Ricardo Franco/CDC.
CDC’s implementing partners provide trainings to help health workers and lay counsellors educate users about the availability of these models and create demand. Implementing partners are also responsible for monitoring the implementation of DSD models in health facilities, thus allowing for the quick identification of challenges and solutions to keep patients on treatment.
Although the DSD policy is recent, this approach first emerged in Mozambique in 2010, through the Community Adherence and Support Groups (GAAC in its Portuguese acronym). The intervention expanded rapidly at the national level with PEPFAR support and CDC contributing to the development of national GAAC guidelines and program implementation.
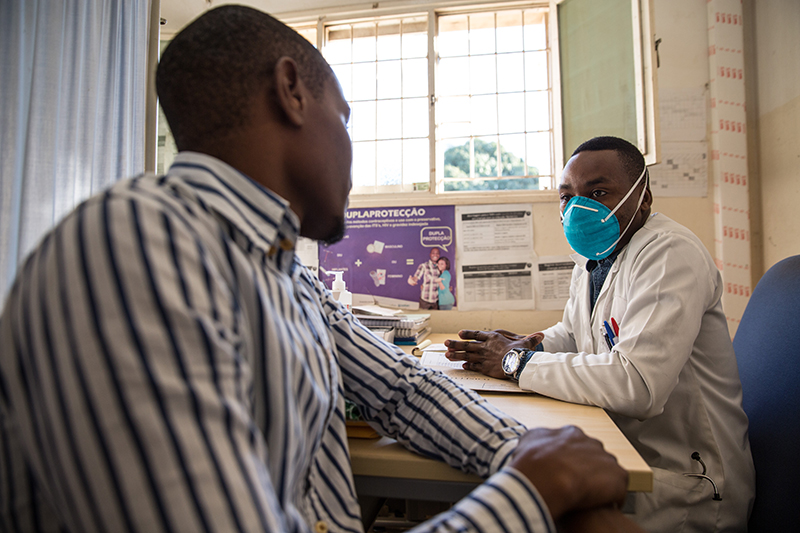
Healthcare provider explains ART delivery options at a health facility in Maputo, Mozambique. Photo by Ricardo Franco/CDC.
Community Adherence and Support Groups (GAAC): organizes patients in groups of up to six people and establishes a rotating schedule of ART pick-ups at the health facility. With this model, a patient only visits the health facility every six months to receive medication and have follow-up clinical consultations.
GAAC also offers psychosocial support, improves the link between the health facility and the community and establishes an early warning system for disease screening and early identification of therapeutic failure.
Fluxo Rápido or Rapid Flow: allows users to receive medication from the health facility’s pharmacy during five months without having to see a clinician first, reducing waiting times.
Dispensa Trimestal or Quarterly Dispensing: patients who are stable and have good treatment support can choose this model that makes it possible to collect medications for a three-month period in a single visit to the pharmacy. This approach is also being expanded to cover a six-month period, particularly benefiting migrant populations, such as miners.
More and more patients are making use of these ART pick-up models. Approximately 70% of all patients on ART now collect their medicines on a quarterly basis. These models have been helpful during the COVID-19 pandemic, they allow patients to continue ART without needing to visit a health facility.
Paragens Únicas or Single Stop Model: services are bundled to meet the needs of specific client populations through family-centered practices allowing all members of a family to access services at the same visit. The model is available in youth dedicated services (Serviços Amigos dos Adolescentes e Jovens – SAAJs), tuberculosis/HIV on-stop-shops, and services friendly to key populations.