CDC’s 6|18 Initiative State Medicaid Agency Activities
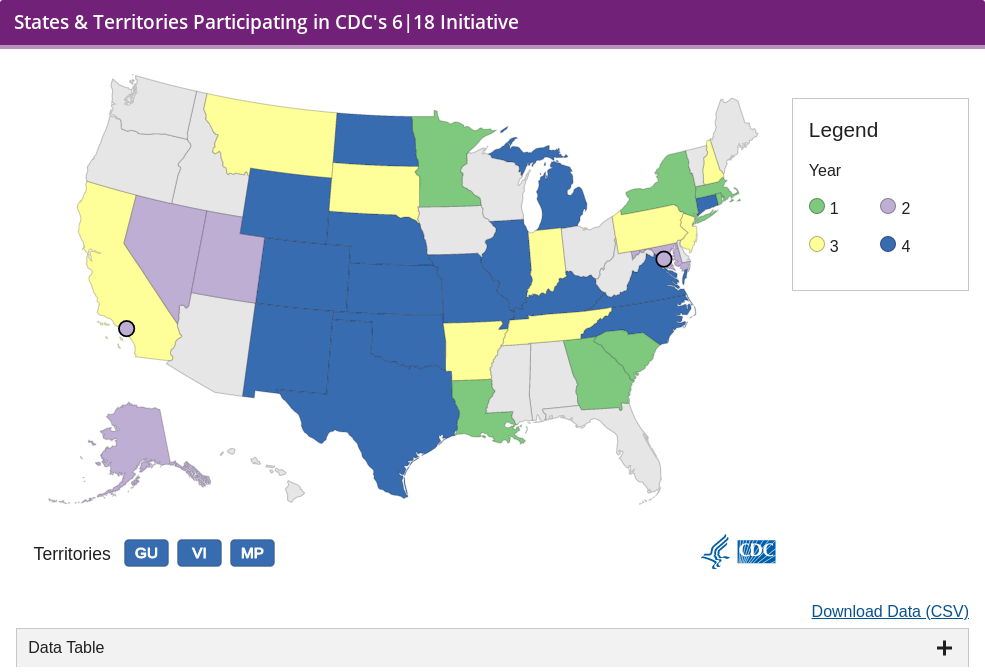
CDC is partnering with 34 Medicaid and public health teams from states, local jurisdictions, and territories to improve and accelerate implementation of the 6|18 Initiative interventions and achieve better care, better health outcomes, and lower costs.
Collectively, these teams have the potential to reach an estimated 47 million1, 2 Medicaid enrollees. CDC is working with external partners and these teams to understand best practices in implementing 6|18 interventions and to help disseminate these best practices to other states.
In year one (2016-2017), 9 state Medicaid agencies and Public Health Department teams implemented interventions for 3 of the 6 health conditions—asthma, tobacco use, and unintended pregnancy—because these conditions are particularly prevalent among Medicaid beneficiaries.
These 9 states started with the following factors critical for success:
- They had active efforts in place to control one or more of the 3 priority health conditions.
- They were working to implement the specific interventions highlighted within the set of 18.
- They had support for the partnership between the Medicaid Agency and the Department of Public Health working on this initiative together.
In year two (2017-2018), 6 additional state Medicaid agency and Public Health Department teams, the District of Columbia Health Department, and the Los Angeles Health Department initiated 6|18 efforts. These new entities joined the initiative to allow CDC to learn from agencies new to 6|18 interventions and to achieve more geographic diversity.
In year three (2018-2019), 18 teams joined the initiative, including 16 new states, one returning state and the Commonwealth of the Northern Mariana Islands. In years two and three, teams are selecting from any of the 6 health conditions and associated interventions.
In year four (2019-2020), 19 teams are participating in the initiative, including 6 new states and two new territories along with 13 returning states and local jurisdictions and one returning territory. Each team will focus on initiating or continuing efforts on multi-sector collaboration on one condition.
Technical Assistance
These state and local teams receive targeted technical assistance and opportunities for peer learning to support implementation through CDC, in partnership with the Robert Wood Johnson Foundation, and the Center for Health Care Strategies. Technical assistance includes:
- Individual team calls to discuss progress and identify challenges and technical assistance needs.
- Facilitated peer-to-peer learning calls focused on topics specific to each health condition.
- Webinars that address cross-cutting topics of interest to all states.
Additionally, CMS (Centers for Medicare & Medicaid Services), and national organizations such as ASTHO (Association of State and Territorial Health Officials), and George Washington University’s Center for Health Policy Research at the Milken Institute School of Public Health collaborate to support state and local teams implementing 6|18 interventions through the technical assistance system. Resources and tools that highlight best practices on how to most effectively use existing covered interventions have been developed to share with other state Medicaid programs and state and local health organizations. States use their own discretion to determine coverage for adult preventive services, since provision of preventive services for adults is optional under state Medicaid plans.
Evaluation
CDC is engaged with these teams and national partners in evaluative activities to monitor the quantitative, qualitative, and health and cost impact changes that occur as a result of this initiative.
For more information on progress and resources for the 6|18 Initiative, please visit the 6|18 Initiative website and the 6|18 Resource Center.
- https://data.medicaid.gov/Enrollment/2018-07-Preliminary-applications-eligibility-deter/p9cb-6r9r/data
- https://www.medicaid.gov/medicaid/program-information/downloads/cms-64-enrollment-report-jul-aug-2016.pdf (The CNMI estimate in this footnote includes both Medicaid and CHIP enrollees)