Vital Signs: Native Americans with Diabetes
Better diabetes care can decrease kidney failure
Native Americans (American Indians and Alaska Natives) have a greater chance of having diabetes than any other US racial group. Diabetes is the leading cause of kidney failure, a costly condition that requires dialysis or kidney transplant for survival. Kidney failure can be delayed or prevented by controlling blood pressure and blood sugar and by taking medicines that protect the kidneys. Good diabetes care includes regular kidney testing and education about kidney disease and treatment. Kidney failure from diabetes among Native Americans was the highest of any race. However, this has declined the fastest since the Indian Health Service (IHS) began using population health and team-based approaches to diabetes and kidney care, a potential model for other populations.
Health care systems can:
- Use population health approaches to diabetes care. Assess long-term outcomes and address disparities. Promote wellness of the entire community and connect people to local resources, including healthy food, transportation, housing, and mental health care.
- Develop a coordinated team approach to diabetes care. Team based-care should include patient education, community outreach, care coordination, tracking of health outcomes, and access to healthcare providers, nutritionists, diabetes educators, pharmacists, community health workers, and behavioral health clinicians.
- Integrate kidney disease prevention and education into routine diabetes care. Screen people with diabetes for kidney disease and make sure that kidney disease is routinely addressed as part of diabetes care.

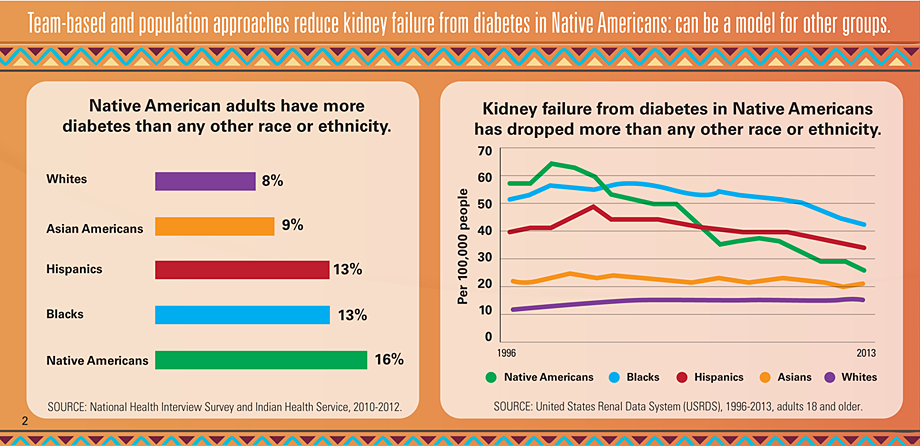
Native Americans are twice as likely as whites to have diabetes.
In about 2 out of 3 Native Americans with kidney failure, diabetes is the cause.
Kidney failure from diabetes dropped by 54% in Native Americans between 1996 and 2013.
Kidney failure from diabetes was highest among Native Americans.
Native Americans are more likely to have diabetes.
- Native Americans are twice as likely as whites to have been diagnosed with diabetes.
Native Americans were more likely to have kidney failure from diabetes than other races until recently.
- Native Americans were nearly 5 times more likely than whites to have kidney failure from diabetes in 1996.
- Reasons include: high blood sugar, high blood pressure, and significant barriers to health care.
Diabetes-related kidney failure among Native Americans decreased by 54% from 1996 to 2013.
- The Indian Health Service uses population health and team-based approaches to diabetes and kidney care.
- Native Americans with diabetes have had important improvements:
- Use of medicines to protect kidneys increased from 42% to 74% in 5 years.
- Average blood pressure in those with hypertension was well-controlled (133/76 mmHg).
- Blood sugar control improved by 10%.
- Kidney testing in those 65 and older was 50% higher compared to the Medicare diabetes population.
Kidney failure is a disabling and expensive complication of diabetes throughout the US.
- Medical costs for kidney failure from diabetes were about $82,000 per person in 2013.
- Medicare spent $14 billion to treat people with kidney failure from diabetes in 2013.
The Federal government is:
- Funding diabetes treatment and prevention services in Native American communities through the Special Diabetes Program for Indians.
- Improving diabetes outcomes for populations who receive direct health care from federal agencies, including Native Americans, veterans, and others.
- Assisting community health centers throughout the US to provide comprehensive diabetes care.
- Developing a comprehensive system for tracking chronic kidney disease (CKD).
Health care systems can:
- Use population health approaches to diabetes care. Assess long-term outcomes and address disparities. Promote wellness of the entire community and connect people to local resources, including healthy food, transportation, housing, and mental health care.
- Develop a coordinated team approach to diabetes care. Team based-care should include patient education, community outreach, care coordination, tracking of health outcomes, and access to healthcare providers, nutritionists, diabetes educators, pharmacists, community health workers, and behavioral health clinicians.
- Integrate kidney disease prevention and education into routine diabetes care. Screen people with diabetes for kidney disease and make sure that kidney disease is routinely addressed as part of diabetes care.
Health care policy leaders and insurers can:
- Set standards and track performance measures requiring health plans to assess the health of all members of their population with diabetes, including those who don’t regularly visit their healthcare provider.
- Promote CKD screening and monitoring and appropriate use of medicines that protect the kidneys in people with diabetes and CKD.
- Support team-based care, care management, patient education, home visits, and community outreach.
Patients with diabetes and their families can:
- Ask about being tested for kidney disease.
- Check their blood pressure and blood sugar regularly; talk with their healthcare provider about goals.
- Talk with their healthcare provider if they are having problems getting or taking their medicines.
- Reduce salt intake to lower blood pressure and protect their kidneys.
Issue Details
Issue Details
Other Sites
- MedlinePlus – Native American Health
- MedlinePlus – Diabetic Kidney Problems
- MedlinePlus – Diabetes
- American Association of Kidney Patients
- National Kidney Foundation
- Indian Health Service Homepage
- Division of Diabetes Treatment and Prevention
- Special Diabetes Program for Indians
- NIH National Institute of Diabetes and Digestive and Kidney Diseases
- National Kidney Disease Education Program
- NIH National Diabetes Education Program
- CMS’ Mapping Medicare Disparities tool
- American Diabetes Association
- ADA’s new 2017 Standards of Care
- VA/DOD Clinical Practice Guidelines: Management of Diabetes Mellitus (DM)
Science Behind the Issue
- Vital Signs Issue details: Native Americans with diabetes, Morbidity and Mortality Weekly Report (MMWR)
- Vital Signs – Native Americans with diabetes [PODCAST – 1:15 minutes]
- Vital Signs – Native Americans with diabetes [PSA – 0:60 seconds]
- CDC Diabetes Homepage
- CDC National Diabetes Education Program
- CDC CKD Surveillance
- CDC’s National Diabetes Prevention Program
- CDC Putting the Brakes on Diabetes Complications
- CDC AI/AN Resources