CDC Haiti: Using Data to Keep HIV Patients in Care
This web page is archived for historical purposes and is no longer being updated.
CDC Haiti has had tremendous success enrolling HIV positive patients on antiretroviral treatment (ART). In 2016, the Haitian National AIDS Program adopted the World Health Organization’s “Test and Start” approach, which makes patients with an HIV-positive diagnosis immediately eligible for ART. CDC Haiti’s PEPFAR partners were quick to implement “Test and Start” and to transfer pre-ART patients, or those individuals whose CD4 counts were not low enough under previous guidelines to initiate treatment, onto ART. The rapid and efficient roll-out of “Test and Start” greatly increased the number of people living with HIV (PLHIV) enrolled on treatment and highlighted the successful collaboration between CDC Haiti, the Haitian Ministry of Health (MOH), and CDC’s implementing partners.
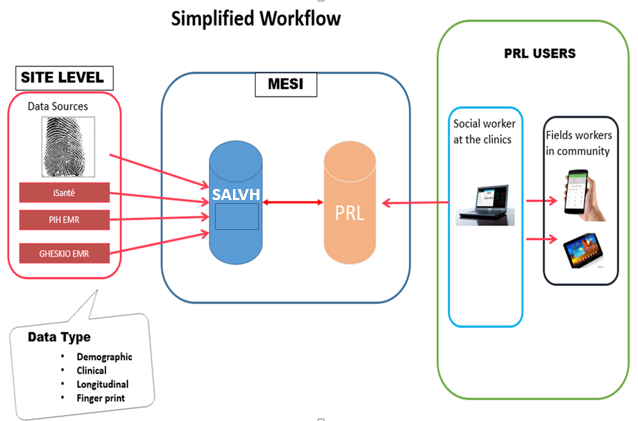
Figure 1. This image demonstrates the flow of data between clinical and community levels. Patient data, including biometric coding, is collected at the site level through three EMR systems and linked to the longitudinal, case-based surveillance system SALVH. PLR receives data from SALVH which clinicians and CHWs can use to actively track patients.
Despite the success implementing “Test and Start” and enrolling patients on treatment, CDC Haiti and its partners were challenged to ensure patients remained adherent to treatment. In response to this problem, CDC Haiti and partners developed the Patient Linkage to and Retention in care (PLR) program. PLR is a multifaceted package of interventions that employs innovative community-based approaches, a unique patient identifier via biometric coding, and a case-based surveillance system to keep patients on treatment and to reduce loss to follow up (LTFU). In 2016, the Office of the Global AIDS Coordinator (OGAC) recognized CDC Haiti’s PLR program and biometric coding as a Game Changer – a title awarded to innovative approaches to fighting HIV/AIDS.
The PLR is an active tracking tool that is a component of a larger HIV health management information system (HMIS) which CDC Haiti helped to build alongside the Haitian MOH and its partners. This HMIS platform includes a longitudinal case-based surveillance system known as SALVH (Suivi Actif Longitudinal du VIH en Haïti). SALVH captures new HIV cases, including the patient’s fingerprint as a unique identifier, from three electronic medical records (EMR) systems that cover more than 95% of patients on ART in Haiti. The PLR tracking tool is linked directly to SALVH and can pull key data from the surveillance system to notify practitioners when patients have missed appointments.
To bring patients back into care, community health workers (CHWs), equipped with electronic tablets for data collection, are deployed to the field to visit the missing patients at their home. The PLR program also facilitates a proactive approach to avoid LFTU by promoting regular contact with all patients, not only defaulters, via calls, text messages, or home visits and by increasing linkages between communities and facilities – such as through community-based drug distribution.
The patient-level data collected through the PLR tracking tool is stored on an easily accessible platform that clinicians and social workers at the facility level and CHWs at the community level can utilize to actively track patients. Access to patient-level data allows CDC Haiti and partners to address critical gaps in the patient care system through targeted interventions. Over 80 health facilities in Haiti currently use the PLR tracking tool which has brought nearly 17,000 patients LTFU back into care.
With over 90,000 patients enrolled on ART in Haiti and over one million Haitians receiving HIV-related health services each year, it is essential that data is used to guide program implementation and to direct resources to the areas of highest impact. The PLR program will continue to be a fundamental aspect of CDC Haiti’s HIV/AID program in the coming years and a major tool in moving the country toward epidemic control.