Newborn Screening Laboratory Bulletin
V. Next Generation Newborn Screening
Genomics
CDC strives to stay in the forefront of technological and scientific advancement in order to continually improve its newborn screening-related activities. Recently CDC expanded laboratory capabilities for its Newborn Screening Quality Assurance Program (NSQAP) by including a group of its scientists (molecular biologists) who have extensive expertise in understanding how genetics and changes in DNA are associated with important public health issues such as diabetes, kidney disease, birth defects, and asthma. The expertise of these scientists helps newborn screening research because DNA-based testing—
- can be used to confirm the results when a newborn tests positive for a disorder.
- can be done, to confirm a positive result, on the same blood spot used for the initial test (allowing all screening results to be reported at the same time without worrying families about testing and retesting).
- can be used to add new disorders to panels for newborn screening.
The newly expanded laboratory has focused on cystic fibrosis, a particularly complex disease with more than 1500 known mutations. The collaboration of CDC scientists and the Cystic Fibrosis Foundation (which was instrumental in providing donor case samples) resulted in the development of proficiency testing materials that are now being used by state laboratories to assure high-quality DNA-based confirmatory testing of positive screening results.
As genetic tests become more available, many newborn screening laboratories are considering the use of DNA-based testing to confirm positive results for disorders such as galactosemia, congenital adrenal hyperplasia, severe combined immune deficiency, and lysosomal storage disorders. As states move testing in this direction, it will be critical for them to have access to technical expertise as well as the kind of blood spot materials necessary for quality assurance and proficiency testing. As newborn screening laboratory testing evolves, CDC will continue to provide the technical expertise and the materials required as more disorders are added to the states’ screening panels. NSQAP—the only comprehensive quality assurance program for newborn screening—has the experience, the infrastructure, and the solid reputation in the newborn screening community to respond to the changing technology and rapid expansion of this field.
Emerging Technologies
Although DNA-based testing is a developing part of newborn screening, biochemical testing is widely used in state newborn screening programs. CDC can use its expertise in both genetics and biochemistry to collaborate with states, research partners, and stakeholders to provide comprehensive data for new methods, new applications, and new blood spot materials for use in newborn screening. In particular, CDC is interested in collaborative research that—
- helps states maintain high standards of proficiency as they expand their newborn screening tests and programs.
- seeks to understand how genetic and biochemical differences that occur within the diverse population of the United States will help improve newborn screening.*
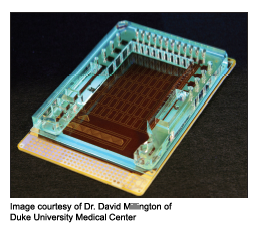
- explores innovative testing technologies (e.g., nanotechnology and “a lab on a chip”).†
Ultimately, the knowledge gained from future research and collaborations will lead to improvements and expansion of newborn screening activities that save lives and improve the health and wellbeing of all babies.
*Understanding the genetic and biochemical differences will not only help improve newborn screening but also allow for research that provides a better understanding of the disease process. CDC scientists will collaborate on population studies with research partners at the federal and state level.
†DNA microarray or digital microfluidics (e.g., chip technology or “lab on a chip”) can be used for detecting disease markers. This technology is appealing to the field of newborn screening because, with additional research and development, it holds the potential to screen simultaneously for hundreds of disorders, improve testing specificity, improve prediction of disease severity (which can guide treatment decisions), enable the inclusion of infectious agents, reduce the amount of blood needed for testing, and produce faster results(10).
Next Section: VI. References