Transcript for CDC Update on Flu Activity
Press Briefing Transcript
Friday, February 2, 2018
Audio recording [MP3, 6.0 MB]
Please Note: This transcript is not edited and may contain errors.
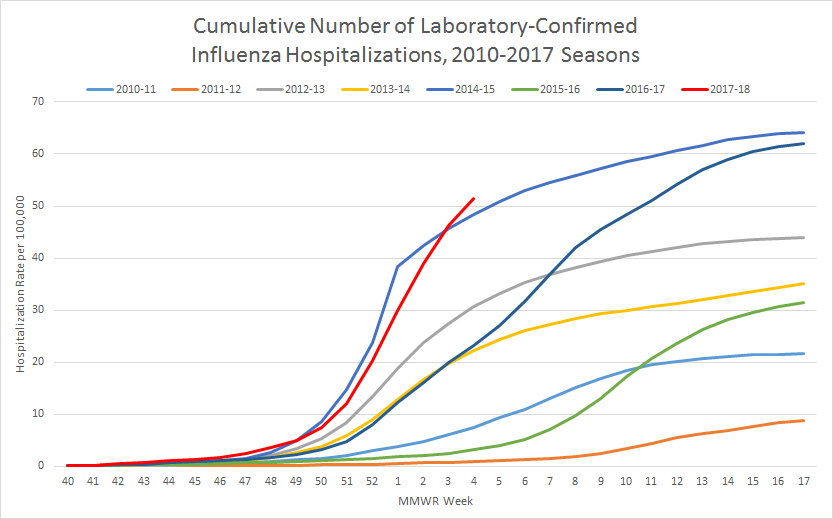
This is a line graph entitled “Cumulative Number of Laboratory-Confirmed Influenza Hospitalizations, FluSurv-NET, 2010-2017 Seasons.” The hospitalization rate per 100,000 is shown on the Y-axis, and it scales from 0 to 70. The MMWR week is shown on the X-axis, and it scales from week 40 to 52, and then from week 1 to 17. Across the top of the graph, a color-coded key is provided to denote which line of the graph refers to which flu season. Data from eight flu seasons are included, beginning with the 2010-2011 flu season and ending with the 2017-18 flu season. A sky blue line represents the 2010-2011 season. An orange line represents the 2011-2012 season. A gray line represents the 2012-2013 season. A yellow line represents the 2013-2014 season. A blue line represents the 2014-2015 season. A green line represents the 2015-2016 season. A dark blue line represents the 2016-2017 season, and a red line represents the 2017-2018 season. The season with the lowest final cumulative rate of laboratory-confirmed influenza hospitalizations is the 2011-2012 season, which had a rate of 8.7 per 100,000. The season with the highest final cumulative rate of laboratory-confirmed influenza hospitalizations is the 2014-2015 season, which had a rate of 64.2 per 100,000. As of week 4, the influenza hospitalization rate for the 2017-2018 season has surpassed the week 4 hospitalization rate for the 2014-2015 season. The hospitalization rate for the 2017-2018 season is currently at 51.4 per 100,000. In comparison, the hospitalization rate during week 4 of the 2014-2015 season was 48.4 per 100,000. The cumulative hospitalization rates per 100,000 for the remaining seasons break down as follows from lowest to highest hospitalization rate: the 2010-2011 season was 21.7; the 2015-2016 season was 31.5; the 2013-2014 season was 35.1; the 2012-2013 season was 44.0; and the 2016-2017 season was 62.0. These hospitalization rates are not adjusted for testing practices, which can vary from season to season; caution should be used when comparing hospitalization rates across seasons.
KATHY HARBEN: Thank you all for joining us today. There continues to be great interest in this flu season. Today we will provide the latest fluview numbers as well as advice on preventing the flu and what you can do to reduce the risk of flu or serious illness. We’re joined by CDC acting Director Dr. Anne Schuchat and also by Dr. Dan Jernigan, Director of the Influenza Division in our National Center for Immunization and Respiratory Diseases. They will both address questions after the briefing. I’ll turn the call over now to Dr. Schuchat.
ANNE SCHUCHAT: Good morning and thank you for joining us. Before we get started, I just want to the say that despite recent leadership changes, CDC remains committed to our 24/7 mission to protect the health, safety and security of Americans. And that mission will not falter. Right now, one of the biggest health threats we are facing is influenza. Flu is incredibly complex and difficult to predict and this season is a somber reminder of why flu is one of the world’s greatest public health challenges. And why we at CDC focus so intensely on efforts to fight flu. In the past week, we have seen increased influenza-like illness activity, more hospitalizations, and tragically, more flu associated deaths in children and adults. And as of this week, overall hospitalizations are now the highest we’ve seen. even higher than the 2014-’15, our previous high season. We also continue to hear reports of crowded hospitals and spot shortages of antiviral medications and rapid influenza tests. Unfortunately, our latest tracking data indicate that the flu activity is still high and widespread across most of the nation. and increasing overall. Influenza A H3N2 viruses continue to dominate this season. However, we are seeing other flu viruses including H1N1, and influenza B causing illness, as well. And in some cases, disproportionately affecting certain age groups. I know many of you are concerned about this flu season and have seen the heart breaking stories of those who have lost loved ones.
This week, we are reporting an additional 16 flu related pediatric deaths for this season. Meaning there are even more families now devastated by flu. That means we’ve received reports for a total of 53 children who have died of the flu so far this season. I also know there are ongoing concerns about whether the flu vaccine that many people received will be effective or whether you’ll be able to fill a prescription for antiviral medicine. While we don’t have all the answers, here’s what I can tell you. We continue to recommend the flu vaccine even though we know most flu vaccines have low effectiveness against H3N2 viruses, effectiveness against other flu viruses is better, and there is more than one flu virus circulating this season. The vaccine may also reduce the severity of symptoms if you catch the flu in spite of being vaccinated, and it is not too late to get the vaccine. As of January 12th, more than 152 million doses of flu vaccine have been shipped nationwide. I also want to mention vaccine against pneumococcal pneumonia. Some of the serious consequences of influenza are bacterial pneumonias. Viral infections like flu can make people more vulnerable to secondary bacterial infections and we recommend people 65 years of age and over get vaccinated against a common pneumonia caused by pneumococcus. You also can reduce your risk of getting the flu through every day measures. Please stay home if you are sick to help prevent spreading respiratory viruses to others.
We also recommend you frequently wash your hands and to reduce spreading infections cover your mouth when you cough or sneeze. Antiviral medications are another tool in the fight against flu. And can be used for treatment. they can help reduce symptoms and shorten how long you are sick. Most people who get flu have mild illness and will get better without medical care or antiviral drugs. However, those who obviously are very sick or at high risk of developing serious flu complications should be treated as soon as possible with antiviral drugs. Remember that young children, people 65 and older, pregnant women, and people with heart or lung disease have a particularly hard time with the flu. CDC has received reports of anti-viral drug shortages in some places that are experiencing high influenza activity. However, the manufacturers say there is product available. Pharmacists may want to increase supply on their shelves and patients may have to call more than one pharmacy to fill their prescription. There is a little good news this week. For the second week in a row, there are signs that activity in the west may be easing up. However, we are by no means out of the woods. Most seasons last up to 20 weeks and we’ve probably got several weeks left of increased flu activity. I want you to know that CDC continues to make flu monitoring and control a priority, helping Americans whether this season is our focus, but we are also working with partners across government and the private sector tore improve the vaccines that we have and find ways and tools to help Americans reduce their risk of getting sick. I want to turn things over to Dr. Jernigan how who give you more details about the latest activity.
DR DAN JERNIGAN: Thank you very much. So as dr. Schuchat has stated this season is turning out to be a particularly challenging one. And it has been compounded by lots of flu occurring nationwide simultaneously over several weeks. this is an unusual pattern for flu in the U.S. but let me just walk through the data that we have so far for this week. These data reflect the experiences of patients and health care providers as of last Friday January 27th. So first let me just talk about how widespread it is, where the flu is occurring. We get reports each week from state health departments about how widespread influenza is across their cities and counties. For the prior three weeks, we had 49 states with the widespread activity, which is something we hadn’t seen since we have been collecting these data. This week, 48 states are still reporting widespread activity. Oregon is the one state that is reporting less influenza activity across the state and we hope it represents a trend we’re seeing of decreasing activity in the west. Let me talk a little bit about what is being seen in doctor’s offices and in emergency departments. We work with 2800 doctors’ offices and emergency departments who obviously report the percent of patients that they are treating with influenza-like illness. For this week, influenza-like illness has increased again. Last week, the number of people even in the clinic that had influenza-like illness was 6.6%. This week it is 7.1%. We’ve had two seasons in the last 15 years that were higher than that. The first was the 2009 H1N1 pandemic, which peaked at 7.8% and the 2003-2004 season, which was a high severity H3N2 season, which peaked at 7.6%. When you look at flu activity at the state level, this week, the number of states experiencing high influenza-like illness activity increased from 39 to 42. In general, for doctors’ offices urgent care clinics and emergency departments, the western part of the country is beginning to see lower flu activity; the eastern part of the country is seeing somewhat higher activity. And southern states are continuing to see high activity at the same levels. Influenza-like illness has been elevated for ten consecutive weeks so far this season. And we know from past information and from following the system that the average duration of a flu season in this network over the last five seasons has been 16 weeks. But it has ranged from 11 to 20 weeks. So there may be many weeks left for this season to go. in terms of hospitalizations where we try and measure the impact on illness, the individual illness and on the population, we collect information about laboratory confirmed influenza hospitalizations in 13 states in the U.S. representing a population of around 9% of the total U.S.. for the past few weeks, we have been watching this season’s hospitalizations track closely with the 2014-’15 season. That 2014-’15 season was characterized as high severity and had an estimated 710,000 hospitalizations by season’s end. this week, we’re reporting a cumulative hospitalization rate of 51.4 which is higher than was seen for this same week during the 2014-’15 season when it was 43.5. if this current trend in hospitalization rates is maintained through the season, it is possible that the number of flu hospitalizations may well exceed 710,000 that was seen in 2014-’15. The highest rates are again overwhelmingly in people aged 65 years and older. People that are 50 to 64 years of age have the next highest rates followed by children that are younger than 5 years. For those that are the young children, we see that about half of those that are being hospitalized have no underlying condition that puts them at higher risk for being hospitalized. We’re still seeing significantly higher hospitalization rates in some states and while reports of new hospitalizations were lower in the last week, the cumulative hospitalization rates in California, for example, are again about four times higher than they were in 2014-’15 and in Oregon and Minnesota, they are double what they were double what they were in 2014-’15. We also have information about pediatric deaths due to influenza, and we receive those reports each week.
This week as Dr. Schuchat mentioned an additional 16 pediatric deaths were reported. The last time that we had this many per week was in 2014 ’15. For this season, only around 20% of these pediatric deaths had been vaccinate and half of these children were otherwise healthy. these deaths are associated with influenza A H3N2, H1N1 viruses as well as influenza b viruses so all the different types of influenza are causing these deaths. Pediatric deaths became nationally notifiable in 2004, and since that time, they’ve ranged from 37 to 171 during regular seasons. The highest was during the 2009 pandemic where 358 pediatric deaths were reported. Looking at adult mortality, we track deaths due to pneumonia and influenza as listed on death certificates across the country. The number of deaths due to pneumonia and influenza increased again over the last week from 9.1% up to 9.7%. This is not as high as the season’s 2012’13 and 2014 ’15 where they peaked at 11.1 and 10.8 but it is possible that this season will reach or surpass those two severe seasons. Finally, CDC characterizes a number of viruses. We support surveillance at state public health labs where they have tested around 45,000 respiratory specimens so far this season. The majority, 76% of those specimens, are H3N2. CDC along with five other W.H.O. designated laboratories, have evaluated the currently circulating H3N2 viruses and do not see evidence that the virus has significantly drifted. However, we do see that the viruses prepared for uses in egg-based vaccine manufacturing have adaptations that make them less similar to the circulating H3N2 viruses. With that I’ll stop.
KATHY HARBEN: Thanks very much. Dr. Jernigan. Terry, we are now ready for questions.
OPERATOR: as a reminder to ask a question, please press star 1 on your touch tone phone and record your name at the prompt. Please be sure that your line is unmuted and record your name at the prompt. Okay? First we have first we have David Lewkowict from Fox news. Your line is open.
DAVID LEWKOWICT: Thank you very much for taking the call. A few quick questions. One is where are we on a universal vaccine? And two, do we see any increase numbers in GBS this season?
ANNE SCHUCHAT: Thank you for those questions. There’s a lot of interest in developing influenza vaccines that have broader and potentially more long lasting protection. NIH is leading the government efforts on that and CDC is one of the keen partners in that. We have some promising research but I would say that we do need to keep focusing on the vaccines we have while we invest in developing that long-term goal of a universal vaccine. The question about Guillain-Barre Syndrome, I’m not aware of increasing reports of that. We can look into that. The approach is to surveillance for that are somewhat different than our routine flu tracking and today’s update is really focused in on the influenza measurements that we’re tracking but thank you for that question. Next question, operator.
OPERATOR: Next, we have Dan Childs of ABC news. Your line is open.
DAN CHILDS: Thank you so much for taking my question. We saw earlier this week that researchers in Canada are saying that this year’s flu vaccine has only been 10 to 20% effective against the dominant H3N2 strain at least in Canada. How reflective do we think that this is of the U.S. situation? I have one follow-up after this.
ANNE SCHUCHAT: Sure. You know, the news from Canada is quite similar to what Australia reported. CDC is working with several states to do vaccine effectiveness, as well. We hope to provide the U.S. experience over the next couple weeks. We’ll hope over the course of the season to be able to look closely at the effectiveness for the different types potentially for different age groups and so forth. This is consistent with our concern that the H3N2 influenza vaccine effectiveness is lower than against other types and that in recent years it’s been more challenging to even get effective H3N2 protection. So your follow-up question?
DAN CHILDS: Yes, thank you so much. Basically, I was also wondering more along the lines to what you said about the egg-based vaccines will this season’s experience provide momentum for transition to cell based flu vaccines and could such a transition have averted illness and saved lives this season in your opinion?
ANNE SCHUCHAT: It’s very important that we measure the effectiveness of different kinds of vaccine. CDC has increased our investment in effectiveness measurement so we can look at different age groups, different types of vaccine as well as different types of flu and we don’t yet have comparative effectiveness for vaccination with a cell-based or recombinant vaccines. That’s a question many are asking. I know that we have a larger supply of egg-based vaccines right now. and the question of whether other formulations will be more protective or whether we would be able to avoid these egg adapted changes through new approaches to selecting strains. I’m going to let Dr. Jernigan add anything if he would like about the specifics of the egg adapted concerns.
DAN JERNIGAN: yes. so this is something that we have been following for several years. It’s something that has developed incrementally over time. So it is a problem with this H3N2 especially that when you take these viruses and try and get them to grow in eggs they make changes that make it very difficult for them to stay looking similar to what is actually out there circulating. So this is a problem with the current viruses that we have. So trying to find better ways to do that is certainly something we’re doing and we are also helping to support by developing cell based candidate vaccine viruses that don’t have those egg adapted changes. But as those technologies go forward, we will continue to validate them and evaluate them, as well.
ANNE SCHUCHAT: Thank you. Next question, operator.
OPERATOR: Next, we have Sarah Troy from the Wall Street Journal. Your line is open.
SARAH TROY: Hi, thank you for taking my question. first I just wanted to ask how common is it for flu to keep rising for this long at this point in the season and secondly, did you expect it to peak at this point?
ANNE SCHUCHAT: The flu is incredibly difficult to predict and as we said, that flu seasons can range from 11 to 20 weeks. The peak is at different points in different years and so this we, of course, do not know if we have hit the peak yet. Many of the measurements are still going up. but we’re at week ten and some seasons go to 20 weeks, i would say the timing is not particularly unusual. what is unusual is the hospitalizations are greater than we’ve been seeing in the past several years. Next question, operator.
OPERATOR: We have Mike Stobbe from The Associated Press. Your line is open.
MIKE STOBBE: Hi. Thank you for taking my question. first, CDC officials in recent weeks had said that regarding vaccine effectiveness that it was possible or even probable that the effectiveness would end up in the 30% to 40% range as it was judged to be last year. I was wondering if I know it’s a couple weeks till you present the final numbers but are you still thinking the 30 to 40 range or have you — I wanted to ask just to clarify, Dr. Schuchat I believe you said something about the hospitalization is the highest ever. Did you mean the highest since 2009, the pandemic year or highest including 2009? Would it be even higher than that pandemic year. Thank you.
ANNE SCHUCHAT: Thank you for the question. It’s important with a vaccine effectiveness estimates to know whether we’re talking about the total or against a particular strain. We have been expecting low effectiveness against the H3N2 strains. And it’s too soon in the season for us to be sure how things will all end up because we are seeing increases in the h1n1 and b components where the vaccine effectiveness is often higher. so I can’t say that I’m surprised about the Canada data but I can say that CDC is working hard to develop robust estimates for the interim look at effectiveness that we hope to release in the weeks ahead. it’s very important that we measure every year and that we learn from the experience and work on improving vaccines. in terms of the highest comment that i made, what we’re saying is so far this year, the cumulative rate of hospitalizations is the highest since we’ve been tracking in this way. which goes back to 2010. in terms of 2009-’10, the pandemic year, that was very high for influenza-like activity. but it wasn’t our peak for hospitalizations because as you remember, we had a relative sparing of the elderly and the elderly account for quite a large proportion of hospitalizations. so I believe on our website, we’re going to have a graph that you may want to take a look at that shows that so far this year, the 2017-’18 season just crossed the hospitalization curve that the 2014-’15 season used to hold the record of. it’s a lot easier to see this than to explain it. So I encourage you to take a look at that graph. again, it’s not end of season hospitalizations and things could level out and we might not have as bad a year as ’14-’15 but as of this week it was pretty bad news to see that hospitalization. Operator, next question.
OPERATOR: next we have Susan Scutti from cnn. your line is open.
SUSAN SCUTTI thank you for taking my call. Has CDC received reports of side effects caused by Tamiflu or antiviral medications?
ANNE SCHUCHAT: Thank you for that question. there’s quite a literature on the adverse events that follow use of antiviral medicines and there’s been a lot of look at the benefits and risks of these medicines. and we – we recommend antiviral medicines for people who have severe presentations of influenza and for people who are at high risk to have complication from getting influenza like young children and older adults and pregnant women, for instance. the common side effects of antiviral medicines are nausea and vomiting. and those kind of consistently show up in the different trials. The fears about very severe side effects of antivirals to my knowledge haven’t really held up to robust examination. so it’s not — we think at this point for people who are at risk for severe problems with influenza particularly when the treatment can begin relatively soon that antivirals are recommended. Next question, operator.
OPERATOR: Next, we have Kathleen Doheny from Web MD. Your line is open.
KATHLEEN DOHENY: Thank you. we’ve been hearing reports that emergency rooms at children’s hospitals are kind of overrun with parents and there’s risk of exposure. what should parents consider and do before considering before going to the ER with their sick kid?
ANNE SCHUCHAT: Thank you for that question. one thing to say is that our vaccination rates in children are a bit higher than in other populations and so far the hospitalizations in children are tracking lower than the 2014 ’15 season while, of course, it’s too soon to know where we’ll end up. But it is important to take steps to protect yourself and not spread to others when you enter the emergency room. Most emergency rooms these days have masks right at the door where you can put a mask on if you’re coughing. The masks are really for you to protect yourself from spreading to someone else. Washing your hands frequently of course, that’s a good idea for children all the time. we hope parents are reminding their kids about frequently washing their hands. That can help you spread germs from yourself to someone else or pick up a germ that’s around you. but the issue of the worried well flocking the emergency rooms may not be a great idea. so if you’re not sure if you need to go to the emergency room or the urgent care, you know, call ahead. but again, the principal thing for parents of young children is that you’ll want to, that if they’re coughing, a mask will help them from spreading and that we hope that folks are staying away who obviously don’t need to be clogging up the emergency room.
KATHLEEN DOHENY: Can you provide though a list of symptoms about how bad should your kid be before you head to the ER or not call the doctor or the advice nurse at the desk?
ANNE SCHUCHAT: it’s so important for people to speak with their health care provider about their child but in general, worrisome signs are a very high persisting fever, difficulty breathing or shortness of breath, rapid heart beat or shallow rapid breathing, or significant tiredness or confusion. in theory young children those kind of symptoms are going to be difficult to assess so we really do think a call to the pediatrician or nurse hotline is very important. but in general, healthy adults tend to do okay. but these kinds of worrisome side effects another one i want to mention is getting better and then suddenly getting worse. that can indicate that you have one of those secondary bacterial pneumonias and that can be a bad emergency. you don’t want to feel like you’re getting better and then suddenly you’re not, you’re getting worse. you really want to seek attention if that’s happening. Next question?
OPERATOR: Next we have Jamie Ducharme from “time” magazine.
JAMIE DUCHARME: thank you. My question is somewhat related. it seems liking there have been a number of cases this year of especially children who obviously don’t seem like they have a particularly severe disease and then it progresses quickly and they end up dying. What would you say to parents who obviously are worried about that happening to their own child?
ANNE SCHUCHAT: You know, unfortunately, we’re seeing flu serious influenza in children who really have no underlying conditions. About half of the cases of hospitalizations for influenza in children are occurring in previously healthy children. Including those who are very young. but we do think those warning signs of difficulty breathing of very high fever, rapid breathing, those are clues to call the doc. and as i said, you’re getting better and then the child’s getting worse. that is a very worrisome sign. I think we have time for one last question. operator if there is one.
ANNE SCHUCHAT: it’s okay if there isn’t one.
OPERATOR: Okay. One moment. We have Dennis Thompson in health bay. Your line is open.
DENNIS THOMPSON: thank you for taking my question. i wanted to ask a follow-up about that new study out of Canada that it estimates that the flu vaccine’s effectiveness is only about 17%. but then they add that the result was not statistically significant. Should we take that report seriously even though it didn’t meet statistical significance?
ANNE SCHUCHAT: It’s important in vaccine effectiveness studies to recognize that there are uncertainties and when we give a number 17, 30, 50, it’s an estimate with a range around it. so the, this time of year most of the investigators are looking at interim estimates and I believe Canada will continue to look and have a final estimate for their season. we’ll be providing an interim estimate in a couple weeks. i think it’s important to say that we expect that the effectiveness against the H3N2 strains will be low. that’s what they saw in Australia at the end of the season. but we don’t have that final number yet. but to say that consistently we’ve seen higher effectiveness against the other types so because we’re continuing to see all three main types circulate and we’re seeing increases in fact in the U.S., it’s not too late to be vaccinated if you haven’t gotten vaccinated yet. and so again, there’s uncertainty a single number doesn’t really tell the whole story but we know that H3N2 vaccine effectiveness is lower year in and year out.
DENNIS THOMPSON: just a follow-up. You know, in terms of us coming up with our own U.S. estimate, what are the chances that the U.S. estimate would deviate much from the Canadian estimate since you know, there’s really a lot of cross border movement?
ANNE SCHUCHAT: It’s not really whether the vaccines are different or the performance is different. it’s a question of the size of the sample. i think what you’re saying is that Canada and the U.S probably have a pretty similar flu season and are using the same kinds of vaccines. so yes, we’re going to expect to be in the same range but the precision will depend on the larger numbers and just that mix of the H3N2, h1n1 and b strains. so I’m not surprised at their result which is quite similar to Australia’s and I think we’ll just have to see ours and again we’ll be sharing an interim result and then an end of year result much later in the year. so thank you all for joining us this morning. it’s still morning. thank you for joining us this morning. i just want to conclude by saying this is a very difficult season. the hospitalization rate is the highest that we’ve seen. we aren’t out of the woods yet, but there are steps that everyone can take to fight the flu. so thank you for calling in and thank you for what you’re doing.
KATHY HARBEN: thank you Dr. Schuchat and Dr. Jernigan and thank you also to the reporters who have joined. If you have follow-up questions, you can call us at 404-639-3286. or you can send us an e-mail at media@CDC.gov. Thank you for joining us. This concludes our call.