Vital Signs: Opioid Overdoses Treated in Emergency Departments
Vital Signs: Opioid Overdoses Treated in Emergency Departments
Identify opportunities for action
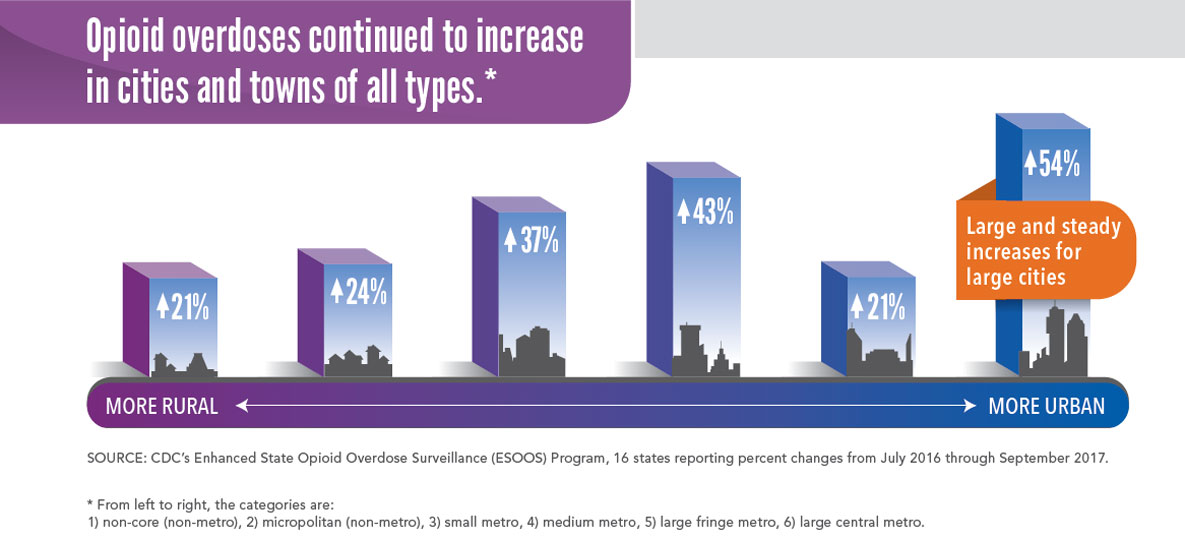
Opioid overdoses continued to increase in cities and towns of all types.*
* From left to right, the categories are:
- Non-core (non-metro): 21 percent increase
- Micropolitan (non-metro): 24 percent increase
- Small netro: 37 percent increase
- Medium metro: 43 percent increase
- Large fringe metro: 21 percent increase
- Large central metro: 54 percent increase – Large and steady increase for large cities
SOURCE: CDC’s Enhanced State Opioid Overdose Surveillance (ESOOS) Program, 16 states reporting percent changes from July 2016 through September 2017.
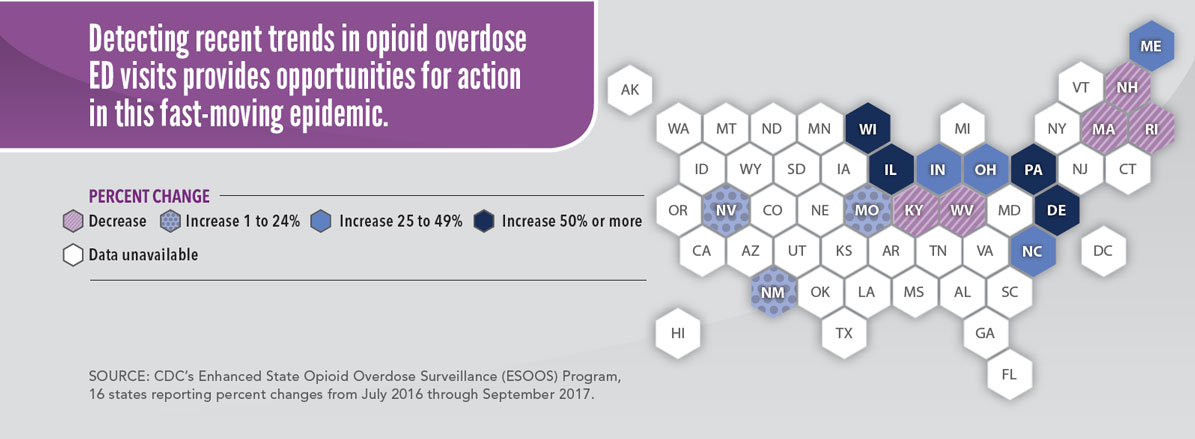
| State | Percentage Change |
| Alabama | Data unavailable |
| Alaska | Data unavailable |
| Arizona | Data unavailable |
| Arkansas | Data unavailable |
| California | Data unavailable |
| Colorado | Data unavailable |
| Connecticut | Data unavailable |
| Delaware | Increase 50% or more |
| District of Columbia | Data unavailable |
| Florida | Data unavailable |
| Georgia | Data unavailable |
| Hawaii | Data unavailable |
| Idaho | Data unavailable |
| Illinois | Increase 50% or more |
| Indiana | Increase 25 to 49% |
| Iowa | Data unavailable |
| Kansas | Data unavailable |
| Kentucky | Decrease |
| Louisiana | Data unavailable |
| Maine | Increase 25 to 49% |
| Maryland | Data unavailable |
| Massachusetts | Decrease |
| Michigan | Data unavailable |
| Minnesota | Data unavailable |
| Mississippi | Data unavailable |
| Missouri | Increase 1 to 24% |
| Montana | Data unavailable |
| Nebraska | Data unavailable |
| Nevada | Increase 1 to 24% |
| New Hampshire | Decrease |
| New Jersey | Data unavailable |
| New Mexico | Increase 1 to 24% |
| New York | Data unavailable |
| North Carolina | Increase 25 to 49% |
| North Dakota | Data unavailable |
| Ohio | Increase 25 to 49% |
| Oklahoma | Data unavailable |
| Oregon | Data unavailable |
| Pennsylvania | Increase 50% or more |
| Rhode Island | Decrease |
| South Carolina | Data unavailable |
| South Dakota | Data unavailable |
| Tennessee | Data unavailable |
| Texas | Data unavailable |
| Utah | Data unavailable |
| Vermont | Data unavailable |
| Virginia | Data unavailable |
| Washington | Data unavailable |
| West Virginia | Decrease |
| Wisconsin | Increase 50% or more |
| Wyoming | Data unavailable |
SOURCE: CDC’s Enhanced State Opioid Overdose Surveillance (ESOOS) Program, 16 states reporting percent changes from July 2016 through September 2017.
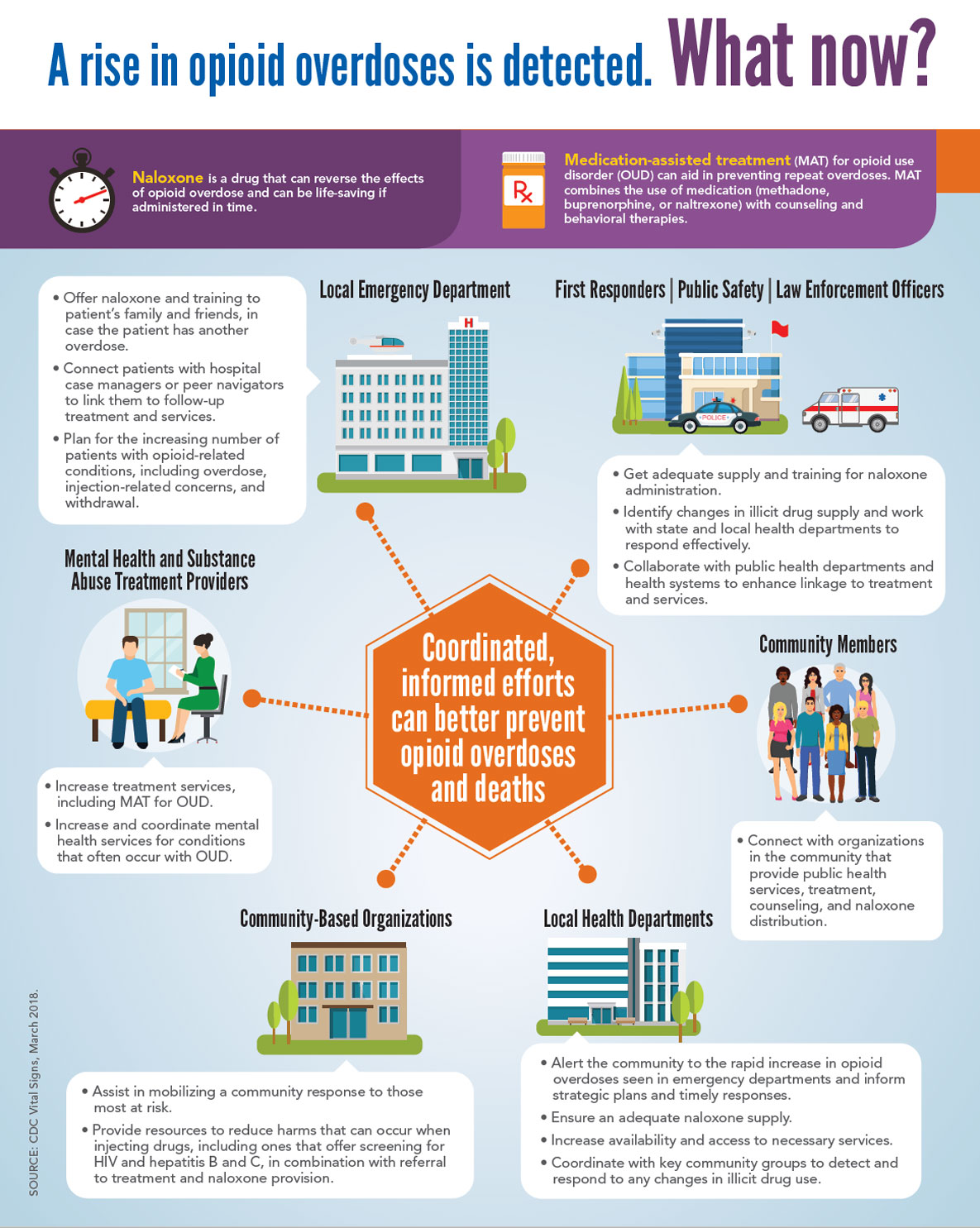
A rise in opioid overdoses is detected. What now?
Naloxone is a drug that can reverse the effects of opioid overdose and can be life-saving if administered in time.
Medication-assisted treatment (MAT) for opioid use disorder (OUD) can aid in preventing repeat overdoses. MAT combines the use of medication (methadone, buprenorphine, or naltrexone) with counseling and behavioral therapies.
Coordinated, informed efforts can better prevent opioid overdoses and deaths
Local Emergency Department
- Offer naloxone and training to patient’s family and friends, in case the patient has another overdose.
- Connect patients with hospital case managers or peer navigators to link them to follow-up treatment and services.
- Plan for the increasing number of patients with opioid-related conditions, including overdose, injection-related concerns, and withdrawal.
First Responders | Public Safety | Law Enforcement Officers
- Get adequate supply and training for naloxone administration.
- Identify changes in illicit drug supply and work with state and local health departments to respond effectively.
- Collaborate with public health departments and health systems to enhance linkage to treatment and services.
Mental Health and Substance Abuse Treatment Providers
- Increase treatment services, including MAT for OUD.
- Increase and coordinate mental health services for conditions that often occur with OUD.
Community Members
- Connect with organizations in the community that provide public health services, treatment, counseling, and naloxone distribution.
Community-Based Organizations
- Assist in mobilizing a community response to those most at risk.
- Provide resources to reduce harms that can occur when injecting drugs, including ones that offer screening for HIV and hepatitis B and C, in combination with referral to treatment and naloxone provision.
Local Health Departments
- Alert the community to the rapid increase in opioid overdoses seen in emergency departments and inform strategic plans and timely responses.
- Ensure an adequate naloxone supply.
- Increase availability and access to necessary services.
- Coordinate with key community groups to detect and respond to any changes in illicit drug use.
