Vital Signs: Opioid Overdoses Treated in Emergency Departments
Identify opportunities for action
- Webinar featuring the 20th US Surgeon General, Acting CDC Director, and other clinical and public health professionals
Archived at Clinician Outreach and Communication Activity (COCA) (“Call Materials”) and CDC’s Office for State, Tribal, Local, and Territorial Support (OSTLTS) (Downloads)
FREE Continuing Education (CE) available until April 17, 2020 - Annals of Emergency Medicine Article – Opportunities for Prevention and Intervention of Opioid Overdose in the Emergency Department
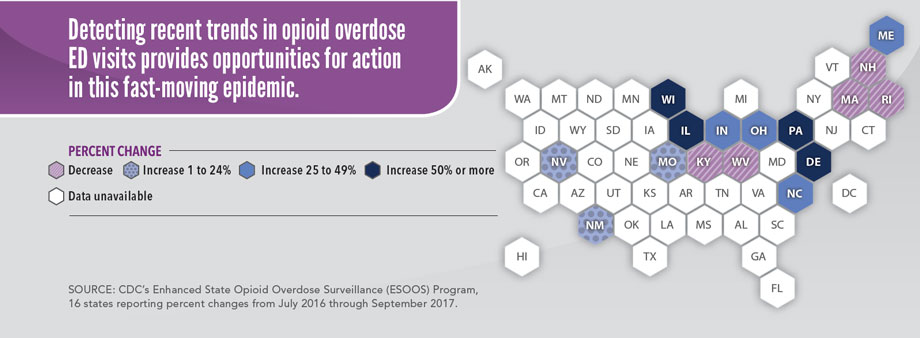
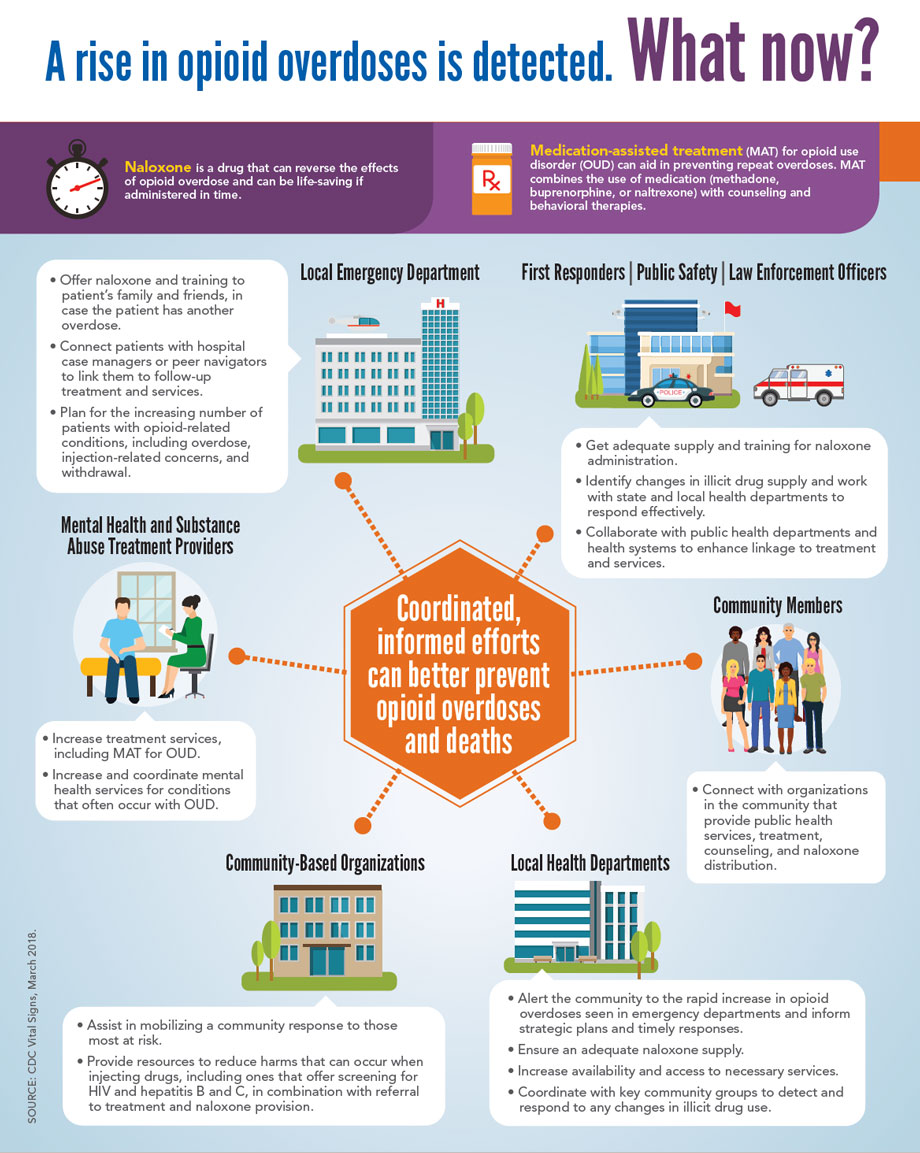
Emergency department (ED) visits for opioid* overdoses rose 30% in all parts of the US from July 2016 through September 2017. People who have had an overdose are more likely to have another, so being seen in the ED is an opportunity for action. Repeat overdoses may be prevented with medication-assisted treatment (MAT) for opioid use disorder (OUD), which is defined as a problematic pattern of opioid use. EDs can provide naloxone, link patients to treatment and referral services, and provide health departments with critical data on overdoses. ED data provide an early warning system for health departments to identify increases in opioid overdoses more quickly and coordinate response efforts. This fast-moving epidemic does not stay within state and county lines. Coordinated action between EDs, health departments, mental health and treatment providers, community-based organizations, and law enforcement can prevent opioid overdose and death.
30% Opioid overdoses went up 30% from July 2016 through September 2017 in 52 areas in 45 states.
70% The Midwestern region witnessed opioid overdoses increase 70% from July 2016 through September 2017.
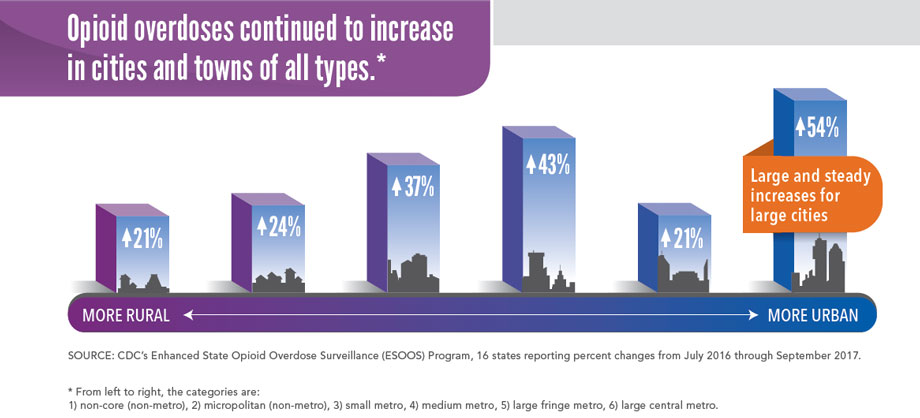
54% Opioid overdoses in large cities increased by 54% in 16 states.
Health departments can:
- Alert communities to rapid increases in overdoses seen in EDs for an informed and timely response.
- Increase naloxone distribution (an overdose-reversing drug) to first responders, family and friends, and other community members in affected areas, as policies permit.
- Increase availability of and access to treatment services, including mental health services and MAT for OUD.
- Support programs which reduce harms from injecting opioids, including those offering screening for HIV and hepatitis B and C, in combination with referral to treatment.
- Support the use of the CDC Guideline for Prescribing Opioids for Chronic Pain, which encourages using prescription drug monitoring programs (PDMPs) to inform clinical practice. https://go.usa.gov/xn6uQ
*Opioids include prescription pain medications, heroin, and illicitly manufactured fentanyl.

Opioid overdose ED visits continued to rise from 2016 to 2017.
From July 2016 through September 2017, opioid overdoses increased for:
- Men (↑30%) and women (↑24%)
- People ages 25-34 (↑ 31%), 35-54 (↑36%), and 55 and over (↑32%)
- Most states (↑ 30% average), especially in the Midwest (↑70% average)
SOURCE: CDC’s National Syndromic Surveillance Program, 52 jurisdictions in 45 states reporting.
The Federal Government is:
- Tracking overdose trends to better understand and more quickly respond to the opioid overdose epidemic.
- Improving access to OUD treatment, such as MAT, and overdose-reversing drugs, such as naloxone.
- Educating healthcare providers and the public about OUD and opioid overdose, and providing guidance on safe and effective pain management.
- Equipping states with resources to implement and evaluate safe prescribing practices.
- Coordinating actions to reduce production and impacts of the illicit opioid supply in the US through the High Intensity Drug Trafficking Areas (HIDTA) Program.
- Supporting cutting-edge research to improve pain management and OUD treatment.
Health Departments can:
- Alert communities to rapid increases in overdoses seen in EDs for an informed and timely response.
- Increase naloxone distribution (an overdose-reversing drug) to first responders, family and friends, and other community members in affected areas, as policies permit.
- Increase availability of and access to treatment services, including mental health services and MAT for OUD.
- Support programs that reduce harms which can occur when injecting opioids, including those offering screening for HIV and hepatitis B and C, in combination with referral to treatment.
- Support the use of the CDC Guideline for Prescribing Opioids for Chronic Pain, which encourages using prescription drug monitoring programs (PDMPs) to inform clinical practice. https://go.usa.gov/xn6uQ
Emergency Departments can:
- Develop post-opioid overdose protocols, which may include
- Offering overdose prevention education, naloxone, and related training for patients, family members, and friends.
- Linking patients to treatment and services in the community as needed.
- Starting MAT in the ED
Healthcare Providers can:
- Prescribe opioids only when benefits are likely to outweigh risks.
- Determine a patient’s prescription drug history and level of risk by accessing data from their state PDMP.
- Identify mental health, social services, and treatment options to provide appropriate care for patients who have OUD.
- Follow the CDC Guideline for Prescribing Opioids for Chronic Pain. https://go.usa.gov/xn6uQ
Everyone can:
- Learn about the risks of opioids. https://go.usa.gov/xn6um
- Learn about naloxone, its availability, and how to use it. https://go.usa.gov/xn6uV
- Store prescription opioids in a secure place, out of reach of others (including children, family, friends, and visitors).
- Contact SAMHSA’s National Helpline: 1-800-662-HELP for anyone who has trouble with opioid use. https://go.usa.gov/xn6uw
Related Pages
- Vital Signs – Opioid Overdoses Treated in Emergency Departments [PODCAST – 1:15 minutes]
- Vital Signs – Opioid Overdoses Treated in Emergency Departments [PSA – 0:60 seconds]
- Morbidity and Mortality Weekly Report (MMWR): Vital Signs: Trends in Emergency Department Visits for Suspected Opioid Overdoses — United States, July 2016–September 2017
- CDC’s National Syndromic Surveillance Program (NSSP) BioSense Platform
- CDC’s Enhanced State Opioid Overdose Surveillance (ESOOS) Program
- CDC’s Prevention for States (PfS) Program
- Vital Signs, 2017: Opioid Prescribing: Where You Live Matters
- Vital Signs, 2015: Today’s Heroin Epidemic: More People at Risk, Multiple Drugs Abused
- CDC Opioid Overdose Website
- CDC’s Rx Awareness Campaign
- CDC Webinar: Coordinating Clinical and Public Health Responses to Opioid Overdoses Treated in Emergency Departments
- CDC’s Town Hall Teleconference
- CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016
- Healthcare Provider Resources
- Online Training: Applying CDC’s Guideline for Prescribing Opioids
- CDC Opioid Prescribing Guideline Mobile App
- Pocket Guide: Tapering Opioids for Chronic Pain [1.78 MB], 4 pages
- Factsheet: Prescription Drug Monitoring Programs (PDMPs) [7.89 MB], 2 pages
- Factsheet: Nonopioid Treatments for Chronic Pain [1.53 MB], 2 pages
- Patient Materials
- Resource Center
- Healthcare Provider Resources
- CDC Learning Connection: Hot Training Topic
Other Sites
- U.S. Department of Health & Human Services Strategy for Fighting Opioid Crisis
- Office of National Drug Control Policy
- Office of the U.S. Surgeon General
- PDMP Center of Excellence, Brandeis University
- Providers’ Clinical Support System
- MedlinePlus – Prescription Drug Abuse
- Office of the National Coordinator for Health Information Technology (ONC) – Linking PDMPs to Health IT
- National Alliance for Model State Drug Laws