CDC Recommends All Nursing Homes Implement Core Elements to Improve Antibiotic Use
Urged to implement at least one core element immediately
New recommendations from the Centers for Disease Control and Prevention (CDC) advise all nursing homes to improve antibiotic prescribing practices and reduce their inappropriate use to protect residents from the consequences of antibiotic-resistant infections, such as C. difficile.
To guide these improvements, CDC released a new resource: Core Elements of Antibiotic Stewardship for Nursing Homes. The Core Elements for Nursing Homes expand upon CDC’s recommendation last year that all acute care hospitals implement an antibiotic stewardship program designed to optimize treatment of infections while reducing adverse events associated with antibiotic use.
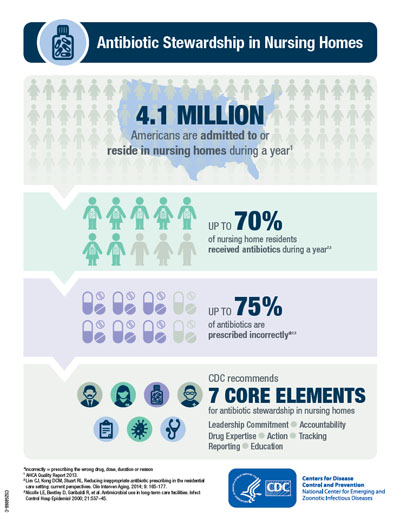
Approximately 4.1 million Americans are admitted to or reside in nursing homes each year.1 Antibiotics are the most frequently prescribed medications in nursing homes. Up to 70 percent of residents receive one or more courses of antibiotics during a year.2,3 Up to 75 percent of antibiotics prescribed in nursing homes are given incorrectly, meaning either the drug is unnecessary or the prescription is for the wrong drug, dose, or duration.2,3
“Superbugs that are hard to treat pose a health risk to all Americans, particularly the elderly whose bodies don’t fight infection as well,” said CDC Director Tom Frieden, M.D., M.P.H. “One way to keep older Americans safe from these superbugs is to make sure antibiotics are used appropriately all the time and everywhere, particularly in nursing homes.”
Protecting nursing home residents
The Core Elements provide practical ways for nursing homes to initiate or expand antibiotic stewardship activities. The guide provides examples of how antibiotic use can be monitored and improved by nursing home leadership and staff. The companion checklist can be used to assess policies and practices already in place and to review progress in expanding stewardship activities on a regular basis. However, depending on resources, some facilities may need more time to implement all these important protections. Ultimately, nursing home antibiotic stewardship activities should, at a minimum, include the following:
- Leadership commitment: Demonstrate support and commitment to safe and appropriate antibiotic use.
- Accountability: Identify leaders who are responsible for promoting and overseeing antibiotic stewardship activities at the nursing home.
- Drug expertise: Establish access to experts with experience or training in improving antibiotic use.
- Action: Take at least one new action to improve the way antibiotics are used in the facility.
- Tracking: Measure how antibiotics are used and the complications (e.g., C. difficile infections) from antibiotics in the facility.
- Reporting: Share information with healthcare providers and staff about how antibiotics are used in the facility.
- Education: Provide resources to healthcare providers, nursing staff, residents and families to learn about antibiotic resistance and opportunities for improving antibiotic use.
“We encourage nursing homes to work in a step-wise manner implementing one or two activities at first, then gradually adding new strategies from each core element over time,” said Nimalie Stone, M.D., CDC medical epidemiologist for long-term care. “Taking any of these actions to improve antibiotic use in a nursing home will help protect against antibiotic-resistant infections and more effectively treat infections. This could lead to better recoveries from infections and ultimately improve health outcomes for all residents.”
The Centers for Medicare & Medicaid Services (CMS) recently proposed a rule that would require long-term care facilities to incorporate an antibiotic stewardship program, including antibiotic use protocols and antibiotic monitoring, into their infection prevention and control program. According to CMS, these requirements will decrease unnecessary or inappropriate antibiotic use by ensuring that residents who need antibiotics are prescribed the right drug at the right dose for the right duration.
“Nursing homes that engage in antibiotic stewardship improve care for residents and help reduce antibiotic resistance,” said Patrick Conway, M.D., M.Sc., CMS deputy administrator for innovation and quality & CMS chief medical officer.
The release of CDC’s Core Elements for Nursing Homes is one step in achieving the objectives set out in the National Action Plan for Combating Antibiotic-resistant Bacteria. Investments to improve antibiotic stewardship across all settings are part of CDC’s Antibiotic Resistance Solutions Initiative for fiscal year 2016.
As part of the plan, within three years CDC will provide technical assistance to federal facilities (e.g., those operated by the Department of Defense, the Department of Veterans Affairs, and the Indian Health Service) and other large health systems to scale up implementation and assess interventions to improve outpatient antibiotic prescribing, extend effective interventions to long-term care settings, and ensure long-term sustainability of antibiotic stewardship efforts.
To learn more about the Core Elements of Antibiotic Stewardship for Nursing Homes, visit: http://www.cdc.gov/longtermcare/prevention/antibiotic-stewardship.html.