Vital Signs: ADHD in Young Children
Use recommended treatment first
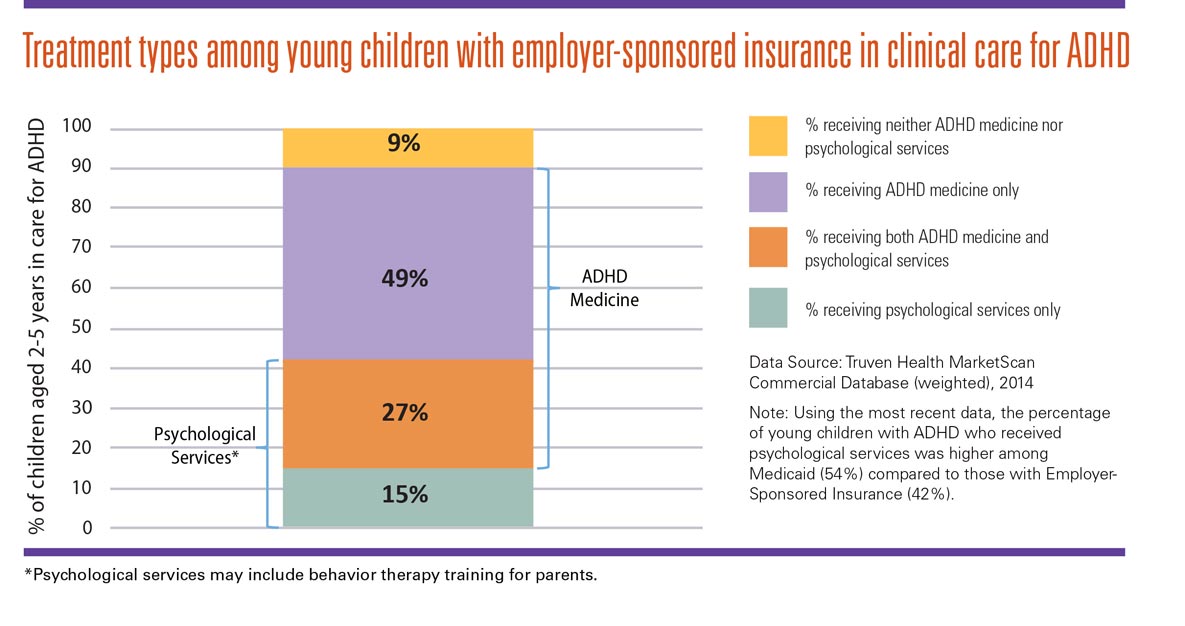
Treatment types among young children with employer-sponsored insurance in clinical care for ADHD
For children aged 2-5 years in care for ADHD:
- 9% receive neither ADHD medicine nor psychological services.
- 49% receive only ADHD medicine.
- 27% receive both ADHD medicine and psychological services.
- 15% receive psychological services only.
Refer parents of young children with ADHD for training in behavior therapy before prescribing medicine.
Steps for healthcare providers
- Assess a young child with ADHD symptoms using clinical practice guidelines.*
- Talk with parents about ADHD treatment and explain the benefits of behavior therapy.
- Improved behavior, self-control, and self-esteem for children.
- Better relationships and reduced stress for families.
- Benefits are lifelong for children and families.
- Refer parents to a therapist before prescribing medicine.** Find a therapist who:
- Teaches parents to better manage their child’s behavior and strengthen parent-child relationship.
- Encourages parents to practice between sessions, regularly monitors progress, and adjusts strategies as needed.
- Follow up with the family during and after treatment to confirm progress.
What parents can expect in behavior therapy
With the support of healthcare providers and therapists, parents can learn skills to help improve their child’s behavior, leading to improved functioning at school, home and in relationships. Parents typically attend 8 or more sessions with a therapist. Sessions may involve groups or individual families. Learning and practicing behavior therapy requires time and effort, but it has lasting benefits for the child.
The therapist meets regularly with the family to monitor progress and provide on-going support. Between sessions, parents practice using the skills they’ve learned from the therapist.
After therapy ends, families continue to experience improved behavior and reduced stress.
For more information about behavior therapy, go to: http://www.cdc.gov/ncbddd/adhd/behavior-therapy.html.
What parents learn when trained in behavior therapy
Parents learn positive communication, positive reinforcement, and structure and discipline.
*Clinical practice guidelines for primary care: http://bit.ly/1nCUenn; Clinical practice guidelines for child psychiatry: http://bit.ly/1UYugZ8
**In areas where behavioral treatments proven to work are not available, the healthcare provider should weigh the risks of starting medicine at an early age against the harm of delaying diagnosis and treatment, as recommended in the American Academy of Pediatrics practice guidelines.
