CDC: 1 in 3 antibiotic prescriptions unnecessary
New CDC data show large percentage of antibiotics misused in outpatient settings
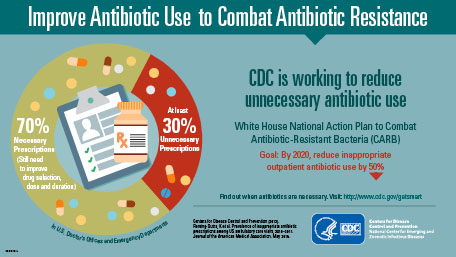
At least 30 percent of antibiotics prescribed in the United States are unnecessary, according to new data published today in the Journal of the American Medical Association (JAMA) by the Centers for Disease Control and Prevention (CDC), in collaboration with Pew Charitable Trusts and other public health and medical experts.
The study analyzed antibiotic use in doctors’ offices and emergency departments throughout the United States. CDC researchers found that most of these unnecessary antibiotics are prescribed for respiratory conditions caused by viruses – including common colds, viral sore throats, bronchitis, and sinus and ear infections – which do not respond to antibiotics. These 47 million excess prescriptions each year put patients at needless risk for allergic reactions or the sometimes deadly diarrhea, Clostridium difficile.
The researchers also estimated the rate of inappropriate antibiotic use in adults and children by age and diagnosis. These data will help inform efforts to improve antibiotic prescribing over the next five years.
“Antibiotics are lifesaving drugs, and if we continue down the road of inappropriate use we’ll lose the most powerful tool we have to fight life-threatening infections,” said CDC Director Tom Frieden, M.D., M.P.H. “Losing these antibiotics would undermine our ability to treat patients with deadly infections, cancer, provide organ transplants, and save victims of burns and trauma.”
The fight to stop antibiotic resistance
In 2015, the White House released The National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB), which set a goal of reducing inappropriate outpatient antibiotic use by at least half by 2020. This means that 15 percent of antibiotic prescriptions (or half of the 30 percent that are unnecessary) must be eliminated by 2020 to meet the CARB goal.
As part of the effort to achieve the national goal, CDC researchers analyzed the 2010–2011 National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS) to determine the number of outpatient visits resulting in antibiotic prescriptions by age, region, and diagnosis in the United States from 2010-2011. They found that:
- Of the estimated 154 million prescriptions for antibiotics written in doctor’s offices and emergency departments each year, 30 percent are unnecessary. This finding creates a benchmark for improving outpatient antibiotic prescribing and use.
- About 44 percent of outpatient antibiotic prescriptions are written to treat patients with acute respiratory conditions, such as sinus infections, middle ear infections, pharyngitis, viral upper respiratory infections (i.e., the common cold), bronchitis, bronchiolitis, asthma, allergies, influenza, and pneumonia. An estimated half of these outpatient prescriptions are unnecessary.
“Setting a national target to reduce unnecessary antibiotic use in outpatient settings is a critical first step to improve antibiotic use and protect patients,” said Lauri Hicks, D.O., director of the Office of Antibiotic Stewardship in the Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, CDC, and commander in the U.S. Public Health Service. “We must continue to work together across the entire health care continuum to make sure that antibiotics are prescribed only when needed, and when an antibiotic is needed that the right antibiotic, dose, and duration are selected.”
Health care professionals, health systems, and patients must take these actions to improve antibiotic use:
- Outpatient health care providers can evaluate their prescribing habits and implement antibiotic stewardship activities, such as watchful waiting or delayed prescribing, when appropriate, into their practices.
- Health systems can improve antibiotic prescribing in offices and outpatient facilities within their networks by providing communications training, clinical decision support, patient and health care provider education, and feedback to providers on their performance.
- Patients can talk to their health care providers about when antibiotics are needed and when they are not. These conversations should include information on patients’ risk for infections by antibiotic-resistant bacteria.
Congress has recognized the urgent need to combat antibiotic resistance. In fiscal 2016, Congress appropriated $160 million in new funding for CDC to implement its activities listed in the National Action Plan for Combating Antibiotic-Resistant Bacteria.
With this funding, CDC is fighting the spread of antibiotic resistance by:
- Accelerating outbreak detection and prevention in every state.
- Enhancing tracking of antibiotic use and resistance mechanisms and resistant infections.
- Supporting innovative research to address gaps in knowledge.
- Informing providers and the general public about antibiotic resistance and appropriate antibiotic use.
- Improving antibiotic use by supporting expansion and development of new programs and activities at the local level.
Information on antibiotic stewardship and appropriate antibiotic use for health care providers and patients can be found at www.cdc.gov/getsmart.