Research Rounds – Volume 2, Issue 5, November 2016
NIOSH Research Rounds is a monthly bulletin of selected research at the National Institute for Occupational Safety and Health.
Volume 2, Number 5 (November 2016)
Tabs Aid Doffing of Filtering Facepiece Respirators
In healthcare, workers wear filtering facepiece respirators as protection against inhaling infectious particles such as viruses and bacteria, but safe use does not end with putting on, or donning, the respirator. Equally important is the proper removal, or doffing, technique, which protects workers from exposure to infectious materials that may have settled on the respirator itself. Once on the hands, the viruses or bacteria pose a risk of infecting the worker if they are re-released in the air and inhaled or if the worker touches any of his or her mucous membranes.
Recommended by the Centers for Disease Control and Prevention (CDC), the proper doffing technique involves pulling the respirator straps at the back of the head. The problem, according to some reports, is that healthcare workers may not know or remember to follow these recommendations due to difficulty with locating and pulling these straps.
Addressing this issue, researchers at the National Institute for Occupational Safety and Health (NIOSH) designed and tested an intervention for NIOSH-certified N95 filtering facepiece respirators, they report in the Journal of Occupational and Environmental Hygiene. The researchers attached four red foam tabs to the straps on the respirators to act as an easy-to-find handle to grasp during removal. They then used a harmless, fluorescent substance as a tracer to track possible “contamination” from the straps to the hands and heads of 20 volunteer study participants, including 15 women and 5 men between 18 and 60 years old. Comparing the tabbed straps to the regular straps, they found that the doffing technique was comparable between both types. However, the tabbed straps resulted in significantly less spread of the fluorescent tracer substance. In addition, the modified models were easier to use than the non-tabbed models. Seven of the 20 participants found the tabbed straps easier to remove, compared with 2 of the 20 who found that doffing was easier with the non-tabbed models. Neither type of strap caused discomfort among the participants.
These findings suggest that tabs can promote ease of use and protection from contamination for workers who properly remove personal protective equipment, such as a respirator. As a next step, the investigators recommend repeating this study with a larger sample of the general population.
To provide information about the proper donning and doffing procedure for personal protective equipment, the CDC created the downloadable posters below, which also are available on the CDC website.
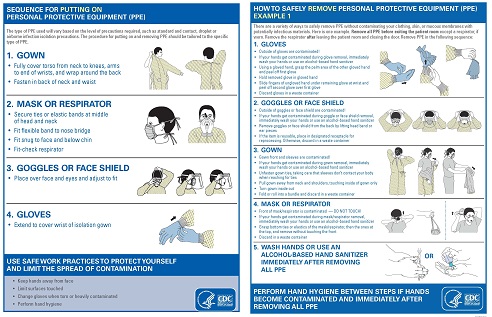
CDC-recommended donning (left) and doffing (right) procedures. Image from CDC.
More information is available:
- Assessing the Efficacy of Tabs on Filtering Facepiece Respirator Straps to Increase Proper Doffing Techniques while Reducing Contact Transmission of Pathogens
- Sequence for Putting on (Donning) and Removing (Doffing) Personal Protective Equipment
- The National Personal Protective Technology Laboratory
- John Howard, M.D., Director
- Fred Blosser, Editor in Chief
- Anne Blank, Story Editor
- Tanya Headley, Contributing Editor
- Cathy Rotunda, Copy Editor
- Glenn Doyle, Technical Lead
- Tonya White, Technical Support
Healthcare Workers Perceive “Cooler” Safety Climate

Healthcare workers reported less positive perceptions of their workplace safety climate than both hospital managers and unit managers. Image from Thinkstock
As winter approaches and cooler temperatures hit most of the nation, workers unpack coats and boots, and workplaces adjust thermostats. However, one climate that should stay the same year-round, no matter where a workplace is located geographically, is the safety climate. Safety climate—defined as the perception among workers about the value of safety—correlates to improved health and safety in the workplace.
Depending on whom you ask, however, this perception may differ.
Although important in all industries, a strong safety climate is especially critical in high-risk occupations such as healthcare. The rate of reportable nonfatal injury and illness in healthcare is almost double that of all private sector occupations, according to 2014 data from the Bureau of Labor statistics. One of the main causes of this high rate is respiratory illness stemming from exposure to airborne bacteria and viruses, and hazardous chemicals in various cleaning and sterilization products.
To compare perceptions about the safety climate for respiratory protection in healthcare, the National Institute for Occupational Safety and Health (NIOSH), in collaboration with university researchers and state health departments, analyzed survey data collected in 2011 and 2012 for a national study. The Respirator Use Evaluation in Acute Care Hospitals study evaluated how acute care hospitals implemented respiratory protection program requirements from the Occupational Safety and Health Administration and infection control guidance from the Centers for Disease Control and Prevention. Survey respondents included 215 hospital managers, 245 unit managers, and 1,105 healthcare workers in 98 acute care hospitals in six states, including California, Illinois, Michigan, Minnesota, New York, and North Carolina. Each survey included 10 questions designed to measure five key components of safety climate:
- Managerial commitment to safety
- Management feedback on safety procedures
- Coworkers’ safety norms
- Worker involvement
- Worker safety training
The investigators found that perceptions varied significantly among the three groups. Overall, healthcare workers reported less positive perceptions of their workplace safety climate than both hospital managers and unit managers. In comparison, unit managers viewed management’s supervision of healthcare workers’ respiratory protection practices more favorably than both hospital managers and healthcare workers.
According to the investigators, the findings indicate the need for frontline healthcare workers’ inclusion to better support effective respiratory protection programs and practices. Hospital management should ensure that they create formal opportunities for frontline healthcare workers to provide feedback to management about their individual respiratory protection programs, training, and ways to improve safe respiratory protection practices at the point of care, according to the study published in the journal Workplace Health & Safety. To understand why perceptions about safety climate differ, further research is necessary.
More information is available:
- Differences in Hospital Managers’, Unit Managers’, and Health Care Workers’ Perceptions of the Safety Climate for Respiratory Protection
- The National Personal Protective Technology Laboratory
Trends in Mining-related Musculoskeletal Disorders Identified
Lung diseases are some of the most serious and recognized risks linked to mining, but coal miners also face other work-related hazards. Of particular concern are work-related disorders affecting the muscles and bones, or musculoskeletal disorders. Recent studies have looked at the causes and prevention of these disorders in various industries, but surveillance data characterizing musculoskeletal injuries by type, prevalence, and trends specifically in mining was somewhat outdated.
Accordingly, investigators at the National Institute for Occupational Safety and Health (NIOSH) and university partners analyzed the most recent data from the Mining Safety and Health Administration on mining-related musculoskeletal disorders. Examining data from 2009 to 2013, they found that musculoskeletal disorders occurred more frequently among both novice and expert miners, according to their paper in The Journal of Safety, Health and Environmental Research. Specifically, musculoskeletal disorders occurred most often among miners with fewer than 5 years and more than 20 years of experience. In terms of absenteeism, the musculoskeletal disorders associated with the most missed workdays were shoulder and knee injuries, which both occurred more often among older miners. In other findings, the study found that some activities are riskier than others for incurring musculoskeletal disorders. In particular, four activities were associated with a greater risk:
- Overexerting
- Falling or being struck by an object while performing materials handling, maintenance, and repair tasks
- Getting on or off equipment or machines
- Walking or running
Injury prevention in public health relies upon identifying trends. By identifying mining-related trends in musculoskeletal disorders, these results provide a renewed focus for ongoing prevention research.
More information is available:
- Identification of Work-Related Musculoskeletal Disorders in Mining
- NIOSH Mining
- Ergonomics and Musculoskeletal Disorders
NIOSH Intervention Model Reaches Small Businesses
An intervention model developed by two investigators at the National Institute for Occupational Safety and Health (NIOSH) brings crucial information about work-related safety and health to small businesses, the same investigators reported in the journal Safety Science. Drawn from previous research in Europe and New Zealand, the model depends upon intermediary groups—such as goods and services suppliers, membership organizations, educational organizations, and government agencies—to relay information about health and safety from large organizations, such as NIOSH, to small businesses.
Reaching small businesses is critical, since most businesses in the United States employ fewer than 20 workers, which is the typical definition of a small business. In fact, 79% of all U.S. companies have fewer than 10 employees. Unfortunately, with fewer employees comes fewer resources to devote to health and safety interventions, and several studies show that small businesses have proportionately more work-related injuries, illnesses, and deaths than businesses with 20 or more employees.
To test their model’s effectiveness in serving small businesses, the investigators applied it to four case studies:
- Trenching safety training for construction
- Basic compliance and hazard recognition for general industry
- Expanded safety and health training for restaurants
- Fall prevention and respirator training for boat repair contractors
What the Case Studies Showed
The model succeeded in several areas, the investigators concluded. It facilitated NIOSH investigators’ participation with the intermediary groups’ planning activities and showed that the needs of the small businesses aligned with the intermediary groups’ offerings. Additionally, the model enabled strong leadership among the intermediary groups, while encouraging ongoing monitoring by NIOSH investigators. At the same time, several challenges emerged in the evaluation. These challenges included inadequate resources among intermediary groups and insufficient opportunity for in-person meetings between these groups and the NIOSH investigators. Another challenge was balancing the number of interactions between NIOSH investigators, the intermediary groups, and the small businesses.
Even so, the case studies show that the model’s reliance on intermediary groups is one way for large organizations to reach more small businesses than they could on their own, according to the investigators. Now, they are applying the model in ongoing studies, including a project exploring how to bring Total Worker Health® practices to small businesses through relevant intermediaries such as local health departments, health service providers to businesses, and safety consultants.