CDC update on widespread flu activity
Press Briefing Transcript
Friday, February 9, 2018
Please Note: This transcript is not edited and may contain errors.
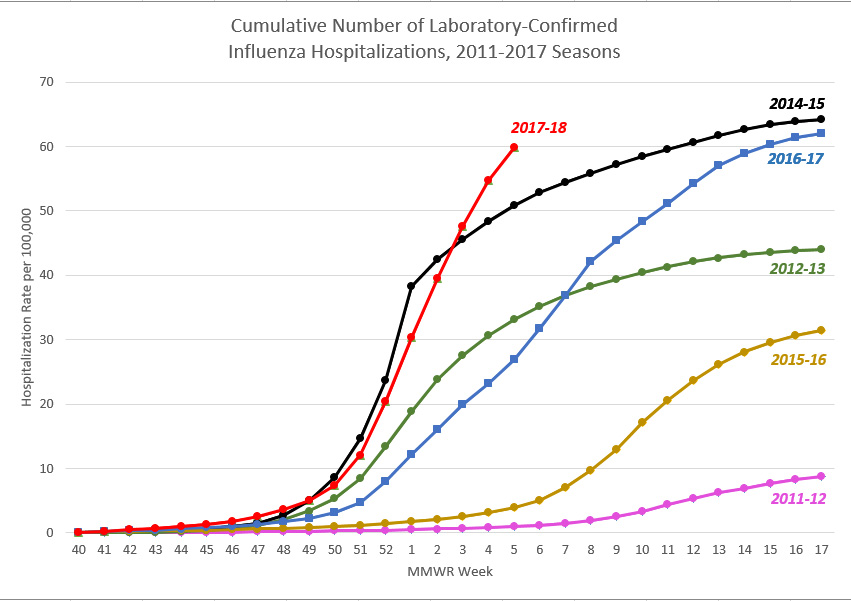
This is a line graph entitled “Cumulative Number of Laboratory-Confirmed Influenza Hospitalizations, FluSurv-NET, 2010-2017 Seasons.” The hospitalization rate per 100,000 is shown on the Y-axis, and it scales from 0 to 70. The MMWR week is shown on the X-axis, and it scales from week 40 to 52, and then from week 1 to 17. Across the top of the graph, a color-coded key is provided to denote which line of the graph refers to which flu season. Data from eight flu seasons are included, beginning with the 2010-2011 flu season and ending with the 2017-18 flu season. A sky blue line represents the 2010-2011 season. An orange line represents the 2011-2012 season. A gray line represents the 2012-2013 season. A yellow line represents the 2013-2014 season. A blue line represents the 2014-2015 season. A green line represents the 2015-2016 season. A dark blue line represents the 2016-2017 season, and a red line represents the 2017-2018 season. The season with the lowest final cumulative rate of laboratory-confirmed influenza hospitalizations is the 2011-2012 season, which had a rate of 8.7 per 100,000. The season with the highest final cumulative rate of laboratory-confirmed influenza hospitalizations is the 2014-2015 season, which had a rate of 64.2 per 100,000. The week 5 influenza hospitalization rate for the 2017-2018 season is higher than the week 5 hospitalization rate for the 2014-2015 season and approaching the cumulative overall end-of-season hospitalization rate for 2014-2015. The hospitalization rate for the 2017-2018 season is currently at 59.9 per 100,000. In comparison, the hospitalization rate during week 5 of the 2014-2015 season was 50.9 per 100,000. The cumulative hospitalization rates per 100,000 for the remaining seasons break down as follows from lowest to highest hospitalization rate: the 2010-2011 season was 21.7; the 2015-2016 season was 31.5; the 2013-2014 season was 35.1; the 2012-2013 season was 44.0; and the 2016-2017 season was 62.0. These hospitalization rates are not adjusted for testing practices, which can vary from season to season; caution should be used when comparing hospitalization rates across seasons.
OPERATOR: Welcome and thank you for standing by. Your mics have been placed on listen only mode until the question and answer session. At that time if you would like to ask a question, you may press star followed by one. Today’s conference is being recorded. If you have any objections, you may disconnect at this time. Now, I’ll turn the call over to Kathy Harben. You may begin.
KATHY HARBEN: Thank you, Shirley, and thank you all for joining us today. There continues to be great interest in influenza. Today we’ll provide the latest Fluview numbers, and advice on preventing the flu and what people can do to reduce the risk of flu or serious illness. We’re joined by CDC Acting Director Dr. Anne Schuchat and we’re also joined by Dr. Alicia Fry of the influenza Division in CDC’s National Center for Immunization and Respiratory Diseases. They will both address questions following our briefing. I’ll now turn the call over to Dr. Schuchat.
ANNE SCHUCHAT: Good morning – and thank you for joining us. We were hoping to have better news to share today, but unfortunately, it looks like this flu season continues to be particularly challenging. Our latest tracking data indicate that influenza activity is still on the rise overall. In fact, we may be on track to beat some recent records. Before getting into the specifics, I just want to recognize that we know this issue is personal to so many Americans, and that there is a lot of fear and alarm about this flu season. There have been far too many heart-wrenching stories in recent weeks about families who have lost loved ones to influenza. And unfortunately, this week’s report reveals more somber news, with an additional 10 flu-related pediatric deaths for this season. That means we have now received reports for 63 children who have died of the flu so far this season. I also know many of you are asking how this season compares to previous ones and how much longer it will go on. But flu is incredibly difficult to predict, and we don’t know if we’ve hit the peak yet. In the past five seasons, influenza-like Illness has been elevated for between 11 and 20 weeks, and we’re only at week 11 now, so we could potentially see several more weeks of activity. Here’s what we can tell you, based on the latest data. Levels of influenza-like-illness across the country are now as high as we observed at the peak of the 2009 H1N1 pandemic. This doesn’t mean that we are having a pandemic, just that levels of influenza-like-illness are as high as what we saw during the peak of H1N1. That’s a signal of how very intense this flu season has been. And let me remind you that the influenza like illness measure is based on outpatient visits and emergency department visits. In addition, overall hospitalizations are now significantly higher than what we’ve seen for this time of year since our current tracking system began almost a decade ago in 2010 and the rate is approaching the final rate of hospitalizations that we observed at the end of the active 2014-2015 flu season. That was our recent severe season. There’s a graphic on our news media site that shows those hospitalizations in comparison with previous seasons. You’ll see there that we have not just crossed a line for 2014-15, but we’re quite a bit higher. The proportion of deaths attributed to pneumonia & influenza is 10.1 percent this week. That means one out of 10 people who died in the week that has passed died from influenza or pneumonia. Influenza A H3N2 viruses continue to dominate this season and these viruses are often linked to more severe illness, especially among children and people age 65 and older. However, we are seeing an increasing proportion of B viruses circulating, as well as a smaller increase in the proportion of H1N1 viruses. Last week, B strains made up 30 percent of the tested viruses. We actually usually see better vaccine protection against these. This week, 48 states are still reporting widespread geographic influenza activity. Oregon and Hawaii are reporting regional or less widespread activity. Last week we reported that part of the West coast were seeing declines in flu activity. This is still true for H3N2 viruses, but some Western states are beginning to see an increase in influenza B activity. It’s not uncommon for there to be second waves of influenza B activity during an influenza season. In past seasons similar to this one, an estimated 34 million Americans have gotten sick with flu. Now, I’d like to talk about preventative steps, because it’s important to remember that there are ways to reduce your risk of getting sick, which can be crucial in a season like this one We continue to recommend getting the flu vaccine to prevent flu. I know there are ongoing concerns about whether the flu vaccine is effective this year, and it’s true that flu vaccines often have lower effectiveness against H3N2 viruses. However, some protection is better than none. Plus, the vaccine’s effectiveness against other flu viruses, like B and H1N1, is better. Because of the ongoing intensity of the flu season and the increasing circulation of influenza B and H1N1, we continue to recommend vaccination even this late in the season. I also want to reiterate the importance of the pneumococcal pneumonia vaccine. Flu can make people more vulnerable to secondary infections like bacterial pneumonia, so we recommend people 65 and over get the pneumococcal pneumonia vaccine. Most children have already been vaccinated against pneumococcal disease from shots they got when they were infants or toddlers. While we need to get flu vaccines every year because the viruses keep changing, the pneumococcal vaccines are more long-lasting. You also can help reduce the spread of flu through simple good health habits, like staying away from people who are sick, frequently washing your hands and covering your cough and sneeze. For those who are already sick, please stay home from work or school. That is such an important recommendation to follow. Otherwise you run the risk of spreading the virus to others – and what may be mild symptoms to you could be deadly to someone else. Antiviral medications are an important tool for treatment. Now its important to remember that most people with flu will feel ill and should stay home from school or work, but most of them won’t need to see a doctor, won’t need to be tested, and won’t need to get antiviral drugs. Antiviral medicines are recommended for people who are very sick with flu or people who are at high risk of serious flu complications who develop flu symptoms. People at higher risk of developing serious flu complications, include those who are very young, very old, pregnant women and people with conditions like heart or lung disease. Clinicians don’t have to wait for confirmatory flu testing, and should begin treatment with antiviral drugs immediately if they suspect flu in a severely ill or high-risk patient. There is a lot of flu out there right now. If it looks like flu, it probably is. Antivirals could mean the difference between a milder illness and a hospital stay or worse. And they work better if they are started earlier. There’s been a lot of interest in the availability of antiviral drugs. Although we know there have been spot shortages in some places experiencing high influenza activity, manufacturers say there is product available. For patients, that might mean calling more than one pharmacy to fill a prescription. Staff here at CDC have been working closely with the commercial supply chain and pharmacies to address gaps in the market and increase access to brand product when the antiviral generics aren’t available. We appreciate the efforts of suppliers, pharmacies, and insurers to try to smooth things out for consumers. I also want to talk about some of the more severe symptoms that families should watch out for, because it’s important to understand that the flu isn’t just sniffles and a cough. The more severe symptoms include a persistent high fever, difficulty breathing or shortness of breath, a rapid heartbeat and significant tiredness or confusion. Another severe symptom is this: you start to get better, and then suddenly you feel much worse. That could indicate a secondary bacterial pneumonia, and you should seek medical attention immediately if that’s happening. I know it can be difficult to assess those symptoms, especially in young children. About half of the cases of hospitalizations for influenza in children have occurred in previously healthy ones with no underlying conditions. That’s why we strongly recommend parents get their children vaccinated each year against the flu. It’s important for parents to speak with a healthcare provider at the first sign of trouble. Flu continues to be a priority for CDC and we are working 24/7 to protect Americans from it. This is a difficult season, and we can’t predict how much longer the intense flu activity will last. But if we all stay vigilant and take steps to fight the flu, we can help reduce the risk of getting – and transmitting – it. Now I will turn to the moderator for questions.
KATHY HARBEN: Thank you Dr. Schuchat. We are now ready for questions Shirley.
OPERATOR: We will now begin the question and answer session. If you would like to ask a question, please press star followed by one. You will be prompted to record you name. To withdraw your question, you may press star followed by two. Again, press star followed by one to ask a question and one moment please for our first question. Our first question comes from Helen Branswell with STAT. Your line is open. You may ask your question.
HELEN BRANSWELL: Thank you very much. Dr. Schuchat, you said in your intro that this year’s season is breaking some records. I know it’s hard to compare one season to another, but can you give us a sense of why you say that? How when you stack this up against previous years is this such a bad year? At this point, what is the year prior to this that you would use as a comparator?
ANNE SCHUCHAT: Yes, thank you Helen. There are a couple of questions in there. Influenza-like illness activity of the most recent week is at 7.7 percent. The previously recorded high for that, in that system was 7.6 percent for a non-pandemic year. That was in 2003-04, where you’ll all remember we saw a very difficult year. An early year, hard on kids, new strain and so forth. So ILI is now at the same level as that peak week of the H1N1 pandemic. The second record situation is in terms of hospitalization. I need to caveat that with the systems of tracking hospitalizations like this really started in 2010, so we can’t go back all the way to 2003-04. One of the areas that we’re really seeing unusual levels of hospitalizations is in non-elderly adults. So far this year we’ve seen 63.1 per hundred thousand people in the 50 to 64 age group being hospitalized by flu. In 2015-16, that number was 35.1. So that’s our most recent severe season and we’re quite a bit higher than that. As I say, we’re on track now with the overall number of 59.9 hundred thousand hospitalizations overall. We’re on track to exceed the or be similar to the end of year rate of hospitalizations for 2014-15. We don’t have any signs of hospitalizations leveling off yet. So, the information on pneumonia and influenza deaths is consistent with similar severe years, but I would say the hospitalizations and that under younger age groups, as well as, the higher level of ILI are where the records are. The other thing to say is that it’s just week 11 and the [inaudible] are increasing. We really don’t feel that we have the end of the season in the next couple of weeks. It could be several more weeks of flu. It’s partly where we will be at the end of year. The other comment for the aficionados of the data is we usually see the increases in influenza-like illness and hospitalizations a couple of weeks before we see what’s going on with influenza and pneumonia deaths. People may have lengthy hospitalizations before they finally die from flu. So there’s some lag there. I wish there was better news this week, but almost everything we’re looking at is bad news. The one bright spot is that the H3N2 virus’ numbers are coming down and those are the more severe strains we think. So we just have to keep being vigilant. Next question operator.
OPERATOR: Thank you. Our next question comes from Maggie Fox with NBC. You line is open, you may ask your question.
MAGGIE FOX: You mentioned that people should stay home from work. We have been talking to people who have been fired, including a nurse who lost her job for staying home from work. Can you talk about the importance of having sick day policies and sick leave for people? Thanks.
ANNE SCHUCHAT: Thank you for that question. It’s such a difficult dilemma for people. We know that no one wants to lose their jobs for being sick. The employers that have policies that are good for their workers can actually be good for the workplace. We have seen some schools that have dismissed students because too many people are sick to keep the school going. This kind of season is really hard on families, communities and workers as well. Next question.
OPERATOR: The next question comes from Mike Stobbe with the Associated Press. Your line is open. You may ask your question.
MIKE STOBBE: Thank you for taking my call. Dr. Schuchat, you said earlier something about we usually see better protection against B. Is there more information you can give us about what the vaccines, how well it’s doing against B? Also, on vaccine effectiveness, if it turns out when you guys have the vaccine effectiveness numbers that it’s not very good, do you think it’s because the flu virus is mutating while the vaccine is being made in the eggs? If that’s the case, what’s the plan for vaccine production this coming fall? Are we going to make the vaccine the same way and might this happen again?
ANNE SCHUCHAT: Thank you mike. We don’t have our results yet for the vaccine effectiveness against the different types. We hope to get it in the near future. The Canadians who have a similar strain circulating and similar vaccines in use have already reported their preliminary results. They did have a high effectiveness for B. I think it was about 55 percent compared to the very low results they had for H3N2. So, I wouldn’t be surprised if we see something like that. As we have been seeing the B strains increase, it’s one of the reasons we said even though it seems like it’s pretty late in the year because the vaccine takes about two weeks to give you protection, we do think it’s worthwhile for people who didn’t already get a vaccine to consider getting vaccinated. The issue with the low effectiveness against H3N2 that we’ve seen over the years and that was particularly striking in Australia and Canada and that we’ll be looking for in our data has raised a lot of questions. There is a lot we need to understand, whether we have been talking and the scientists at NIG as well have been talking about the egg-adapted changes in viruses grown in eggs to prepare vaccines. Whether there are short-term and longer-term steps that could be taken to reduce the risks that that will happen, it may be that there are vaccine viruses that can be collected that are less likely to have that problem. It may be that there is merit in exploring other approaches to vaccine production. You know, there are cell-based vaccines and recombinant vaccines, but as we’ve been saying we don’t know yet that there is differences in effectiveness in the different types of vaccines. It’s a key question that people want to look at and more studies are expected. I can say that the U.S. government, Department of Health & Human Services is looking at this season’s data very carefully and needing to talk about longer-term approaches to improve flu vaccines. Next question operator.
OPERATOR: Thank you. Our next question comes from Lena Sun with the Washington Post. Your line is open. You may ask your question.
LENA SUN: I’m sorry Dr. Schuchat. I’m having a little hard time hearing you. I wasn’t sure of some of the words you said. In your opening, you said this season is on track to and I think you said, break something records. I wasn’t sure what the in between was. You also said in answering Helen’s question that another sort of bad thing was that you’re seeing increase in ILI and hospitalizations and that normally you see increase in ILI and hospitalizations a couple weeks before pneumonia deaths. I wasn’t sure if what you were saying is this season different in that all those are coming at the same time?
ANNE SCHUCHAT: I’m sorry about my volume. I will try to make sure to speak louder. I believe at the beginning what I meant to say was this season we are on track to break some recent records. In terms of the lag, I wasn’t saying this season is different. What I was trying to say was we have very high influenza-like illness activity. We have very high hospitalizations. Our pneumonia and influenza deaths are not yet very, very high compared to previous years, but unfortunately, more deaths are likely to happen. So that lag I was describing was meant to say over the next few weeks we do expect it would make sense to see lots of pneumonia and influenza deaths. The people who are likely to die may already be in the hospital basically. That was the message I was trying to convey and, again sorry about the volume. Operator, next question.
OPERATOR: Thank you. The next question comes from Brenda Goodman with WEB MD. Your line is open. You may ask your question.
BRENDA GOODMAN: Hi Dr. Schuchat. I just have a question about the B strain starting to peak and whether you have seen such a close overlap before between the A and the B strains. We have heard from some of our readers’ questions about could I get the flu twice in once season if I get difference strains and anecdotally we have heard reports that some people have been diagnosed with A and B strain at the same time. Are you hearing about that? Is that contributing to some of the severity?
ANNE SCHUCHAT: The B strains often, or it’s not uncommon for B strains to increase later in the season. The idea that a person can get infected with A and during the same season get infected with B definitely happens. It’s one of the reasons we say even if you have already had the flu this season it makes sense to get vaccinated because it could protect you against the other strain. In a season that’s so intense like this we may hear of more of those cases such as your readers are reporting where a person got on and then the other. It is possible to get the two at the same time. I have a virologist sitting across the table shaking her head vigorously so we know it is not a lab error. That can happen. Next question operator.
OPERATOR: Thank you. The next question comes from Miranda Suarez with WBUR. Your line is open. You may ask your question.
MIRANDA SUAREZ: Hi, so you talked earlier about the rate of flu in the west. I was wondering if you had specific numbers for New England as a region? If not, where I can find those numbers.
ANNE SCHUCHAT: I think we can get back to you after the call with specifics. I would like to say that our website has what we call FluView, where every week we update numbers. There are state-specific data in there. We can get with you after the call. Somebody can follow up with you. Next question, operator?
OPERATOR: Thank you. Our next question comes from Courtney Norris with PBS Newshour. Your line is now open. You may ask your question.
COURTNEY NORRIS: Thank you so much for taking my call. I was just curious if you talk more about, I believe you said Oregon and Hawaii were reporting less widespread influenza activity. If there is any, you know, reason why or what’s known about why those two are less?
ANNE SCHUCHAT: You know, most years the influenza season starts and ends at different times in different places. The places where it started earlier may be the ones, which are starting to see improvements earlier. One of the unusual features of this year was that we have had several weeks now where so many states have had high activity at the same time. That contributed, we think, to some of the spot shortages in anti-viral drugs. Because often it is the east coast and then the west coast or the Midwest. But we had so many states with high levels of activity all at the same time. I don’t think there is anything special about Oregon. Hawaii, of course, is very special in many ways, but I think with a very different season that a lot of places. But I think that Oregon may just have seen the season come earlier than other parts of the country. Next question.
OPERATOR: Thank you. Our next question comes from Catherine Roberts with Consumer Reports. Your line is open. You may ask your question.
CATHERINE ROBERTS: Thanks for taking my question. Two things. First, can you give us more details about what’s being done to address the spot shortages? How long does the response usually take and is there talk of dipping into the strategic stockpile reserves? Then, two, to what extent are you seeing consumer interest in alternative treatments for flu given shortages in the anti-viral drugs and the severe season generally? Thank you.
ANNE SCHUCHAT: the supply of the anti-viral drugs exceeds the demand that we are having although prescriptions this year are higher than in previous years. There are millions of doses, literally, that have been produced. The efforts have involved staff here being in contact with the producers of both the brand and generic drugs, the distributors who handle the shipments, the pharmacies and large chain stores as well as the pharmacy benefit managers and there are actually a number of insurers. One of the things that was done was ask pharmacies to try to stock larger amounts rather than trying to reorder. Another has been working with some of the companies and the pharmacy benefit managers to address, you know, it may be that in a particular store there is no more generic, but there is branded product. So there’s been efforts to work with the parts of the system who in some cases allow the brand to be used either as a generic in term of the prescription that was written or as a preferred brand which is less costly than usual. So there’s been a lot of cooperation, I would say, in the different parts of the system. How quickly is the adjustment? I would say it varies in different areas. The large chain stores do have quite a bit of the market and are working pretty closely to correct things. So I absolutely want to say I’m sorry for the people who are having trouble finding medicine that they are looking for and the efforts people have had to take to find a place that can fill their prescriptions. But that we are working hard with the system to try to improve it as quickly as possible. The Strategic National Stockpile is not needed. The commercial supply is there. The Strategic National Stockpile is not used to displace the commercial supply. Next question.
OPERATOR: Thank you. Our next question comes from Sarah Toy with the Wall Street Journal. Your line is open. You may ask your question.
SARAH TOY: Thanks for taking my question. We were told of a case where a woman delayed filling her anti-viral script due to cost. She was eventually hospitalized and she’s passed away from flu related complication. Earlier you mentioned it could make the difference between a hospitalization and mild illness and from what we’ve heard it is the most effective early on when a person starts showing symptoms. Can you tell me a little bit about the best time to take the meds and at what point does it not make a difference anymore.
ANNE SCHUCHAT: I really can’t say when it doesn’t make a difference anymore. But the studies suggest that taking medicine within 48 hours of beginning symptoms will give those drugs the best chance of working. In some of our studies, it may be four to seven days after symptoms began, there was some benefit in terms of reducing complications. But the best data comes from randomized control trials that looked really at the duration of symptoms and found that if you could start the medicine within 48 hours there was a significant shortening of how long the illness lasted. Most the data about reduced complications like hospitalizations or intensive care unit admissions comes from observational data. There are some qualifications that need to be made about the timing there. I would say that we do want clinicians to know that if the person look like they have flu, don’t wait on a test result of if you get a negative test result and the person – it’s a time of year now where most people with respiratory illness that looks like flu do have flu. You should treat if it’s a person with severe presentation or a person with underlying risk conditions. Next question, operator.
OPERATOR: Thank you. Our final question comes from Michelle Cortez with Bloomberg News. Your line is open. You may ask your question.
MICHELLE CORTEZ: Thanks so much. You said we are seeing more ILI than going all the way back to 200.3 When we look at the FluView you guys put out today, just a couple of minutes ago, it looks like we are already king of exceeding the swine flu levels that we saw. You said we are above 2003. I know that your data doesn’t go back. You know, with the method you’re using now. But when you look, I’m sure you have expertise there. How far back do you have to go to beyond 2003 to see a season like this? And then the follow up to that is the swine flu and 2003 those were both new viruses or new strains. We’re not seeing that. My understanding is this strain is similar to what we saw two years ago. Why is it that this strain is seemingly hitting so much harder than other years? Thanks.
ANNE SCHUCHAT: Yeah, thanks. One think I want to say about the long-term comparisons, there is a lot of things that are different from 2003 to now. You know, one thing is that a majority of children actually get vaccinated against flu now. We weren’t routinely vaccinating children. You may remember 2003-04 was an early season and really severe in children. Really after that season we started to make deaths in children from flu reportable because the problem was so great. I think in terms of all the records and so forth because we do have high vaccination rates in children, because the H1N1 and B strains are often more of a problem in children than the H3N2 focusing on the older populations, I think we’ll have to see in the end how well the vaccine is working against children’s influenza and whether we are breaking records in kids or not this year. Hopefully the full toll on children won’t be as bad as in those earlier years. In term of the question of, you know, 2009-10 was a pandemic strain, a novel re-assortment from a couple different species. The birds, pigs and people. 2004-04 was a new H3N2 strain. We are still characterizing this year’s virus. This year’s virus isn’t’ new in terms of anti-genic drift the wat the 2003-04 strain was, but our virologists and others around the country are studying the virus to see whether there are other explanations for the more severe disease we are seeing. We are also still looking at the vaccine effectiveness and trying t6o understand whether there are host difference, things like prior immunization that may contribute to something. I think we have a lot to learn still about influenza including about this particular season. It’s a wakeup call about how severe influenza can be and why we can never let down our guards against this virus because it is a very, very – the virus is always changing. We need to stay faster than it in our changes. Thank you. I believe that’s the last question. I really appreciate the interest and our website will have the graph that I mentioned, as well as, the whole FluView.
KATHY HARBEN: Thank you Dr. Schuchat and Dr. Fry for joining us today. Also, thank you to the reporters who joined. For follow-up questions, you can call us at 404-639-3286 or you can email us at media@cdc.gov. Thanks for joining us. This concludes our call.