2016 STD Prevention Conference Highlights
Expedited Partner Therapy
The 2016 STD Prevention Conference showcases the latest STD prevention research, both from the United States and abroad.
This page highlights one presentation and three scientific posters focusing on expedited partner therapy (EPT), which is also called patient-delivered partner therapy (PDPT). While EPT is an effective prevention intervention, this research explores uptake, barriers to implementation, and what more is needed to ensure it has the greatest impact.
Poster or presentation images, as well as full abstracts and related links follow below.

- Reinfection with chlamydia and gonorrhea is a serious problem. As many as 1 in 4 young women treated for chlamydia becomes infected again within one year.
- EPT is effective — studies have shown that patients whose partners received EPT were 29% less likely to be reinfected than those who simply told their partners to visit the doctor.
- EPT is legal in 40 states and potentially allowable in an additional eight states and Puerto Rico.
EPT Abstracts
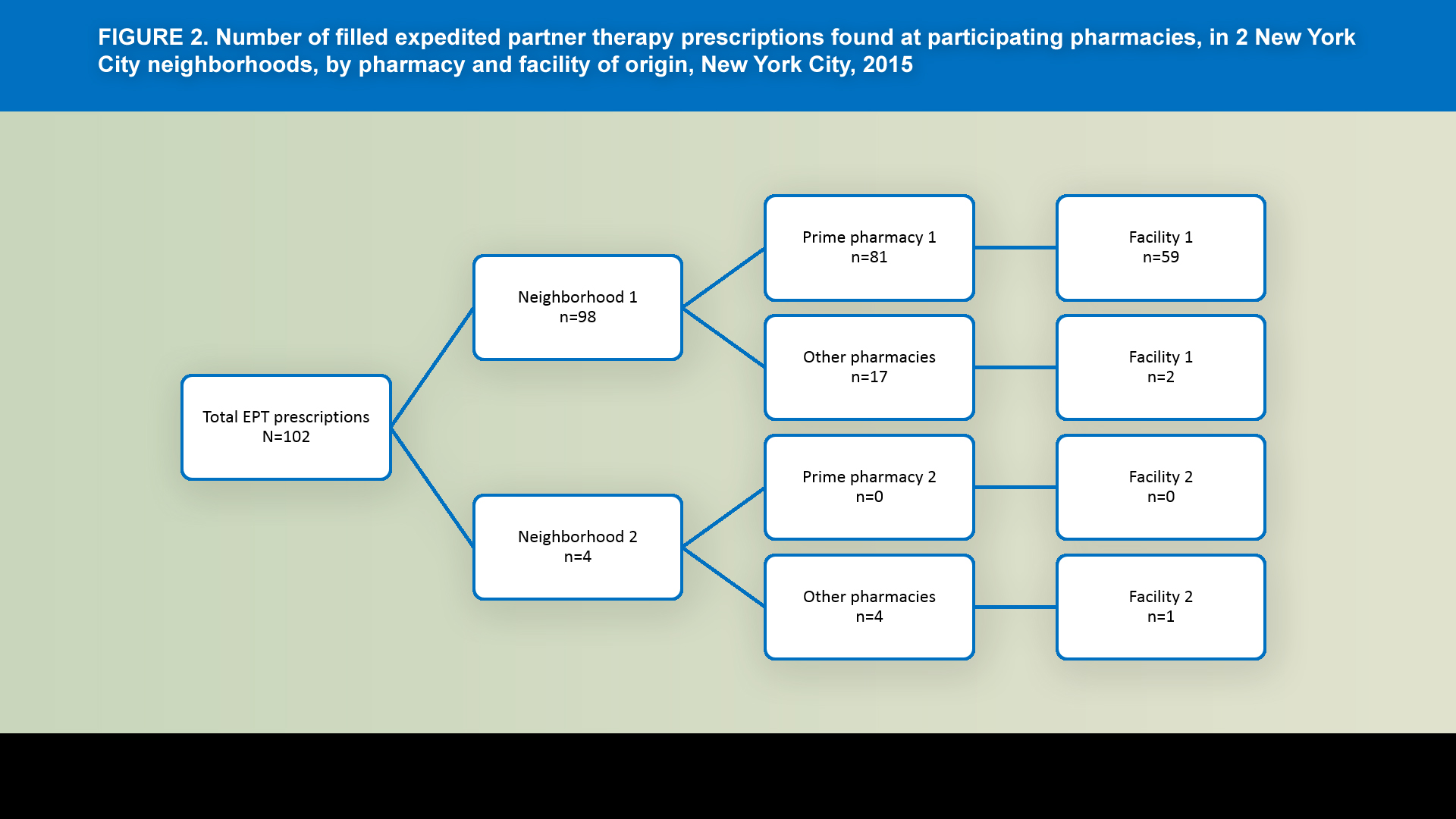
SENTINEL PHARMACY SURVEILLANCE FOR EXPEDITED PARTNER THERAPY PRESCRIPTIONS IN NEIGHBORHOODS WHERE PROVIDERS REGULARLY WRITE EXPEDITED PARTNER THERAPY PRESCRIPTIONS, NEW YORK CITY, 2016
Ebiere Okah, Vibhuti Arya, Meighan Rogers, Michelle Kim, Julia A. Schillinger
Background: Expedited partner therapy (EPT) for Chlamydia trachomatis (Ct) is the practice of providing (Ct)-infected patients with medication, or prescription (prescription-EPT) to deliver to their sex partners without first examining those partners. New York City (NYC) providers commonly employ prescription-EPT, yet NYC pharmacists report only occasional receipt of EPT prescriptions. This project assessed the frequency of EPT prescriptions filled in two NYC neighborhoods.
Methods: The two NYC facilities reporting the most frequent use of prescription-EPT were identified from Ct provider case reports and contacted to ascertain their EPT practices. Facility1 providers prescribed two 1-gram doses of azithromycin, including sex partner treatment on the index patient’s electronic prescription. Facility2 providers gave patients paper prescriptions for sex partners. We reviewed prescriptions filled in 2015 for Azithromycin, 1 or 2 grams at pharmacies near these facilities; prescriptions indicating partner therapy were classified “EPT prescriptions”.
Results: Twelve of 26 identified pharmacies agreed to participate. At 7 pharmacies near Facility1, we found 61 EPT prescriptions from Facility1 and 37 from other facilities. At 5 pharmacies near Facility2, we found only one EPT prescription from Facility2 and three from other facilities. Providers at the first facility (Facility1) submitted 112 Ct case reports indicating prescription-EPT, compared to 114 submitted by the second (Facility2).
Conclusion: EPT prescriptions were received in NYC pharmacies near to EPT-prescribing facilities, but with great variability and at a lower frequency than suggested by provider case reports. Provider EPT prescribing practices may impact the likelihood that partners receive medication, and should be further evaluated.
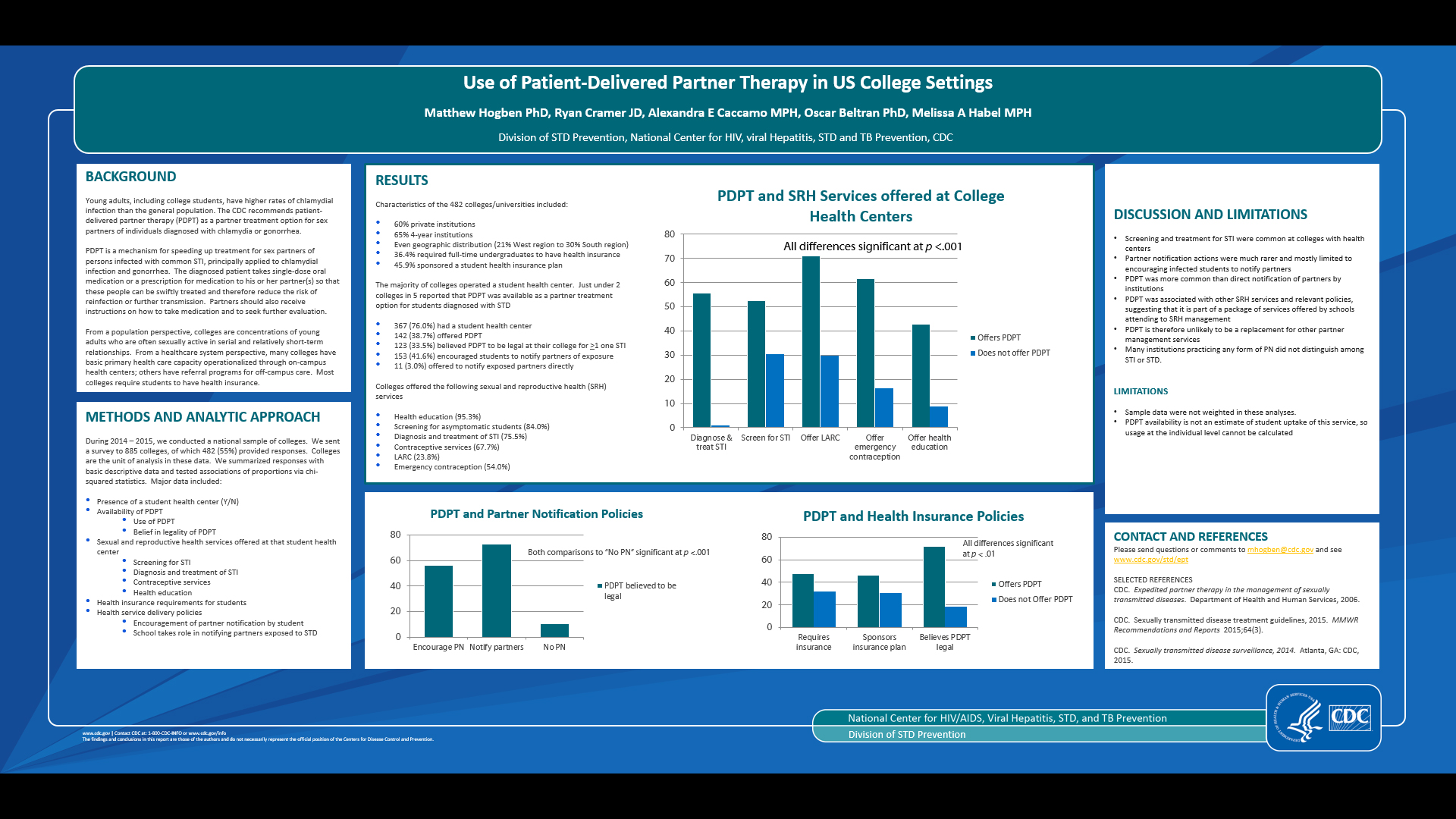
USE OF PATIENT-DELIVERED PARTNER THERAPY IN US COLLEGE SETTINGS
Matthew Hogben, PhD, Ryan Cramer, JD, MPH, Alexandra Caccamo, MPH, Oscar Beltran, PhD and Melissa Habel, MPH
Division of STD Prevention, Centers for Disease Control and Prevention, Atlanta
Background: Young adults, including college students, have higher rates of chlamydial infection than the general population. The CDC recommends patient-delivered partner therapy (PDPT) as a partner treatment option for sex partners of individuals diagnosed with chlamydia or gonorrhea. We examined college health center use of PDPT in a national sample of colleges.
Methods: Data were collected from 482 colleges (55%/885 surveyed) during 2014-2015. We asked whether the college had a student health center, which sexual and reproductive health (SRH) services were offered, and surveyed health insurance requirements and health service delivery policies. We compared PDPT availability to all other choices (no, don’t know, non-response) and measured associations between variables via chi-squares.
Results: Most colleges (n = 367, 76.0%) reported having a student health center; PDPT was available at 142 (38.7%) colleges. PDPT was significantly associated with availability of SRH services such as diagnosis and treatment of STI (55.7% vs. 0.9%), gynecological services (59.2% vs. 13.9%), and contraceptive services such as LARC (70.9% vs. 29.9%) and emergency contraception (61.5% vs. 16.2%), all p <.001. PDPT was more likely to be available at colleges that encouraged patient partner notification (56.3%) or notified partners directly (72.7%), than at schools without partner notification (10.6%), p <.001. PDPT availability was also associated with mandatory health insurance (47.7% vs. 32.1%), school-sponsored insurance plans (46.1% vs. 30.7%), and asymptomatic screening (52.6% vs. 30.4%), all p <.01. PDPT was offered in 71.5% of schools in states where the respondent believed PDPT was legal and in 18.2% – 36.4% of schools where the respondent believed PDPT was illegal, uncertain or other, p <.001.
Conclusions: PDPT was more likely to be available in colleges that offered SRH services and where staff believed PDPT was legal. Further research could explore the conditions under which PDPT is used (e.g., PDPT-related confidentiality policies).
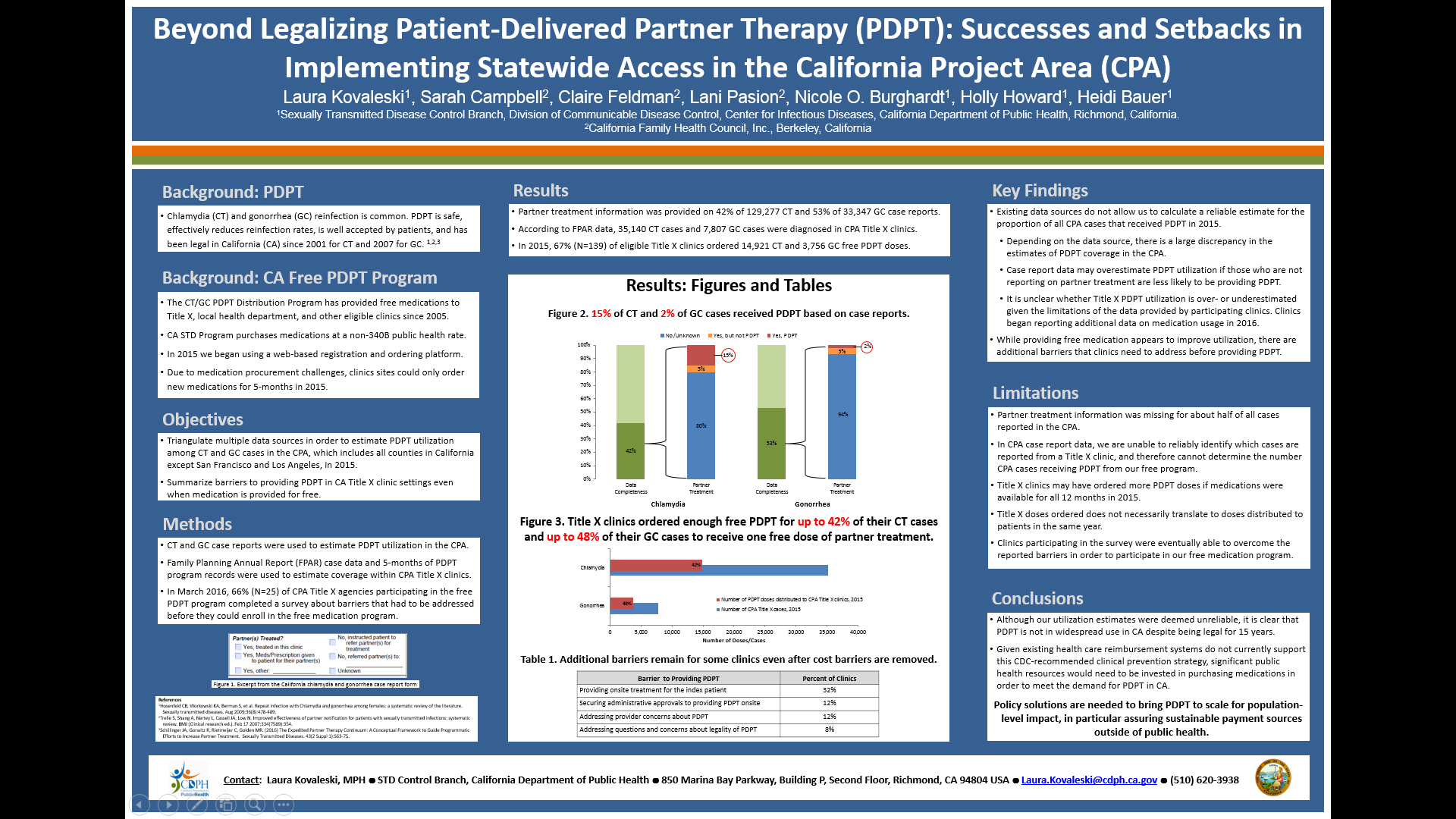
BEYOND LEGALIZING PATIENT-DELIVERED PARTNER THERAPY (PDPT) – SUCCESSES AND SETBACKS IN IMPLEMENTING STATEWIDE ACCESS IN THE CALIFORNIA PROJECT AREA (CPA)
Laura Kovaleski1, Sarah Campbell2, Claire Feldman2, Lani Pasion2, Nicole O. Burghardt1, Holly Howard1, Heidi Bauer1
1Sexually Transmitted Disease Control Branch, Division of Communicable Disease Control, Center for Infectious Diseases, California Department of Public Health, Richmond, California.
2California Family Health Council, Inc., Berkeley, California
Background: Chlamydia and gonorrhea (CT/GC) reinfection is common, and PDPT has demonstrated effectiveness in reducing reinfection rates. California legalized PDPT in 2001, however clinical practices still experience barriers to partner treatment, including lack of reimbursement. California Title X (TX) clinics can obtain a 6-month supply of free PDPT medication through a web-based program we developed. Assessing PDPT uptake and ongoing barriers can inform strategies for maximizing PDPT utilization.
Methods: We used case reports to estimate minimum PDPT utilization among CT/GC cases in the CPA in 2015. We used Family Planning Annual Report data and PDPT program records to estimate PDPT coverage within CPA TX settings. Medication procurement challenges required the PDPT program to close from February-August 2015, thus 5 months of program records were available for analysis. In March 2016, 66% (N=25) of CPA TX agencies completed a survey about barriers that had to be addressed before participating in the free program.
Results: Partner treatment information was completed on 42% of 129,277 chlamydia and 53% of 33,347 gonorrhea case reports. Among these, 15% (N=8,368) of chlamydia cases and 2% (N=272) of gonorrhea cases received PDPT. Despite program interruptions, 67% (N=139) of eligible CPA TX clinics ordered 14,921 chlamydia and 3,756 gonorrhea free medication doses. At one dose per case, this represents PDPT for up to 42% of 35,140 chlamydia and 48% of 7,807 gonorrhea annual CPA TX cases. Clinics reported barriers related to program requirements for on-site treatment of index patients (32%), administrative approvals (12%), provider concerns (12%), and legality questions (8%).
Conclusion: Obtaining legal status for PDPT has not led to widespread use in California. Addressing reimbursement barriers with a free program has improved coverage rates; however, additional barriers remain. Policy solutions are needed to bring PDPT to scale for population-level impact, in particular to assure sustainable payment sources outside of public health.
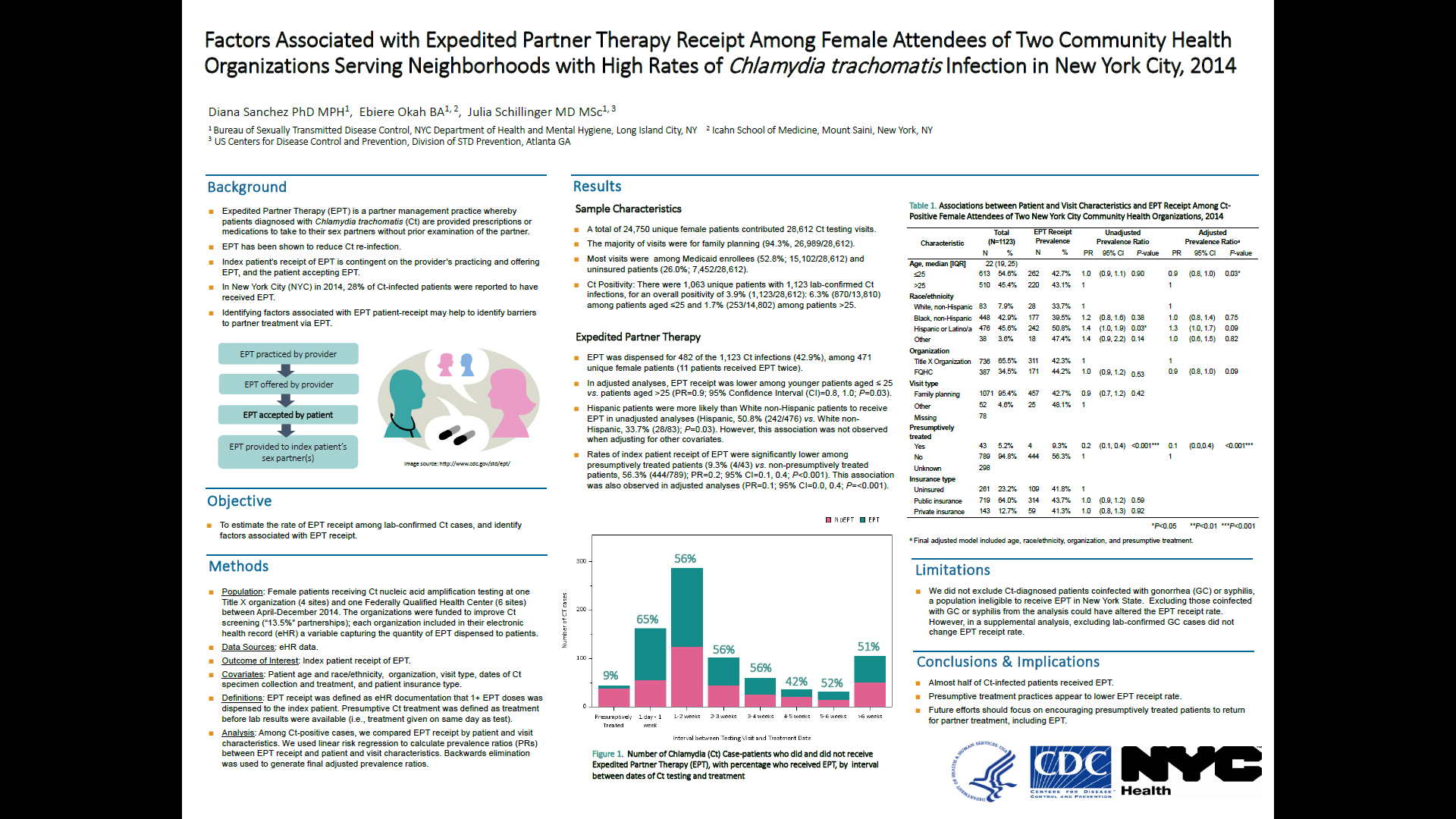
FACTORS ASSOCIATED WITH EXPEDITED PARTNER THERAPY RECEIPT AMONG FEMALE ATTENDEES OF TWO COMMUNITY HEALTH ORGANIZATIONS SERVING NEIGHBORHOODS WITH HIGH RATES OF CHLAMYDIA TRACHOMATIS INFECTION IN NEW YORK CITY, 2014
Diana Sanchez, PhD, MPH1, Ebiere Okah, BA2 and Julie Schillinger, MD, MSc3
1Bureau of Sexually Transmitted Diseases, New York City Department of Health and Mental Hygiene, Long Island City, 2School of Medicine, Icahn School of Medicine at Mount Sinai, New York, 3Bureau of Sexually Transmitted Disease Control, NYC Department of Health & Mental Hygiene/ Centers for Disease Control and Prevention, Long Island City
Background: Expedited Partner Therapy (EPT) has been shown to reduce Chlamydia trachomatis(Ct) re-infection. In New York City (NYC) in 2014, only 28% of Ct-infected patients were estimated to have received EPT. Identifying factors associated with patient-receipt of EPT is critical to improving EPT uptake.
Methods: We analyzed electronic health record data on Ct nucleic acid amplification testing performed between April-December2014 among women attending two high-volume community healthcare organizations with 8 sites throughout NYC. Extracted variables included: patient age and race/ethnicity, insurance status, clinic location, dates of Ct specimen collection and treatment, and whether EPT was dispensed. Among Ct-positive cases, we compared index patient EPT receipt by patient and visit characteristics.
Results: A total of 24,750 unique female patients contributed 28,612 Ct testing visits. There were 1,063 unique patients with 1,123 lab-confirmed Ct infections, for an overall positivity of 3.9% (1,123/28,612); 6.3% (870/13,810) among patients aged ≤25 and 1.7% (253/14,802) among patients >25. The majority of visits were for family planning (94.3%, 26,989/28,612), and among Medicaid enrollees (52.8%; 15,102/28,612) and uninsured patients (26.0%; 7,452/28,612). EPT was dispensed to 482 of the 1,123 Ct cases (42.9%), among 471 unique female patients (11 patients received EPT twice). Rates of index patient receipt of EPT were significantly lower among presumptively treated patients (presumptively treated patients, 9.3% (4/43) vs. non-presumptively treated patients, 56.3% (444/789); p<0.001). Hispanic patients were more likely than non-Hispanic patients to receive EPT (Hispanic, 47.7% (227/476) vs. non-Hispanic, 39.2% (223/569); p=0.006).
Conclusions: Less than half of Ct-infected patients received EPT, and EPT receipt varied considerably according to time of Ct treatment. Presumptively treated patients were unlikely to receive EPT, suggesting that future efforts should focus on encouraging those presumptively treated to return for partner treatment.