2011 Salmonella Outbreak Linked to Ground Turkey
NOTICE: This outbreak is over. The information on this page has been archived for historical purposes only and will not be updated.
Posted November 10, 2011
Outbreak Summary
CDC collaborated with public health officials in many states and the U.S. Department of Agriculture’s Food Safety and Inspection Service (USDA-FSIS) to investigate a multistate outbreak of Salmonella Heidelberg infections that was caused by eating ground turkey. Public health investigators used DNA “fingerprints” of Salmonella bacteria to identify ill persons who were part of this outbreak. The Salmonella bacteria were obtained from diagnostic testing; pulsed-field gel electrophoresis (PFGE) was used to determine DNA fingerprint patterns. Investigators used data from PulseNet, the national subtyping network made up of state and local public health laboratories and federal food regulatory laboratories that performs molecular surveillance of foodborne infections. The outbreak strain of Salmonella Heidelberg was resistant to several commonly prescribed antibiotics. This antibiotic resistance may have been associated with an increase in the risk of hospitalization or possible treatment failure in infected individuals.
A total of 136 persons infected with the outbreak strain of Salmonella Heidelberg were reported from 34 states with illness onset dates between February 27 and September 13, 2011. The number of ill persons identified in each state was as follows: Alabama (1), Arkansas (1), Arizona (3), California (7), Colorado (4), Connecticut (1), Georgia (2), Illinois (16), Indiana (2), Iowa (2), Kansas (3), Kentucky (2), Louisiana (1), Massachusetts (4), Maryland (1), Michigan (12), Minnesota (2), Mississippi (2), Missouri (7), Nebraska (2), Nevada (1), New Jersey (1), New York (3), North Carolina (4), Ohio (12), Oklahoma (2), Oregon (1), Pennsylvania (8), South Dakota (3), Tennessee (2), Texas (18), Utah (1), Vermont (1), and Wisconsin (4).
Among persons for whom information was available, illnesses began on or after February 27, 2011. Ill persons ranged in age from less than 1 year to 90 years old, with a median age of 23 years old. Fifty-five percent were male. Among the 94 ill persons with available information, 37 (39%) were hospitalized. One death was reported.
The outbreak can be visually described with a chart showing the number of people who became ill each day. This chart is called an epi curve. For more details, please see the Timeline for Reporting Cases of Salmonella Infection for more details.
Investigation of the Outbreak
Collaborative investigative efforts of state, local, and federal public health and regulatory agencies indicated that ground turkey was the likely source of this outbreak. Among the 94 ill persons with available information, 51 (54%) reported consuming ground turkey. This proportion was significantly higher than results from a survey of healthy persons in which 11% of persons interviewed reported consuming ground turkey in the 7 days before they were interviewed. Product information (such as date and location of purchase of ground turkey) was collected from ill persons and was used by local, state, and federal public health, agriculture, and regulatory agencies to further the investigation.
Cultures of five ground turkey samples purchased from five retail locations between March 7 and June 27, 2011, yielded Salmonella Heidelberg with the outbreak strain. PFGE patterns from these Salmonella bacteria were added to the PulseNet database between April 11 and July 12, approximately a month after each sample was collected. Preliminary information indicated that all of these products originated from a common food-production establishment (Cargill Meat Solutions Corporation in Springdale, Arkansas). These products were obtained as part of routine sampling in the National Antimicrobial Resistance Monitoring System (NARMS) and were not linked to illnesses.
This was a multidrug resistant strain of Salmonella Heidelberg. As of September 12, 2011, investigators collected antibiotic resistance information on isolates from 12 samples of ground turkey collected at retail and from 23 ill persons infected with the outbreak strain of Salmonella Heidelberg. The isolates from the ground turkey samples were resistant to antibiotics including ampicillin, streptomycin, tetracycline, and gentamicin. The sensitivity testing results indicated that isolates from humans were also resistant to ampicillin and tetracycline, and some were resistant to streptomycin and gentamicin. All human isolates were sensitive to several common antibiotics used in clinical practice such as ciprofloxacin, ceftriaxone, and trimethoprim-sulfamethoxazole. Antimicrobial resistance may increase the risk of hospitalization or possible treatment failure in infected individuals.
A sample of leftover unlabeled frozen ground turkey was collected by public health officials from the home of an ill person infected with the outbreak strain of Salmonella Heidelberg in Ohio. Culture of the ground turkey sample yielded the outbreak strain on July 29, 2011. In addition to the outbreak strain, with the “initial” PGFE pattern, a Salmonella Heidelberg with a second closely related PFGE pattern was identified in the contaminated leftover product. Since February 27, 2011, a total of 27 ill persons have been reported to PulseNet with this closely related PGFE pattern. Among the 13 such patients who have been interviewed, 12 (92%) reported consumption of ground turkey in the week before their illness began. The closely related PGFE pattern was also found in a retail sample of ground turkey taken as part of NARMS surveillance. This retail sample originated from Cargill Meat Solutions Corporation establishment in Springdale, Arkansas. Based on these findings, the 27 ill persons with this second closely related PFGE pattern of Salmonella Heidelberg were included in the total count of outbreak cases.
On July 29, 2011, USDA-FSIS released a public health alert for frozen or fresh ground turkey products. This alert reminded consumers of the critical importance of following package cooking instructions for frozen or fresh ground turkey products and general food safety guidelines when handling and preparing any raw meat or poultry. The alert advised that, while cooking instructions may give a specific number of minutes of cooking for each side of the patty in order to attain 165°F internal temperature, consumers should be aware that actual time may vary depending on the cooking method (broiling, frying, or grilling) and the temperature of the product (chilled versus frozen). Therefore, it is important that the final temperature of 165 °F be reached for safety. The alert recommends that consumers not rely on the cooking time for each side of the patty, but use a food thermometer. For more information on this public health alert, please see FSIS Issues Public Health Alert for Frozen, Fresh Ground Turkey Products.
Recall Information
On August 3, 2011, Cargill Meat Solutions Corporation, a Springdale, Arkansas, establishment, recalled approximately 36 million pounds of ground turkey products that may have been contaminated with a multidrug resistant strain of Salmonella Heidelberg. The products subject to recall were all comprised of ground turkey meat and had the establishment number “P-963” inside the USDA mark of inspection.
On September 11, 2011, Cargill Meat Solutions Corporation recalled another 185,000 pounds of ground turkey products after product samples at the plant tested positive for the outbreak strain of Salmonella Heidelberg based on sample results from an intensive in-plant investigation performed by FSIS. On September 27, 2011 FSIS reported that one positive sample was confirmed to have the outbreak strain and the isolate was multidrug resistant.
Clinical Features/Signs and Symptoms
Most persons infected with Salmonella bacteria develop diarrhea, fever, and abdominal cramps 12 to 72 hours after infection. The illness usually lasts 4 to 7 days, and most persons recover without treatment. However, in some persons, the diarrhea may be so severe that the patient needs to be hospitalized. Salmonella infection may spread from the intestines to the bloodstream and then to other body sites and can cause death unless the person is treated promptly with antibiotics. Older adults, infants, and those with impaired immune systems are more likely to have a severe illness from Salmonella infection.
Advice to Consumers, Retailers, and Others
This particular outbreak appears to be over. However, Salmonella is still an important cause of human illness in the United States. More information about Salmonella, and steps people can take to reduce their risk of infection, can be found on the CDC Salmonella Web Page and the CDC Vital Signs Web Page.
While the shelf-life of the recalled ground turkey products has been exceeded, consumers might still have recalled products in their homes if the ground turkey was frozen.
- Consumers should check their homes for recalled ground turkey products and not eat them; restaurant and food service operators should not serve it. Consumers with questions about recalled ground turkey products may contact Cargill’s consumer relations toll free telephone number (1-888-812-1646).
- Wash hands, kitchen work surfaces, and utensils with soap and water immediately after they have been in contact with raw meat or poultry including frozen and fresh ground turkey. Then, disinfect the food contact surfaces using a freshly prepared solution of 1 tablespoon unscented liquid chlorine bleach to 1 gallon of water.
- Cook poultry thoroughly. Ground turkey and ground turkey dishes should always be cooked to 165 °F internal temperature as measured with a food thermometer; leftovers also should be reheated to 165 °F. The color of cooked poultry is not always a sure sign of its safety. Only by using a food thermometer can one accurately determine that poultry has reached a safe minimum internal temperature of 165 °F throughout the product. Turkey can remain pink even after cooking to a safe minimum internal temperature of 165 °F. The meat of smoked turkey is always pink. Be particularly careful with foods prepared for infants, older adults, and persons with impaired immune systems.
- If served undercooked poultry in a restaurant, send it back to the kitchen for further cooking.
- Avoid cross-contaminating other foods. Uncooked meats and poultry should be kept separate from produce, cooked foods, and ready-to-eat foods. Hands, cutting boards, counters, knives, and other utensils should be washed thoroughly after touching uncooked foods. Hands should be washed before handling food, and between handling different food items.
- Refrigerate raw and cooked meat and poultry within 2 hours after purchase (1 hour if temperatures exceed 90° F). Refrigerate cooked meat and poultry within 2 hours after cooking. Refrigerators should be set to maintain a temperature of 40 °F or below.
- Persons who think they might have become ill from eating possibly contaminated ground turkey should consult their health care providers. Infants, older adults, and persons with impaired immune systems are more likely than others to develop severe illness.
Key Resources
- FoodSafety.gov
- AskKaren.gov (FSIS virtual representative)
- 1-888-MPHotline (1-888-674-6854), USDA English/Spanish Meat and Poultry Hotline
CDC’s Role in Food Safety
As an agency within the U.S. Department of Health and Human Services (HHS), CDC leads federal efforts to gather data on foodborne illnesses, investigate foodborne illnesses and outbreaks, and monitor the effectiveness of prevention and control efforts. CDC is not a food safety regulatory agency but works closely with the food safety regulatory agencies, in particular with HHS’s U.S. Food and Drug Administration (FDA) and the Food Safety and Inspection Service within the United States Department of Agriculture (USDA). CDC also plays a key role in building state and local health department epidemiology, laboratory, and environmental health capacity to support foodborne disease surveillance and outbreak response. Notably, CDC data can be used to help document the effectiveness of regulatory interventions.
Final Case Count Map
Persons infected with the outbreak strain of Salmonella Heidelberg, by state, as of November 7, 2011 (n=136)
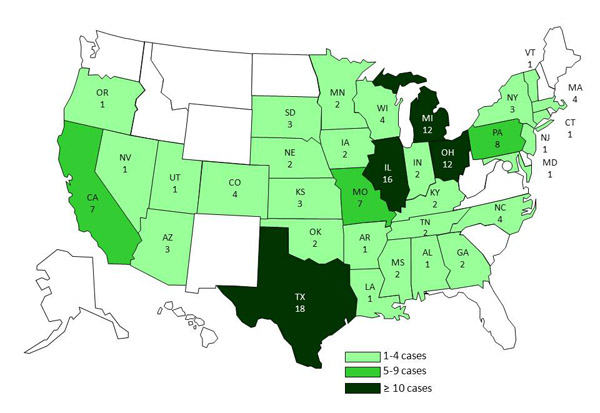
A total of 136 persons infected with the outbreak strain of Salmonella Heidelberg were reported from 34 states with illness onset dates between February 27 and September 13, 2011. The number of ill persons identified in each state was as follows: Alabama (1), Arkansas (1), Arizona (3), California (7), Colorado (4), Connecticut (1), Georgia (2), Illinois (16), Indiana (2), Iowa (2), Kansas (3), Kentucky (2), Louisiana (1), Massachusetts (4), Maryland (1), Michigan (12), Minnesota (2), Mississippi (2), Missouri (7), Nebraska (2), Nevada (1), New Jersey (1), New York (3), North Carolina (4), Ohio (12), Oklahoma (2), Oregon (1), Pennsylvania (8), South Dakota (3), Tennessee (2), Texas (18), Utah (1), Vermont (1), and Wisconsin (4).
Final Epi Curve
Persons infected with the outbreak strain of Salmonella Heidelberg, by week of illness onset*
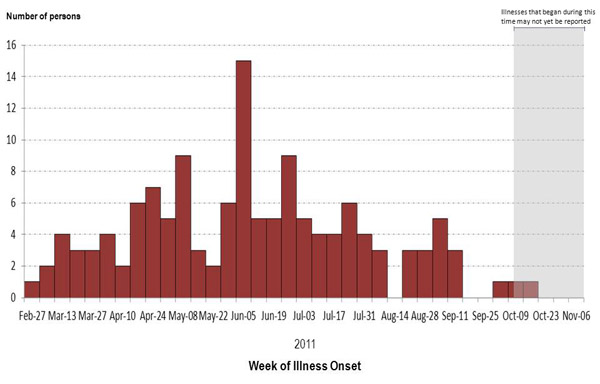
*n=134 for whom information was reported as of November 7, 2011. Onset data not currently available for all persons with reported illness.