2008 Salmonella Outbreak Linked to Raw Produce
NOTICE: This outbreak is over. The information on this page has been archived for historical purposes only and will not be updated.
Posted August 28, 2008
Outbreak Summary
CDC has been working with state, local, and tribal health departments, the Indian Health Service, and the Food and Drug Administration (FDA) to investigate a large, multi-state outbreak of Salmonella Saintpaul. The outbreak appears to be over. However, CDC and state health departments are continuing to conduct surveillance for cases of infection with the outbreak strain. Public health officials also continue to analyze data gathered during the investigations.
On May 22, 2008 the New Mexico Department of Health notified CDC of four people ill with the outbreak strain of Salmonella Saintpaul and 15 other persons with Salmonella infection whose isolates had not yet been characterized. In the following weeks, cases of illness with the outbreak strain continued to be reported and the outbreak expanded to include 43 states, the District of Columbia and Canada.
CDC and its public health partners on the federal, state, local, and tribal levels searched for the source of the outbreak and took steps to stop transmission of the infection. The investigators depended on the cooperation of hundreds of ill and well persons across the country who answered questions about what foods they had recently consumed. This allowed investigators to link illness with particular food items. In addition, public health officials in several states, with the assistance of CDC, investigated clusters of ill persons who had eaten at the same restaurants. FDA and state investigators traced the origin of some produce items back through the distribution chain and collected samples to test for the presence of the outbreak strain.
The investigation showed that jalapeño peppers were a major source of contamination and that serrano peppers also were a source. In addition, tomatoes were possibly a source, particularly early in the outbreak. Jalapeño peppers were traced back to distributors in the United States that received produce grown and packed in Mexico. The outbreak strain was isolated from samples of jalapeño peppers collected in a US warehouse and a patient’s home and from samples of serrano peppers and water collected on a farm in Mexico.
Since April, 1442 persons infected with Salmonella Saintpaul with the same genetic fingerprint have been identified in 43 states, the District of Columbia, and Canada. These were identified because clinical laboratories in all states send Salmonella strains from ill persons to their State public health laboratory for characterization. The number of ill persons identified in each state is as follows: Alabama (8 persons), Arkansas (21), Arizona (59), California (16), Colorado (17), Connecticut (5), Florida (4), Georgia (42), Idaho (6), Illinois (120), Indiana (21), Iowa (2), Kansas (21), Kentucky (2), Louisiana (3), Maine (1), Maryland (39), Massachusetts (31), Michigan (28), Minnesota (31), Mississippi (2), Missouri (20), Montana (1), New Hampshire (6), Nevada (14), New Jersey (16), New Mexico (115), New York (41), North Carolina (28), Ohio (10), Oklahoma (38), Oregon (11), Pennsylvania (15), Rhode Island (3), South Carolina (2), Tennessee (10), Texas (559), Utah (3), Virginia (31), Vermont (2), Washington (18), West Virginia (1), Wisconsin (13), and the District of Columbia (1). Five ill persons are reported from Canada. Four appear to have been infected while traveling in the United States; the travel status of the fifth ill person is unknown.
Among the 1414 persons with information available, illnesses began between April 16 and August 11, 2008 with most becoming ill during May or June; 119 became ill on July 1 or later. These numbers include those with estimated onset dates as well as those with reported onset dates. The latest reported onset date is August 11. The latest estimated onset date is August 7.
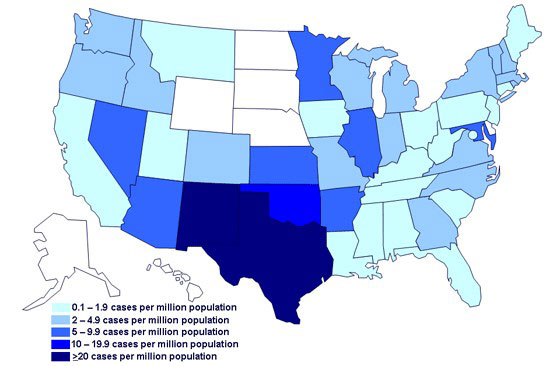
Complete demographic information was available for 565 ill people. Of these, 52% were male; 79% were white, 8% were American Indian/Alaska Native, 3% were black, 2% were Asian/Pacific Islander, and 7% reported other or multiple races. Hispanic ethnicity was reported for 22%. Patients ranged in age from <1 to 99 years with a median age of 33 years. The rate of illness was highest among persons 20 to 29 years old. Cases were distributed among 43 states, the District of Columbia, and Canada, with particularly high incidence rates in New Mexico and Texas. At least 286 persons were hospitalized, and the infection might have contributed to two deaths.
The outbreak can be visually described with a chart showing the number of persons who became ill each day. This chart is called an epidemic curve or epi curve. Please see Interpretation of Epidemic Curves during an Active Outbreak. It shows that the number of persons who became ill peaked during May and decreased in June. The average number of persons who became ill in recent weeks continues to decrease, indicating that the outbreak is ending. See the Salmonella Outbreak Investigations: Timeline for Reporting Cases.
Only 18 persons infected with this strain of Salmonella Saintpaul were identified in the country during April through August of 2007. The previous rarity of this strain and the distribution of illnesses in all U.S. regions suggest that the implicated food is distributed throughout much of the country. Because many persons with Salmonella illness do not have a stool specimen tested, it is likely that many more illnesses have occurred than those reported. Some of these unreported illnesses may be in states that are not on today’s map.
For More Information:
- MMWR article Multistate Outbreak of Salmonella Serotype Saintpaul Infections Associated with Multiple Raw Produce Items
- New England Journal of Medicine article 2008 Outbreak of Salmonella Saintpaul Infections Associated with Raw Produce
Final Epi Curve
Persons infected with the outbreak strain of Salmonella Saintpaul, by date of illness onset*
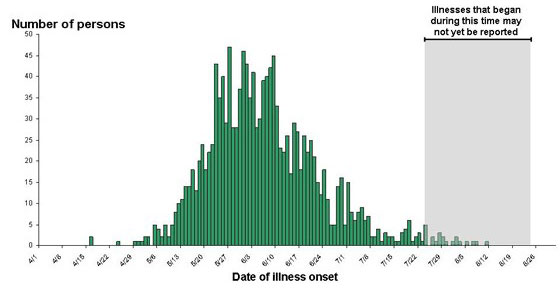
*n=1442 for whom information was reported/estimated as of August 25, 2008
Final Case Count Maps
Persons infected with the outbreak strain of Salmonella Saintpaul, by state of residence, as of August 25, 2008 (n=1442)
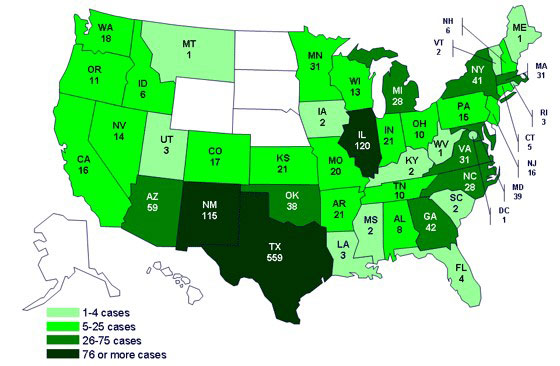
The number of ill persons identified in each state is as follows: Alabama (8 persons), Arkansas (21), Arizona (59), California (16), Colorado (17), Connecticut (5), Florida (4), Georgia (42), Idaho (6), Illinois (120), Indiana (21), Iowa (2), Kansas (21), Kentucky (2), Louisiana (3), Maine (1), Maryland (39), Massachusetts (31), Michigan (28), Minnesota (31), Mississippi (2), Missouri (20), Montana (1), New Hampshire (6), Nevada (14), New Jersey (16), New Mexico (115), New York (41), North Carolina (28), Ohio (10), Oklahoma (38), Oregon (11), Pennsylvania (15), Rhode Island (3), South Carolina (2), Tennessee (10), Texas (559), Utah (3), Virginia (31), Vermont (2), Washington (18), West Virginia (1), Wisconsin (13), and the District of Columbia (1).
Incidence of cases of infection with the outbreak strain of Salmonella Saintpaul, by state of residence, as of August 25, 2008
Clinical Features
Most persons infected with Salmonella develop diarrhea, fever, and abdominal cramps 12-72 hours after infection. Infection is usually diagnosed by culture of a stool sample. The illness usually lasts 4-7 days. Although most people recover without treatment, severe infections may occur. Infants, elderly persons, and those with impaired immune systems are more likely than others to develop severe illness. When severe infection occurs, Salmonella may spread from the intestines to the bloodstream and then to other body sites, and can cause death. In these severe cases, antibiotic treatment may be necessary.
Advice to Consumers
The U.S. Food and Drug Administration (FDA) has lifted its advice to consumers to avoid eating jalapeño and serrano peppers grown, harvested or packed in Mexico.
The FDA has taken this action consistent with the CDC announcement that the Salmonella Saintpaul outbreak appears to be over, and that jalapeño peppers and serrano peppers grown in Mexico and associated with the Salmonella Saintpaul outbreak are no longer in circulation in the U.S. market.
In July, the FDA lifted its advice to avoid raw red round, red Roma, and red plum tomatoes.
The FDA continues to work with CDC, Mexican authorities, state regulatory agencies and food industry groups to ensure that Americans continue to enjoy one of the safest food supplies in the world.
Consumers are reminded that vegetables are an important part of a healthy diet and that cooking vegetables kills bacteria, including Salmonella.
Questions and Answers
What is salmonellosis? What are the symptoms?
Salmonellosis is an infection caused by bacteria called Salmonella. Most people infected with Salmonella develop fever, diarrhea, and abdominal cramps 12 – 72 hours after exposure. Although illness usually lasts 4 – 7 days and most people recover without treatment, severe illness may occur that requires medical attention and hospitalization. In these patients, the Salmonella infection can spread from the intestines to the bloodstream and then to other body sites. In this situation, the infection can cause death unless the patient is treated promptly with antibiotics. Infants, elderly people, and people with impaired immune systems are more likely than other people to become severely ill.
How do people get infected with Salmonella?
Salmonella bacteria live in the intestinal tracts of many animals, including food animals such as cattle and poultry, wild animals, and pets. Salmonella usually are transmitted to humans by eating food contaminated with animal feces. Contaminated foods usually look and smell normal. Contaminated foods are often of animal origin, such as poultry, eggs, pork, and raw milk. However, contaminated fruits and vegetables also cause many illnesses. Thorough cooking kills Salmonella.
The feces of some pets, especially reptiles, can contain Salmonella without causing illness in the animal. Birds commonly carry Salmonella, and outbreaks of illness among young children given baby chicks at Easter have prompted health authorities to advise against this practice. People should always wash hands after being in contact with any animal or its environment. Adults should assure that children practice proper handwashing techniques. More information on proper handwashing.
Food handlers and others can contaminate food by not washing hands with soap after handling raw poultry, eggs, or meat, or after using the bathroom.
Does Salmonella make foods taste or look different?
Most products contaminated with Salmonella do not taste or look any different than usual.
How is Salmonella infection diagnosed?
Salmonella infection is usually diagnosed by culture of a stool sample. In severe illness, it can sometimes be detected in other parts of the body such as blood.
How can Salmonella infections be treated?
Salmonella infections usually resolve in 4 – 7 days and usually do not require treatment other than oral fluids. Persons with severe diarrhea may require rehydration with intravenous fluids. Antibiotics, such as ampicillin, trimethoprim-sulfamethoxazole, or ciprofloxacin, are not usually necessary unless the infection spreads from the intestines.
Are there long term consequences to a Salmonella infection?
Persons with diarrhea usually recover completely, although it may be several months before their bowel habits are entirely normal. A small number of persons with Salmonella develop pain in their joints, irritation of the eyes, and painful urination. This is called Reiter’s syndrome. It can last for months or years, and can lead to chronic arthritis which is difficult to treat. Antibiotic treatment does not make a difference in whether or not the person develops arthritis.
How common is salmonellosis?
In 2004, CDC estimated that there are about 1.4 million illnesses, 15,000 hospitalizations, and 400 deaths from Salmonella infection in the United States every year. Approximately 40,000 of those infections are confirmed each year by isolation of the Salmonella strain. Salmonellosis is more common in summer than in winter.
Children are the more likely than adults to get salmonellosis. The rate of diagnosed infections in children less than five years old is about five times higher than the rate in all other persons. Young children, the elderly, and the immunocompromised are the most likely to have severe infections.
How can tomatoes become contaminated with Salmonella?
Salmonella in the environment can contaminate tomatoes. Salmonella can be found in the feces of many animals (e.g., food animals, reptiles, amphibians, birds) and in some habitats, such as ponds and drainage ditches. Although the exact mechanism by which tomatoes become contaminated is not known, experimental evidence suggests certain possibilities. In experimental studies, the insides of whole tomatoes can be contaminated in at least two ways: (1) if tomatoes are immersed in water that is colder than the tomato, water can enter through the stem scar; if the water is contaminated, Salmonella can be carried in; (2) if contaminated water touches the stem or flower of a tomato plant, the growing tomato can be contaminated. Contamination on the tomato surface also can be transferred to the inside when it is cut. Food handlers infected with Salmonella who have not washed their hands may also contaminate tomatoes during preparation. If a cut tomato that is contaminated with Salmonella is kept out of the refrigerator, the bacteria can multiply to much higher numbers.
What is the CDC’s current advice about eating tomatoes?
At this time, consumers should avoid eating or handling raw red plum, red Roma, and round red tomatoes unless they are from the sources listed. If consumers have tomatoes in their homes and are unsure of where they were grown or harvested, they are encouraged to contact the store where they bought the tomatoes. Consumers may continue to buy cherry tomatoes, grape tomatoes, tomatoes with the vine still attached, and tomatoes grown at home — all of which do not appear to be involved in the outbreak.
Consumers everywhere are advised to:
- Refrigerate within 2 hours or discard cut, peeled, or cooked tomatoes, or products made from tomatoes, such as salsa.
- Avoid purchasing bruised or damaged tomatoes and discard any that appear spoiled.
- Thoroughly wash all tomatoes under running water. Do not wash tomatoes in a tub or sink filled with water.
- Keep tomatoes that will be consumed raw separate from raw meats, raw seafood, and raw produce items.
- Wash cutting boards, dishes, utensils, and counter tops with hot water and soap when switching between types of food products.
Is it OK for consumers to eat tomatoes that might be associated with this outbreak if they cook them?
FDA is recommending that consumers not eat any tomatoes that could be associated with this outbreak, either raw or cooked.
Salmonella is easily killed by high temperatures. However, when a food is contaminated with Salmonella, people often do not cook it to a high enough temperature or long enough to kill the bacteria. (For example, raw chicken is commonly contaminated with Salmonella. We advise people to use a cooking thermometer to assure that they cook chicken well enough to kill the Salmonella bacteria.)
Are tomatoes from farmers’ markets included in this outbreak?
Some farmers’ markets get their tomatoes from sources other than local farms. These other sources may include the same ones that provided the tomatoes implicated in the Salmonella outbreak. Consumers should ask retailers at farmers’ markets about the sources of their tomatoes.
During this outbreak, is it safer to eat locally grown tomatoes?
Consumers should confirm with their retailers that the source of “locally grown” tomatoes is one of the sources listed on the FDA list.