Improving Access to Children’s Mental Health Care
Learn how CDC works to identify policies and practices that connect more families to mental health care
- Improving strategies to connect families to mental health care
- Addressing gaps in the workforce
- Investigating how funding issues affect mental health care
- Understanding how social determinants of health affect mental health care
- Identifying children who need more support
- Addressing concerns early and supporting well-being of families
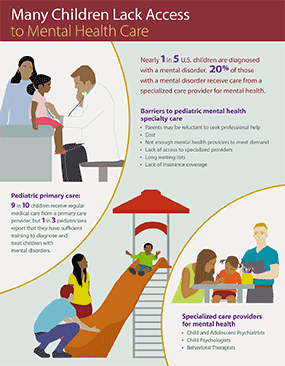
Access to mental health care is important when children have difficulty with emotions or behavior. It can be challenging for some families to get mental health care for their children. Nearly 1 in 5 children have a mental, emotional, or behavioral disorder1, such as anxiety or depression, attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), disruptive behavior disorder, or Tourette syndrome. Children with these disorders benefit from early diagnosis and treatment.
Unfortunately, only about 20% of children with mental, emotional, or behavioral disorders receive care from a specialized mental health care provider2. In addition, many children with other types of developmental and learning disorders may also have difficulty with emotions or behavior and need treatment.
Some families cannot find mental health care because of the lack of providers in their area. Some families may have to travel long distances or be placed on long waiting lists to receive care. High costs, lack of insurance coverage, and the time and effort involved make it harder for parents to get mental health care for their child.
What CDC is doing to improve access to mental health care for children
CDC is committed to helping children and families get the mental health care they need. There are many ways to improve access to mental health care, and CDC has many activities around improving lifelong mental health. This page provides an overview of examples, but is not a complete description of CDC’s work on children’s mental health. Some of the ways CDC is working to improve access to mental health care for children include the following:
- Improving strategies to connect families to mental health care
- Understanding gaps in the mental health workforce serving children
- Investigating how funding policies affect mental health care
- Understanding social determinants of health that make it harder for some families to get access to mental health care
Improving strategies to connect families to mental health care
One of the barriers to obtaining mental health care that families face is not being able to connect to mental health care providers. Policies that address this barrier may be one way to improve access.
- Behavioral Health Integration (BHI) is one approach that can improve access to mental health services for children and their families. A CDC-sponsored report on BHI published by the Milbank Memorial Fund showed that partnerships between primary medical care practices and mental health care specialists can make mental health services more accessible for some families.
- CDC conducted a systematic review of policy levers affecting children’s mental health care access that showed that policies that allow mental health care to be located in primary medical care and in schools can help improve access.
- CDC developed a policy report that presents promising practices for delivering mental health care in rural areas, including telemedicine, school-based health centers, and integrating behavioral health in primary care.
- CDC sponsored a report on Integrated Family Care that examined five service providers’ successes and challenges with implementing the Integrated Family Care model by expanding care focused on the child alone to meet the emerging physical health, mental health, and social service needs of families with young children.
- CDC reviewed the research evidence to understand how couple‐ and family‐based psychosocial interventions can be used to promote infant and early childhood mental health.
- CDC supported a telemental health workshop by The National Academies of Sciences, Engineering, and Medicine to discuss how telemental health services could be a critical tool for improving mental health care access for children during and after the pandemic, and to examine limitations.
Addressing gaps in the workforce
- CDC funds the National Resource Center on ADHD and the Tourette Association of America to increase the capacity of healthcare providers and educators to support the health, mental health, and education of children with ADHD and/or Tourette syndrome and associated conditions, and help individuals find the best health services and educational supports to improve their health and well-being.
- CDC is partnering with the American Academy of Pediatrics (AAP) to create educational modules for pediatricians and other health care providers. These modules will be available for free as an AAP PediaLink. This education will provide training on best practices in health care for children and adolescents with specific disorders like Tourette syndrome and fragile X syndrome.
- CDC and partner organizations examined whether U.S. emergency departments (EDs) have policies in place to care for children with mental health and social concerns and found that less than half of EDs had such a policy, identifying gaps that could improve access if filled.
- Using data on behavioral health service providers from around the nation, CDC created state maps showing the availability of providers who can assess, refer, or treat children’s mental health concerns in 2015. View state maps showing the number of U.S. behavioral health providers per 10,000 children by county in 2015.
- CDC is currently characterizing differences in the rules that states have about licensure and credentialing for child mental health service providers (social workers, marriage and family therapists, and licensed professional counselors) to identify laws and policies that could affect the mental health workforce.
Investigating how funding issues affect mental health care
- Children’s mental health is connected to family care; for example, many evidence-based treatments for young children with behavior problems, ADHD, or anxiety include parent training. A CDC-sponsored report describes opportunities for healthcare providers and insurers to use primary care as a launching pad toward Integrated Family Care.
- A CDC-sponsored report describes how child health champions and state Medicaid programs can collaborate to reward quality and outcomes of child health care rather than quantity of care delivered.
- The systematic review of policy levers that affect mental health access found that insurance-based policies such as making mental health equal to physical health and providing public insurance to those who need it can help improve access.
Understanding how social determinants of health affect mental health care
Social determinants of health are conditions in the places where children live, learn, and play that affect a wide range of health and developmental outcomes.
- Mental health is impacted by poverty.
- CDC funded a review of the evidence of the health benefits of the Earned Income Tax Credit (EITC) found that children in families receiving the EITC showed fewer behavioral health problems, including anxiety and depression.
- CDC funded a report on supplemental security income (SSI) policies that points to ways that State Supplementary Payment (SSP) program benefits can be used as a tool to reduce childhood poverty and better support children with disabilities.
- CDC funded a fact sheet that explains how policymakers and other partners can navigate SSI asset limit requirements to expand the number of children with disabilities who can access this benefit.
- Geographic location, such as living in rural areas, can affect access to mental health care.
- CDC published a report on factors that affect childhood mental, behavioral, and developmental disorders in rural communities. A New England Journal of Medicine commentary highlighted the report and presented solutions that address differences in access to mental health treatment for children living in rural areas compared with urban areas.
- CDC developed a mental health services for children policy report that presents promising practices for delivering mental health care in rural areas.
- Racism and other adverse childhood experiences can impact children’s mental health.
- CDC is working on research to better understand the impact of racism and other adverse childhood experiences on mental health, to find ways to improve prevention and intervention.
- CDC is investigating the effects of adverse childhood experiences on risk and protective factors including access to medical care and mental health services.
Identifying children who need more support
- CDC and other federal partners collect data to understand children’s mental health and to identify how many children are diagnosed with different disorders. A comprehensive children’s mental health report using data from 9 different sources to describe mental health, mental disorders, and mental health treatment in children during 2013–2019 showed that poor mental health among children continues to be a substantial public health concern. CDC funded the development of an Opening Playbook for state, tribal, and local health departments that shows ways to use available data to improve child and adolescent mental health. The playbook shows how three indicators that schools generally have available or can make available, specifically attendance, disciplinary actions, and school readiness, can be used to begin assessing children’s mental health at the population level.
Addressing concerns early and supporting well-being of families
In addition to increasing access to mental health care for children, CDC works to improve healthy child development, and to increase emotional, psychological, and social well-being. Mental health is also an aspect of the Whole School, Whole Community, Whole Child (WSCC) approach. CDC supports adolescent and school mental health efforts such as the following:
- Social and Emotional Climate and Learning | Healthy Schools | CDC
- Sleep and Health | Healthy Schools | CDC
- School Connectedness | Adolescent and School Health | CDC
- Adolescent Connectedness | Adolescent and School Health | CDC
- Mental and Emotional Health Module for PreK–12 | Adolescent and School Health | CDC

CDC also provides families with tools that help them identify concerns about children’s emotions and behavior early and learn strategies to support their children.
- CDC and partners funded the National Academies of Sciences, Engineering, and Medicine Forum for Children’s Well-Being to inform a forward-looking agenda for building a stronger research and practice base around the development and implementation of programs, practices, and policies to promote all children’s mental, emotional, and behavioral health and prevent mental disorders.
- CDC funded the National Academies of Sciences, Engineering, and Medicine to develop a suite of microlearning, graphic novel style tools based on cognitive behavioral therapy techniques—available in both English and Spanish—to promote coping and resilience and help children and youth manage feelings of stress, anxiety, and sadness.
- CDC developed the Milestone Tracker App to help parents track their child’s developmental milestones from age 2 months to 5 years, get tips from CDC for encouraging their child’s development, and find out what to do if they are ever concerned about how their child is developing.
- CDC funded the Association of University Centers on Disabilities to pilot 12 Children’s Mental Health Champions (CMHC) in 10 states and 1 territory. The Champions work to implement effective strategies for mental health promotion, prevention supports, and the creation of networks (e.g., school, health care, and community) to promote better connections between these systems.
Resources
Journal Articles
- Characteristics Associated with Presence of Pediatric Mental Health Care Policies in Emergency Departments
- Differences in Health Care, Family, and Community Factors Associated with Mental, Behavioral, and Developmental Disorders Among Children Aged 2–8 Years in Rural and Urban Areas—United States, 2011–2012
- Evidence base Review of Couple‐ and Family‐based Psychosocial Interventions to Promote Infant and Early Childhood Mental Health, 2010–2019
- Trends Over Time and Jurisdiction Variability in Supplemental Security Income and State Supplementary Payment Programs for Children with Disabilities
- Policy Levers to Promote Access to and Utilization of Children’s Mental Health Services: A Systematic Review
Reports
- Achieving Payment Reform for Children Through Medicaid and Stakeholder Collaboration
- Behavioral Health Integration in Pediatric Primary Care
- Considerations for Using Telemental Health Services for Children and Youth
- Expanding SSI Access: Understanding Asset Limits for Children with Disabilities
- Profiles in Integrated Family Care
- Plan and Provider Opportunities to Move Toward Integrated Family Health Care
- Using Data to Improve Child and Adolescent Mental Health (CAMH): The Opening Playbook
Other Resources
- Forum for Children’s Well-Being Promoting Cognitive, Affective, and Behavioral Health for Children and Youth
- Earned Income Tax Credit (EITC): One of the most effective public health interventions you’ve never heard of
- Mental Health Services for Children Policy Brief: Providing Access to Mental Health Services for Children in Rural Areas
More Information
- Children’s Mental Health | CDC
- Child Development | CDC
- “Learn the Signs. Act Early.” | CDC
- Attention-Deficit / Hyperactivity Disorder (ADHD) | CDC
- Tourette Syndrome | CDC
- Autism Spectrum Disorder (ASD) | CDC
References
- National Research Council and Institute of Medicine. (2009). Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. O’Connell, T. Boat, & K. E. Warner Eds. Washington, DC. The National Academic Press.
- Martini R, Hilt R, Marx L, et al.; for the American Academy of Child and Adolescent Psychiatry. Best principles for integration of child psychiatry into the pediatric health home. pdf icon[217 KB, 13 pages]