Combatting AMR/HAI in South Caucasus
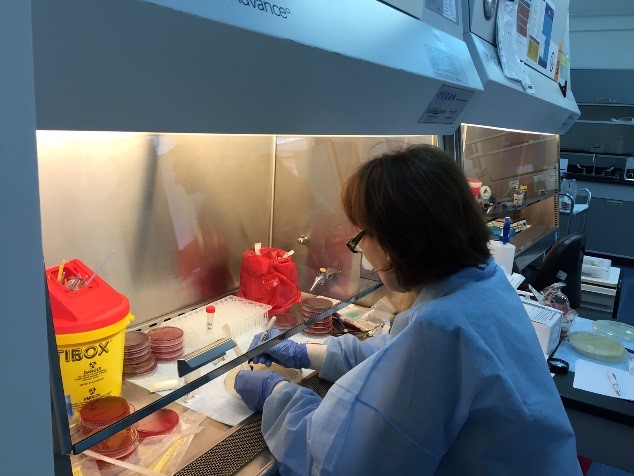
Irma Shvelidze, lab technician in bacteriology, in Kutaisi, Georgia. Photo by Nino Macharashvili.
Antimicrobial resistance (AMR). Hospital-acquired infections (HAIs). These chilling phrases have unfortunately become a part of our everyday language. Combatting them is an important element of CDC’s Global Health Security Agenda.
In the CDC-South Caucasus Office (CDC-SC), Marika Geleishvili and Beth Skaggs are on the front lines of the efforts to combat AMR and HAIs. Marika is an epidemiologist focused on leading efforts to establish a hospital-based AMR/HAI surveillance network and Beth is the laboratory advisor focused on strengthening laboratory capacity and determining the profile of AMR/HAI organisms.
Poor infection prevention and control (IPC) practices in hospital settings fuel the burden of HAIs and AMR. CDC-SC, in collaboration with CDC’s Division of Healthcare Quality Promotion (DHQP), has begun a proactive effort to reduce HAIs and spread of AMR through IPC trainings and monitoring, as well as implementing hospital-based HAI and AMR surveillance, which includes determining the antimicrobial susceptibility patterns of the HAI-causing bacterial pathogens.
Historically, hospitals in the region have resisted surveillance systems to monitor and report HAI and AMR cases because of potentially negative consequences to their business and reputation. Through CDC-SC’s efforts in training, promoting evidence-based decisions and policy making, clinicians have started to change their mindset around HAIs and AMR.
In 2015, ICU physicians asked CDC-SC for assistance in establishing HAI/AMR surveillance and implementing IPC training and guidelines. Physicians acknowledged that it would be useful to put a surveillance system in place to determine HAI-causing organisms in hospitals, and then to implement IPC interventions. These were huge, welcome steps forward. The physicians expect to see the number of HAIs increase in the short term as a result of active surveillance and better reporting, but they also expect to see the numbers decrease in the long term as IPC interventions are routinely implemented.
Overuse and inappropriate use of antibiotics are important drivers for the emergence of AMR. The work CDC-SC is doing with its Georgian partners is focused on improving the use of laboratory data to guide antibiotic treatment and to raise awareness of the critical importance of IPC policies and practices to reduce HAIs. The Georgian government has recently passed new legislation prohibiting the sale of antibiotics without a physician prescription. This new policy, coupled with CDC-SC’s epidemiological and laboratory technical assistance, make the goal of reducing the emergence and spread of AMR pathogens possible. Training clinicians to interpret and apply laboratory results in treatment decision-making will reduce the overuse and inappropriate use of antibiotics. Currently there are country-level workshops available on IPC and on-the-job bacteriology lab training and mentorship.
To be effective, HAI surveillance must be supported by lab confirmation of the pathogen and subsequently the antimicrobial susceptibility pattern. This requires the lab to have resources to conduct AMR surveillance and to compile data. Strengthening lab capacity is crucial to identifying pathogens which meet the case definition of HAI. Improved laboratory capacity to rapidly and accurately detect etiologies of HAIs and AMR profiles will increase the demand for laboratory services.
Microbiology is an essential part of standard procedures for isolating and identifying HAIs and for susceptibility testing using international standards. Georgia tests in accordance with the European Union Committee on Antimicrobial Susceptibility Testing, which is the European version of the U.S. Clinical Laboratory Standards Institute. The purpose is to build lab capacity according to international standards of microbial testing and results.
CDC-SC is also collaborating with Walter Reed Army Institute of Research (WRAIR) on lab capacity strengthening to support detection of AMR pathogens. WRAIR has a lab within Georgia’s national reference lab, which it uses to examine pathogens and resistance mechanisms at molecular levels. All of these data are used to inform policy and practice in controlling AMR.
Georgia’s national reference lab is the Lugar Center, a state-of-the-art national reference lab built with USG funding. CDC-SC is working to transform the Lugar Center into a Center of Excellence in the region, and, in collaboration with WHO, into a WHO Collaborating Center for AMR. That means an infrastructure will be used to create a regional lab that will serve Georgia and the region as a diagnostic leader for identifying and preventing AMR.
The Lugar Center would serve the South Caucasus region which includes Georgia, Armenia, and Azerbaijan, a region of approximately 17 million people. CDC-SC has a big role in the diplomacy required to get countries to collaborate and send specimens and samples to another country for testing. An important part of that diplomacy is emphasizing that keeping all people healthy is paramount. CDC-SC also implements regional FELTP from all three countries. The FELTP residents and graduates participate in HAI surveillance programs. The HAI activities started in Georgia first, but other countries in the region are propagating Georgia’s experience via FELTP residents and graduates.
The good news is that the efforts by Beth and Marika and their colleagues from DHQP are yielding results. Clinicians are contacting CDC-SC to report that they have a problem with HAIs in their facility and they need CDC-SC’s help to recognize, detect, and prevent it. CDC-SC is seeing an incremental but steady change in practices that are slowing new HAIs through better prevention. Nurses now have an opportunity for training on better IPC practices to reduce HAIs, interacting with clinicians about prevention, teaching the importance of handwashing, improving blood sampling safety, and injection safety. This is the first opportunity the nurses have had to be trained on IPC since they graduated from school. It’s challenging for them to change habits and practices but they are looking forward to seeing the results – reduced AMR/HAI rates.
While there’s always a need for increased resources and increased lab capacity, CDC-SC is improving lab testing, providing practical training for healthcare workers, and implementing surveillance, prevention, and control guidelines in hospitals. There is still much work to be done but CDC-SC is staffed with dedicated public health professionals who, along with country and global partners, are determined to combat AMR and HAIs in the region.