Remarkable progress made reducing kidney failure from diabetes in Native American populations
Success suggests ways to prevent kidney failure, lower U.S. health costs
Press Release
Embargoed Until: Tuesday, January 10, 2017, 2:30 p.m. ET
Contact: Media Relations
(404) 639-3286
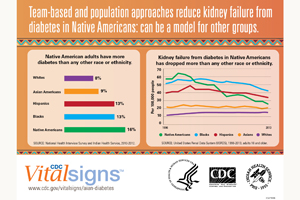
Federal data show diabetes-related kidney failure among Native American adults (American Indians/Alaskan Natives) decreased 54 percent between 1996 and 2013. This remarkable decrease follows population-based approaches to diabetes management and improvements in clinical care begun by the Indian Health Service (IHS) in the mid-1980s.
“The Indian Health Service has made tremendous progress by applying population health and team-based approaches to diabetes and kidney care,” said CDC Director Tom Frieden M.D., M.P.H. “Strong coordinated clinical care and education, community outreach and environmental changes can make a dramatic difference in reducing complications from diabetes for all Americans.”
Native Americans have a greater chance of having diabetes than any other U.S. racial/ethnic group. Diabetes is the leading cause of kidney failure in the U.S. About 2 in 3 Native Americans with kidney failure have diabetes, according to this month’s Vital Signs. But the rate of diabetes-related kidney failure in Native Americans has declined the fastest of any racial/ethnic group in the U.S.
Kidney failure is a devastating and costly condition that requires regular dialysis or a kidney transplant for survival. According to the Vital Signs report, the estimated yearly cost in 2013 of kidney failure from diabetes was $82,000 for one person and $14 billion for Medicare overall. Diabetes-related kidney failure is delayed or prevented by controlling blood pressure and blood sugar, using kidney-protective medicines, and regular kidney testing.
“The 54 percent decline in kidney failure from diabetes followed implementation of public health and population approaches to diabetes as well as improvements in clinical care by the IHS,” said Mary L. Smith, Indian Health Service principal deputy director. “We believe these strategies can be effective in any population. The patient, family, and community are all key partners in managing chronic diseases, including diabetes.”
Key Findings from the report include:
- Despite well-documented health and socioeconomic disparities in the Native American population, kidney failure from diabetes has decreased substantially since 1996.
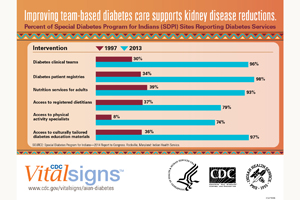
- IHS-supported care for Native Americans with diabetes has improved:
- Use of medicine to protect kidneys increased greatly, from 42 percent to 74 percent in 5 years.
- Average blood pressure in Native Americans with diabetes and hypertension is well controlled (133/76 in 2015).
- Blood sugar control improved by 10 percent between 1996 and 2014.
- More than 60 percent of Native Americans with diabetes 65 years and older had a urine test for kidney damage (2015) compared to 40 percent of the Medicare diabetes population (2013).
The Federal Government is supporting the fight against kidney failure in Native Americans and other U.S. populations by:
- Funding diabetes treatment and prevention services in Native American communities through the Special Diabetes Program for Indians.
- Developing a national system for tracking chronic kidney disease and its complications.
- Helping community health centers throughout the U.S. provide comprehensive diabetes care.
To read the entire Vital Signs report, visit: www.cdc.gov/vitalsigns/aian-diabetes.
For more information on the Indian Health Service and CDC’s work, visit: www.ihs.gov and www.cdc.gov.
About Vital Signs
Vital Signs is a report that appears as part of the CDC’s Morbidity and Mortality Weekly Report. Vital Signs provides the latest data and information on key health indicators: cancer prevention, obesity, tobacco use, motor vehicle passenger safety, prescription drug overdose, HIV/AIDS, alcohol use, health care-associated infections, cardiovascular health, teen pregnancy, food safety, and viral hepatitis.