Vital Signs: Containing Unusual Resistance
Early, aggressive action can prevent spread
Free Continuing Education (CE) on Vital Signs: Containment of Novel Multidrug-Resistant Organisms and Resistance Mechanisms — United States, 2006–2017 (MMWR/Medscape) – available until June 27, 2019.
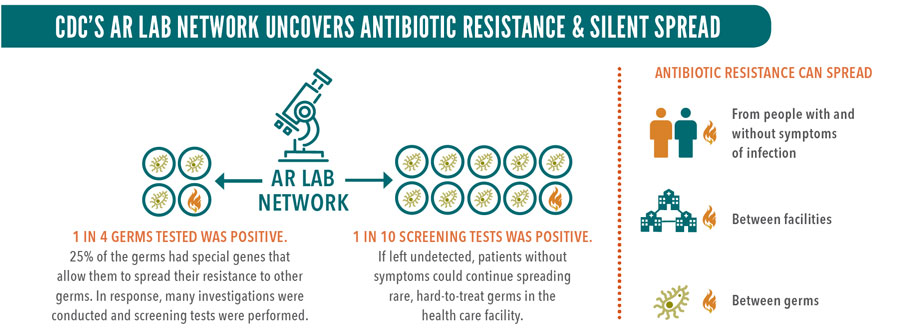
221. New nationwide testing in 2017 uncovered 221 instances of unusual resistance genes in “nightmare bacteria.”
1 in 10. 11% of screening tests, in people with no symptoms, found a hard-to-treat germ that spreads easily.
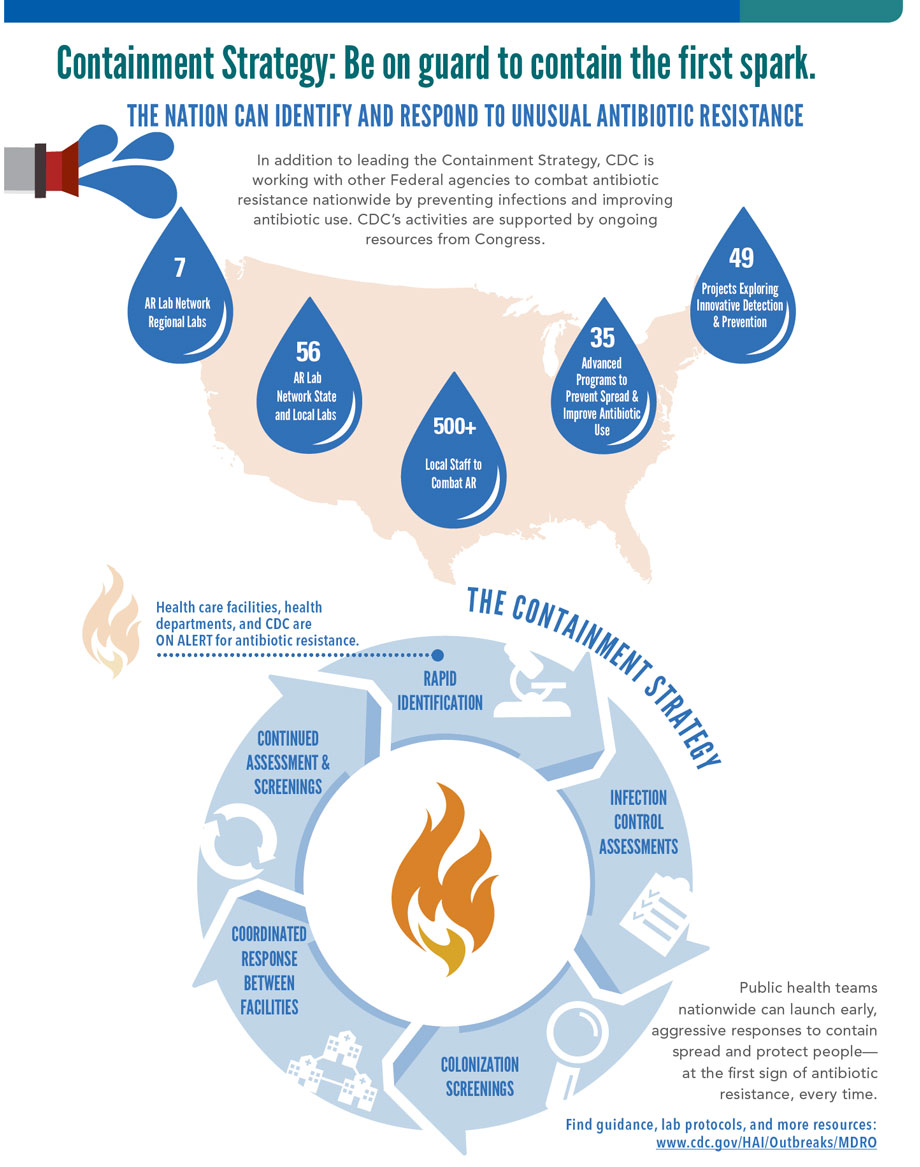
1st. The Containment Strategy keeps new threats from spreading. Launch at the first sign of unusual resistance.
More than 23,000 Americans die each year from infections caused by germs resistant to antibiotics. While antibiotic resistance (AR) threats vary nationwide, AR has been found in every state. And unusual resistance germs, which are resistant to all or most antibiotics tested and are uncommon or carry special resistance genes, are constantly developing and spreading. Lab tests uncovered unusual resistance more than 200 times in 2017 in “nightmare bacteria” alone. With new resources nationwide, early and aggressive action—when even a single case is found—can keep germs with unusual resistance from spreading in health care facilities and causing hard-to-treat or even untreatable infections. For example, CDC estimates show that this aggressive approach could prevent 1,600 cases of CRE* in one state over three years. Health departments can lead the Containment Strategy and act swiftly with health care facilities and CDC at the first sign of unusual resistance.
State and local health departments can:
- Make sure all health care facilities know what state and local lab support is available and what isolates (pure samples of a germ) to send for testing. Develop a plan to respond rapidly to unusual genes and germs when they first occur.
- Assess the quality and consistency of infection control in health care facilities across the state. Help improve practices.
- Coordinate with affected health care facilities, the new AR Lab Network regional labs, and CDC for every case of unusual resistance. Investigations should include onsite infection control assessments and colonization screenings for people who might have been exposed. They could spread it to others. Continue until spread is controlled.
- Provide timely lab results and recommendations to affected health care facilities and providers. If the patient came from or was transferred to another facility, alert that facility.
*CRE is carbapenem-resistant Enterobacteriaceae.

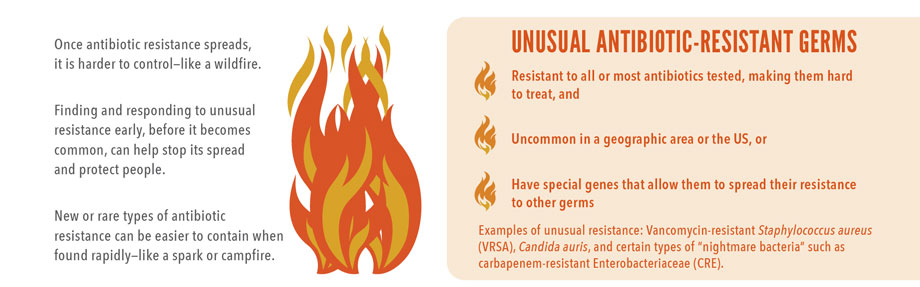
Antibiotic-resistant germs can spread like wildfire.
Germs constantly develop resistance against new and older antibiotics. Antibiotic-resistant germs can cause difficult-to-treat or untreatable infections. Some types of antibiotic resistance are already widespread.
View large image and text description
View large image and text description
Preventing an Unusual Antibiotic Resistance Wildfire
Rapid Response in Tennessee
- Health department identified an unusual resistance germ in a patient who recently received health care outside the US.
- Health department and the facility in Tennessee did infection control assessments and colonization screenings within 48 hours. No spread found.
- Moving forward, CDC’s AR Lab Network regional labs expanded services to test patients in the US with recent health care outside the country.
Ongoing Vigilance in Iowa
- Health department identified an unusual resistance germ in a nursing home patient.
- Health department and the facility did infection control assessments and screened 30 patients for colonization. Investigation revealed the germ may have spread to 5 additional people.
- Facility used infection control and contact precautions, such as gloves and gowns, to help stop spread.
- No further spread found during follow-up assessments.
SOURCE: CDC Vital Signs, April 2018.
The Federal Government is:
- Monitoring resistance and sounding the alarm when threats emerge. CDC develops and provides new lab tests so health departments can quickly identify new threats.
- Improving identification through CDC’s new AR Lab Network in all 50 states, 5 large cities, and Puerto Rico, including 7 regional labs and a national tuberculosis lab for specialty testing.
- Supporting prevention experts and programs in every state, and providing data and recommendations for local prevention and response.
- Testing innovative infection control and prevention strategies with health care and academic partners.
State and Local Health Departments and Labs can:
- Make sure all health care facilities know what state and local lab support is available and what isolates (pure samples of a germ) to send for testing. Develop a plan to respond rapidly to unusual genes and germs when they first appear.
- Assess the quality and consistency of infection control in health care facilities across the state, especially in facilities with high-risk patients and long stays. Help improve practices.
- Coordinate with affected health care facilities, the new AR Lab Network regional lab, and CDC for every case of unusual resistance. Investigations should include onsite infection control assessments to find spread. Consider colonization screenings. Continue until spread is controlled.
- Provide timely lab results and recommendations to affected health care facilities and providers. If the patient came from or was transferred to another facility, alert that facility.
- Find resources: www.cdc.gov/hai/outbreaks/mdro
Health Care Facilities can:
- Plan for unusual resistance arriving in your facility. Find resources: www.cdc.gov/hai/outbreaks/mdro
- Leadership: Work with the health department to stop spread of unusual resistance. Review and support infection control in the facility.
- Clinical labs: Know what isolates to send for testing. Establish protocols that immediately notify the health department, health care provider, and infection control staff of unusual resistance. Validate new tests to identify the latest threats. If needed, use isolates from wwwn.cdc.gov/arisolatebank/.
- Healthcare providers, epidemiologists, and infection control staff: Place patients with unusual resistance on contact precautions, assess and enhance infection control, and work with the health department to screen others. Communicate about status when patients are transferred. Continue infection control assessments and colonization screenings until spread is controlled. Ask about any recent travel or health care to identify at-risk patients.
Everyone can:
- Inform your health care provider if you recently received health care in another country or facility.
- Talk to your health care provider about preventing infections, taking good care of chronic conditions and getting recommended vaccines.
- Practice good hygiene, such as keeping hands clean with handwashing or alcohol-based hand rubs, and keep cuts clean until healed.
Related Pages
- Vital Signs Issue details: Containment of Novel Multidrug-Resistant Organisms and Resistance Mechanisms – United States, 2006-2017 Morbidity and Mortality Weekly Report (MMWR)
- CDC: Interim Guidance for a Health Response to Contain Novel or Targeted Multidrug-resistant Organisms (MDROs)
- CDC: Drug Resistance Laboratories
- CDC: Antibiotic/Antimicrobial Resistance
- CDC: Antibiotic Resistance Investments
- CDC: Antibiotic Resistance Threats in the United States, 2013
- CDC: Investing in States: Maps
- CDC: Vital signs: preventing antibiotic-resistant infections in hospitals—United States, 2014.
Other Sites
- MedlinePlus – Antibiotic Resistance
- Carbapenem-Resistant Enterobacteriaceae: A Strategic Roadmap for Infection Control.
- The Problem of Carbapenemase-Producing-Carbapenem-Resistant-Enterobacteriaceae Detection.