Multistate Outbreak of Fungal Meningitis and Other Infections – Microscopic Gallery of Pathologic Results
On October 30, 2015, CDC updated its web resources for patientsand clinicians. Patients affected by tainted steroid injections from the New England Compounding Center continue to receive treatment for their infections and clinicians should continue to monitor patient recovery. All relevant materials for patientsand cliniciansconcerning the multistate outbreak of fungal meningitis and other infections are located on this page.
This page highlights pathological findings for the Multistate Fungal Meningitis Outbreak Investigation.
Disease Caused by Fungus in Brain Tissue
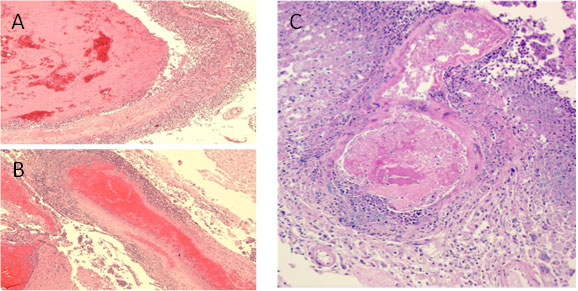
Major histopathologic findings in clinical cases of meningitis show evidence of necrotizing, suppurative vasculitis with thrombosis (A and B). These findings are seen in many cases involving a branch of the basilar artery (C), which are consistent with the clinical findings.
Disease Caused by Fungus in Brain Tissue
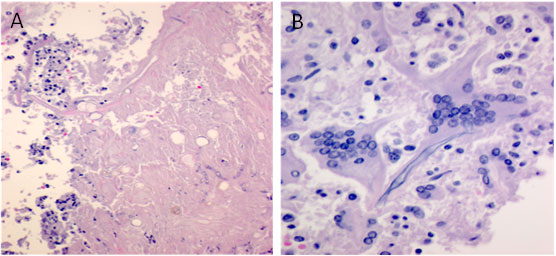
Another finding in the basilar artery is necrosis (A) and giant cell arteritis (B).
Fungus in Brain Tissue
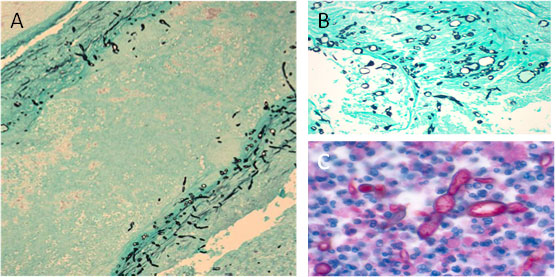
Fungal hyphae (black) can be visualized with silver stain within vessel walls (A) and in area of necrosis in basilar artery (B). Using a polyfungal immunohistochemistry reagent, fungal hyphae (red) is also seen in the purulent exudate in spinal meningitis (C).
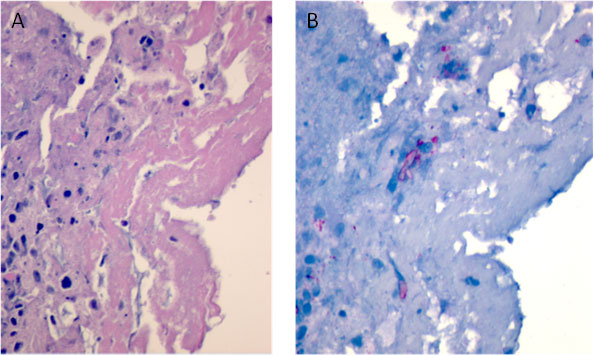
Fungus in Tissue Surrounding the Spinal Cord
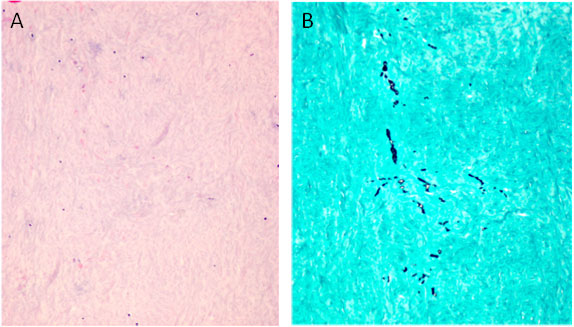
Arachnoiditis is a complication present in some of the patients. In tissue obtained adjacent to the affected site, dense collagen-rich soft tissue with no inflammatory infiltrate (A) is seen. Fungal hyphae are seen in this tissue by silver stain (GMS) with modified oxidation times (B).
Fungus in a Hip Joint
In patients with arthritis, fibrin and necrotic debris are seen in affected joints (A). Although rare, immunohistochemistry facilitates the focal detection of hyphae (B) in these areas (red staining).