Domestic HIV/AIDS Surveillance: Current Trends and Status of State HIV Reporting
CDC Congressional Testimony
April 27, 2006
Committee on Energy and Commerce, Subcommittee on Health, United States House of Representatives
Statement of:
Kevin Fenton, M.D., Ph.D.
Director
National Center for HIV, STD, and TB Prevention
Coordinating Center for Infectious Diseases
Centers for Disease Control and Prevention
U.S. Department of Health and Human Services
Introduction
Good morning Mr. Chairman and Members of the Subcommittee. My name is Kevin Fenton and I am Director of the National Center for HIV, STD, and TB Prevention at the Centers for Disease Control and Prevention (CDC). I am accompanied by Matt McKenna, Chief of the Center′s HIV Incidence &
Case Surveillance Branch. Thank you for the opportunity to discuss current trends in HIV/AIDS in the United States and the status of state HIV surveillance systems.
Twenty-five years ago, the first cases of AIDS were reported in the United States. HIV and AIDS remains one of the greatest public health challenges today. To date, HIV has claimed the lives of more than 22 million people worldwide, and in the United States, more than 500,000 people have died of AIDS. The number of new HIV infections annually has declined from more than 150,000 in the late 1980s to an estimated 40,000 per year today.An estimated 1 – 1.2 million people currently are living with HIV/AIDS in the United States. Due to more effective treatment, people are living longer and healthier lives after a diagnosis of HIV. Despite the growing pool of persons capable of transmitting the virus, the number of persons becoming newly infected each year has remained constant over the last 10 years, at approximately 40,000 new infections per year.
While the struggle to prevent new HIV infections is not over, there have been some major successes. For instance, the dramatic decrease in mother to child (perinatal) HIV transmission is one of the great success stories of HIV prevention. Since the beginning of the epidemic, the number of infants infected with HIV through mother-to-child transmission has decreased by almost 90%, from an estimated peak of 1,750 HIV-infected infants born each year during the early to mid-1990s to between 140 and 230 infants in 2002. These declines are due to multiple interventions, including routine voluntary HIV testing of pregnant women, the use of rapid HIV tests at delivery for women of unknown HIV status, and the use of antiretroviral therapy by HIV-infected women during pregnancy and infants after birth.
We have also seen declines in the number of HIV and AIDS cases attributed to injection drug use. For example, the number of AIDS cases attributed to injection drug use has declined by about 15% from 2000 to 2004. In addition to the dramatic decline in the occurrence of new cases since the beginning of the epidemic, the HIV/AIDS epidemic has changed in other important ways. In the early days of the epidemic, the greatest number of new infections was found among white men who have sex with men (MSM) and among injection drug users. Today, while men who have sex with men overall still account for the largest percentage of new HIV infections, the epidemic has expanded to have a growing impact on racial and ethnic minorities (particularly African Americans). During 2001-2004 in 35 areas with HIV case reporting, 51% of all new HIV/AIDS diagnoses were in African Americans. The epidemic is also affecting more women. Early in the epidemic, HIV infection and AIDS were diagnosed for relatively few women and female adolescents. Today, women account for more than one quarter of all new HIV/AIDS diagnoses. Women of color are especially affected by HIV infection and AIDS, and in 2002 (the most recent year available) HIV infection was the leading cause of death for African American women aged 2534 years.
Of great concern to us is the approximately 25 percent of persons with HIV who do not know they are infected. We believe that infections transmitted from this group account for more than half of new HIV infections each year, underscoring the rationale for our substantially increased efforts to reach at-risk communities with HIV testing services. When people know their status they are more likely to protect their partners from infection. Knowledge of one′s HIV infection can help prevent the spread of HIV to others.
HIV surveillance in the United States
A robust surveillance system provides a strong foundation for good public health programs.Surveillance data are crucial to informing and guiding effective and evidence-based prevention efforts.Surveillance for HIV/AIDS has evolved over time in response to changes in the epidemic, development in diagnostics, technologies and treatments.Initial surveillance was for AIDS cases, but as new diagnostic tools have become available, and our understanding of the disease pathogenesis has evolved, so too have our methods for surveillance. Today, surveillance of HIV/AIDS is among the most complex for any infectious diseaserelying upon multiple methods, data sources and analytic techniques. Having accurate information about the HIV epidemic requires obtaining information about several important events over the life of a case, from initial infection, through diagnosis, to clinical and laboratory markers of illness, through death.
CDC is responsible for ensuring the integrity of the national HIV/AIDS surveillance system to accurately monitor the epidemic in the United States. CDC provides funding, technical assistance, and coordinates activities with states to aggregate data that constitute the national system. CDC also issues recommended security and confidentiality policies and procedures to state and local surveillance programs that are consistent with the agency standards for the security of surveillance data.CDC requires that recipients of federal funds for HIV/AIDS surveillance establish the minimum security standards and include their security policy in applications for surveillance funds. As with other diseases, individual state governments have authority for statutory and regulatory issues for HIV/AIDS reporting and data protection, including the decision regarding what type of system will be used for disease reporting, such as name-based or code-based. Except for HIV, all other reported infectious diseases, including AIDS, are routinely reported to states using name-based reporting systems. It is important to note, for confidentiality purposes, that the CDC does not receive the names of individuals. This information resides with public health authorities at the state level.
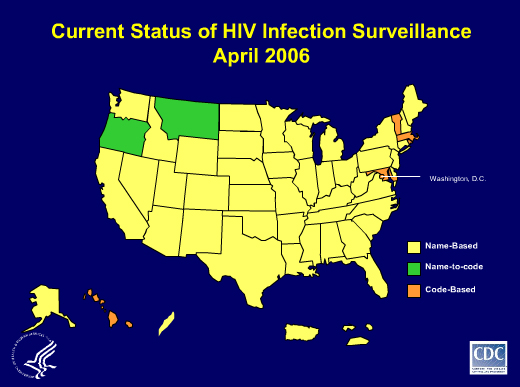
Since the beginning of the epidemic, AIDS surveillance has been a cornerstone of national, state, and local efforts to monitor the scope and impact of the HIV epidemic. AIDS surveillance data, however, no longer accurately describe the full extent of the epidemic, as effective therapies have slowed the progression of HIV disease. Since 1999, CDC has advised states to conduct HIV reporting using the same name-based approach currently used for AIDS surveillance nationwide. Currently, 43 states use confidential name-based HIV case reporting. The remaining seven states and the District of Columbia use code or name-to-code reporting. Among those eight areas there are seven different codes. Several of the remaining states have notified CDC that they intend to implement name-based HIV surveillance in 2006. In fact, on April 17, 2006, the Governor of California signed into law SB 669 which has moved the state from a code-based to an integrated name-based reporting system.
Use of HIV/AIDS Data
CDC′s HIV/AIDS surveillance system is the nation′s key source of information used to track the epidemic. Surveillance activities provide demographic, laboratory, clinical and behavioral risk data that are used to identify populations at greatest risk for HIV infection.There are three primary uses of surveillance data: 1) epidemic monitoring, including estimates of incidence and prevalence of HIV and AIDS in the population, estimates of incidence of HIV infection, and changes and trends in HIV and AIDS in populations at risk; 2) prevention planning to target prevention interventions, evaluate their effectiveness, and facilitate access to health, social and prevention services; and 3) allocation of local, state, and federal funds for prevention, care and treatment services, including the Ryan White Comprehensive AIDS Resources Emergency Act (RWCA).
CDC surveillance data for AIDS and HIV disease are used by the Health Resources and Services Administration (HRSA) to determine funding levels under the RWCA. Each year, CDC provides to HRSA all AIDS case counts for states and eligible metropolitan areas (EMAs) based on reports from state health departments for the previous 10, 12-month periods, as required by law. These data are not adjusted in any way and constitute crude, counts of reported cases as prescribed in the current RWCA legislation.CDC also provides HRSA with bi-annual survival weights to calculate the estimated living cases for computation of the Title I and II grant awards.HRSA uses CDC′s surveillance data to determine Title I and II allotments as well as to identify areas that qualify as EMAs and emerging communities.
History of HIV/AIDS Reporting
At the beginning of the HIV epidemic, before we even knew that HIV causes AIDS, surveillance of this public health problem could only be conducted by tracking AIDS cases and deaths. In the early 1980s when all states implemented mandatory reporting for this condition, they implemented the same system used for all other reportable conditions where the name of the affected person served as the patient identifier.
In 1985, when the first diagnostic test for HIV became available, Minnesota and Colorado were the first states to begin conducting surveillance for persons diagnosed with HIV but who were not yet sick with AIDS. These states extended their existing systems and used name-based reporting for HIV diagnosis. By the end of 1994, when CDC began to support national aggregation of surveillance data on non-AIDS HIV, 25 states collecting this information were using name-based systems. Four other states (Maryland, Texas, Connecticut, and Oregon) were using codes.
Numerous formal evaluations of name-based reporting for AIDS were conducted during the late 1980s and early 1990s. These evaluations demonstrated that this was a highly accurate and reliable method for conducting surveillance for AIDS and non-AIDS HIV. Because the vast majority of states were using name-based systems for non-AIDS HIV, the fact that name-based HIV and AIDS case surveillance had been shown to be highly accurate and reliable, and no formal evaluations of code-based systems had been conducted, CDC determined that only name-based reports would be accepted into the data collection system for the national database.
In 1995, CDC convened a meeting of states conducting non-AIDS HIV surveillance (code and name-based) to review the operational, technical, and scientific challenges associated with surveillance using coded identifiers.The states recommended that CDC evaluate additional coded identifiers and assist them in documenting and disseminating the results of their findings. With CDC collaboration and support, Texas and Maryland conducted an evaluation of their code-based systems based on reports submitted during 1994-1996. This research documented nearly 50 percent incomplete reporting and other deficiencies in the accuracy and reliability of these systems.Texas subsequently switched to name-based reporting; Maryland continued to execute and evaluate its code-based system.
The other major outcome of this 1995 meeting was a request from the states that research be done to determine whether name-based reporting discouraged HIV testing. CDC and the University of California-San Francisco did several evaluations, all of which showed no impact of reporting laws on testing behavior. The two main reasons people reported for not testing for HIV were not perceiving themselves at risk and being afraid to find out that they were positive.
In 1997, the Council of State and Territorial Epidemiologists promulgated a position statement recommending the addition of non-AIDS HIV to the national public health surveillance system. In 1999, CDC published formal guidelines for the conduct of non-AIDS HIV surveillance. These recommendations provided performance standards for evaluating HIV surveillance systems (name or code); reviewed the existing evidence for the reliability and accuracy of varying methods for reporting this condition; and based on the existing evidence at that time, “advised” that states use name-based systems. However, CDC also stated that it would continue to work with states to develop and implement standardized methods for evaluating surveillance systems using name and code-based data. Throughout all subsequent national meetings, as well as in discussions with states, CDC reiterated that it “advised” states to use name-based reporting, and the agency′s commitment to develop standardized evaluation methods.
In 2001, CDC funded 10 states (3 code-based and 7 name-based) to pilot methods for evaluating these systems. Two of the code-based states–Illinois and Washington–have subsequently switched to name-based reporting.
Also in 2001, CDC launched a national evaluation of interstate duplicate reports (i.e. multiple reports from multiple states that provide information about the same person.) This was necessary because the great success of HIV treatments meant that persons with HIV and AIDS were living longer, healthier lives, and were more likely to move across and within states. From the outset of this evaluation, it was clear that technical problems made it impossible to efficiently include code-based reports. These problems included: 1) the variety of codes used by different states conducting this type of surveillance; 2) the lack of a central, standardized, national database with code-based reports; and 3) the inability of states using codes to adequately communicate with states using names regarding potential duplicate records. Therefore, only name-based reports could be included in this interstate de-duplication effort. The results of this assessment indicated that the number of duplicate reports for non-AIDS HIV cases varied a great deal from state to state, and exceeded the proportion of duplicate case reports for AIDS cases.
Following completion of the interstate duplication study, CDC did three things: 1) identified and eliminated all identified records attributable to duplicate reporting in the national database; 2) implemented a formal system for coordinating the ongoing identification and removal of duplicate reports in the national database; 3) published and disseminated a “Dear Colleague” letter signed by the CDC Director in July 2005 stating that the agency was upgrading the guidance for states to implement name-based HIV reporting from “advising” to “recommending.” The letter also indicated that CDC would provide technical assistance to states transitioning from code to name-based systems to assure that their data could be integrated into the national HIV (non-AIDS and AIDS) data system as quickly as possible.
Additionally, the RWCA Amendments of 2000 called for an Institute of Medicine (IOM) study of states′ HIV surveillance systems and their adequacy and reliability for the purpose of using such data as the basis for CARE Act formula grant allocation.The IOM issued its report, Measuring What Matters, on allocation, planning and quality assessment for the RWCA. The IOM did not evaluate the accuracy or effectiveness of code-based systems. The IOM Committee noted in the Report that it was beyond its capacity to evaluate the HIV case-reporting system of each state and territory. The IOM Committee determined that it was ”unclear if name-based reporting is intrinsically superior to code-based reporting for eliminating duplicate reports.” This Report made clear that technical problems made it impossible to efficiently include code-based reports. The Committee did not have available the final results of the interstate duplication evaluation project when it made these recommendations.
Current Status
CDC strongly supports the requirement in the RWCA for states to implement HIV reporting by 2007. CDC′s policy is to accept HIV infection and AIDS case surveillance data only from areas conducting confidential name-based reporting because this reporting has been shown to routinely achieve high levels of accuracy and reliability. Personal identifiers are removed before data are provided to CDC. CDC provides recommended security and confidentiality policies and procedures of state and local surveillance programs that are consistent with the agency standards for the security of HIV/AIDS surveillance data.CDC also requires that recipients of federal funds for HIV/AIDS surveillance establish the minimum security standards and include their security policy in applications for surveillance funds.
HIV surveillance that is conducted using coded patient identifiers has not been shown to routinely produce equally accurate, timely, or complete data compared to that conducted using confidential, name-based surveillance methods. Currently, only confidential, name-based HIV reporting, integrated with AIDS surveillance data, can be used by states to identify and remove cases that are counted in more than one state before they are reported to CDC′s national surveillance database.
States that have implemented code-based systems consistently inform CDC that these systems are more complex, expensive and burdensome than name-based reporting systems. Since states have extensive experience with name-based systems for persons with HIV who have progressed to AIDS, CDC has accepted that these assertions are valid. However, few formal economic evaluations have been conducted. CDC is only aware of one such systematic quantitative evaluation comparing the relative costs of name-based systems to systems using codes and name-to-code. This evaluation found that a name-to-code reporting system was 15 percent more expensive than name-based reporting, and reporting based exclusively on codes was 50 percent more expensive than name-based reporting.
CDC is providing technical assistance to states transitioning from code- to name-based systems to assure that their data can be integrated into the national HIV (non-AIDS and AIDS) data system as quickly as possible. CDC continues to provide assistance to the seven states that have made the transition to name-based systems since the IOM report was published in 2004.As previously noted, as of April 2006, 43 states have adopted use of name-based systems of HIV reporting.
CDC continues to provide funding and technical assistance to states that use code-based methods for identifying patients in their HIV surveillance system. CDC is implementing and disseminating methods for conducting evaluations of the accuracy and reliability of reporting systems within states, regardless of reporting method. CDC is deploying data management software that integrates functions that will allow areas to use standardized methods to evaluate their systems based on recently completed pilot studies. In addition, CDC regularly offers technical assistance to areas using code-based systems that have not received this software. This assistance includes the software, and relevant documentation, that was used in the pilots.
Closing
In summary, CDC is responsible for ensuring the integrity of the national HIV/AIDS surveillance system to accurately monitor the epidemic in the United States. CDC continues to work closely with all states to help them adopt and implement high-quality HIV surveillance systems. Having all states collect HIV information in the same manner will ensure that the nation has reliable and valid data to monitor the scope of the epidemic; plan for and evaluate prevention, care, and treatment programs; and focus those programs on persons most at risk. Thank you again for this opportunity. I will be pleased to answer any questions.
Figure 1. Current Status of HIV Infection Surveillance, April 2006.