Recommendations for Fully Vaccinated People
COVID-19 Homepage

Location, location, location
Interpretive Summary for July 16, 2021
Location, location, location
The conditions in which people live, learn, work, and play can affect a wide range of health risks and outcomes. Differences in the prevalence of many risks and outcomes differ by metropolitan and non-metropolitan* areas. Long-standing systemic health and social inequities have put some rural residents at increased risk of getting or having severe illness from COVID-19. The COVID-19 cumulative death rate in non-metropolitan areas has exceeded that of metropolitan areas since December 2020.
Approximately 1 in 5 people in the United States live in rural communities. Rural areas can face different health challenges depending on where they are located. Many are considered highly vulnerable according to CDC’s Social Vulnerability Index (SVI), which includes factors such as housing, transportation, socioeconomic status, race, and ethnicity. Additionally, rural communities often have a higher proportion of residents who lack health insurance, live with a chronic disease or disability, are older than 65 years, and have limited access to health care facilities with intensive care capabilities. These factors place residents of rural communities at increased risk for COVID-19-associated illness and death.
Because of this increased risk, vaccination disparities between urban and rural areas could further undermine efforts to reduce morbidity and mortality from COVID-19 nationally. A recent CDC report found that COVID-19 vaccination coverage was lower in rural counties compared to urban counties. Efforts are underway to raise awareness about COVID-19 vaccines, and to make vaccines more accessible to residents of rural communities. We must work together to ensure that all people, regardless of geographic location, have resources to maintain and manage their physical and mental health, including easy access to accurate information and affordable medical care so all communities can thrive.
* Metropolitan vs. Non-Metropolitan classification type groups 6 National Center for Health Statistics (NCHS) Urban-Rural classifications, where “Metro” counties include Large Central Metro, Large Fringe Metro, Medium Metro, and Small Metro and “Non-Metro” counties include Micropolitan and Non-Core (Rural). Urban/rural classification type is based on the 2013 National Center for Health Statistics Urban-Rural Classification Scheme for Counties.
Note to readers: To find a vaccine provider near you, visit Vaccines.gov or your state or local public health department website. You can also text your zip code to 438829 to get 3 locations near you with vaccines in stock. If you prefer your information in Spanish, text your zip code to 822862. You can also call the National COVID-19 Vaccination Assistance Hotline at 1-800-232-0233 to get help in English, Spanish, and more than 150 other languages. It also has a TTY line to support access by hearing impaired callers. If you or someone you know is hesitant about COVID-19 vaccination, CDC has information and answers to frequently asked questions to help inform the decision.
Reported Cases
The current 7-day moving average of daily new cases (26,306) increased 69.3% compared with the previous 7-day moving average (15,541). The current 7-day moving average is 89.6% lower than the peak observed on January 10, 2021 (251,880) and is 129.3% higher than the lowest value observed on June 20, 2021 (11,472). A total of 33,797,400 COVID-19 cases have been reported as of July 14.
33,797,400
Total Cases Reported
33,797,400
Total Cases Reported
26,306
Current 7-Day Average*
26,306
Current 7-Day Average*
15,541
Prior 7-Day Average
15,541
Prior 7-Day Average
+69.3%
Change in 7-Day Average since Prior Week
+69.3%
Change in 7-Day Average since Prior Week
*Historical cases are excluded from daily new cases and 7-day average calculations until they are incorporated into the dataset for the applicable date. Of 73,766 historical cases reported retroactively, 1,474 were reported in the current week and 697 were reported in the prior week.
Daily Trends in COVID-19 Cases in the United States Reported to CDC

7-Day moving average
SARS-CoV-2 Variants
Multiple variants of the virus that causes COVID-19 are circulating globally, including within the United States. To date, four variants have been classified as a variant of concern (VOC). Nowcast estimates* of SARS-CoV-2 cases caused by these VOCs for the two weeks ending July 3 are summarized here. Nationally, the proportion of cases attributed to B.1.617.2 (Delta) is predicted to increase to 57.6%, becoming the predominant lineage in the United States; B.1.1.7 (Alpha) proportion is predicted to decrease to 24.9%; P.1 (Gamma) proportion is predicted to decrease to 7.7%; and B.1.351 (Beta) is predicted to decrease slightly to 0.1%. Nowcast estimates predict that B.1.617.2 (Delta) will be the predominant lineage circulating in all HHS regions and be more than 75% in regions 7 and 8. B.1.1.7 (Alpha) is predicted to be less than 40% in all HHS regions. P.1 (Gamma) is predicted to be more than 10% in regions 1, 5, and 10; and B.1.351 (Beta) is predicted to be less than or equal to 0.5% in all HHS regions.
*The median time from specimen collection to sequence data reporting is about 3 weeks. As a result, weighted estimates for the most recent few weeks may be unstable or unavailable. CDC’s Nowcast is a data projection tool that helps fill this gap by generating timely estimates of variant proportions for variants that are circulating in the United States. View Nowcast estimates on CDC’s COVID Data Tracker website on the Variant Proportions page.
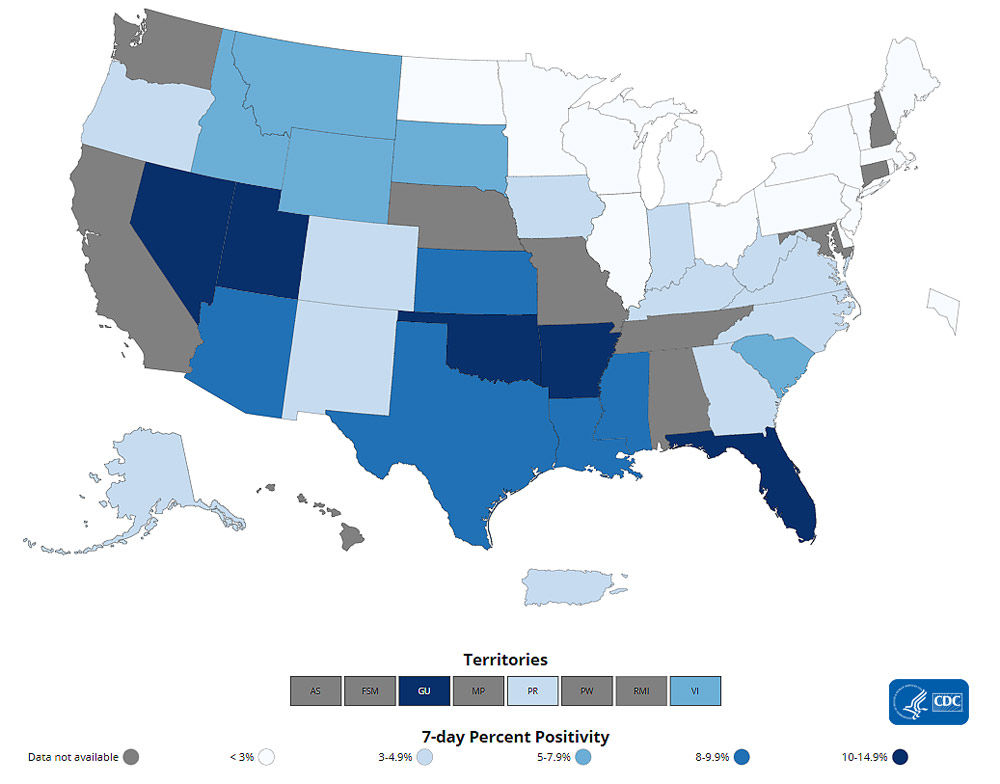
Testing
The percentage of COVID-19 NAATs (nucleic acid amplification tests) that are positive (percent positivity) has increased from the previous week. The 7-day average of percent positivity from tests is now 4.0%. The 7-day average number of tests reported for July 02 – July 08 was 507,379 down 11.0% from 569,778 for the prior 7 days.
476,020,464
Total Tests Reported
476,020,464
Total Tests Reported
507,379
7-Day Average Tests Reported
507,379
7-Day Average Tests Reported
4.0%
7-Day Average % Positivity
4.0%
7-Day Average % Positivity
2.8%
Previous 7-Day Average % Positivity
2.8%
Previous 7-Day Average % Positivity
+40.7%
Change in 7-Day Average % Positivity since Prior Week
+40.7%
Change in 7-Day Average % Positivity since Prior Week
COVID-19 NAAT Laboratory Test 7-day Percent Positivity by State/Territory
Vaccinations
The U.S. COVID-19 Vaccination Program began December 14, 2020. As of July 15, 336.1 million vaccine doses have been administered. Overall, about 185.1 million people, or 55.8% of the total U.S. population, have received at least one dose of vaccine. About 160.4 million people, or 48.3% of the total U.S. population, have been fully vaccinated.* As of July 15, the 7-day average number of administered vaccine doses reported (by date administered) to CDC per day was 270,592, a 35.7% decrease from the previous week.
The COVID Data Tracker Vaccination Demographic Trends tab shows vaccination trends by age group. As of July 15, 88.9% of people ages 65 or older have received at least one dose of vaccine and 79.3% are fully vaccinated. Just over two-thirds (67.9%) of people ages 18 or older have received at least one dose of vaccine and 59.2% are fully vaccinated. For people ages 12 or older, 65.2% have received at least one dose of vaccine and 56.5% are fully vaccinated.
336,054,953
Vaccines Administered
336,054,953
Vaccines Administered
185,135,757
People who received at least one dose
185,135,757
People who received at least one dose
160,408,538
People who are fully vaccinated*
160,408,538
People who are fully vaccinated*
55.8%
Percentage of the US population that has received at least one dose
55.8%
Percentage of the US population that has received at least one dose
48.3%
Percentage of the US population that has been fully vaccinated*
48.3%
Percentage of the US population that has been fully vaccinated*
+0.6
Percentage point increase from last week
+0.6
Percentage point increase from last week
+0.6
Percentage point increase from last week
+0.6
Percentage point increase from last week
*People are considered fully vaccinated 2 weeks after their second dose in a 2-dose series (such as the Pfizer or Moderna vaccines), or 2 weeks after a single-dose vaccine (such as Johnson & Johnson’s Janssen vaccine).
Daily Change in Number of COVID-19 Vaccinations in the United States Reported to CDC

7-Day moving average
Hospitalizations
New Hospital Admissions
The current 7-day average for July 7–July 13 was 2,794. This is a 35.8% increase from the prior 7-day average (2,058) from June 30–July 6. The 7-day moving average for new admissions has consistently increased since June 25, 2021.
2,317,457
Total New Admissions
2,317,457
Total New Admissions
2,794
Current 7-Day Average
2,794
Current 7-Day Average
2,058
Prior 7-Day Average
2,058
Prior 7-Day Average
+35.8%
Change in 7-Day Average
+35.8%
Change in 7-Day Average
The start of consistent reporting of hospital admissions data was August 1, 2020.
Daily Trends in Number of New COVID-19 Hospital Admissions in the United States
New admissions are pulled from a 10 am EST snapshot of the HHS Unified Hospital Timeseries Dataset. Due to potential reporting delays, data from the most recent 7 days, as noted in the figure above with the grey bar, should be interpreted with caution. Small shifts in historic data may also occur due to changes in the CMS Provider of Services file, which is used to identify the cohort of included hospitals.
Cumulative Trends in Hospitalizations in People in Racial and Ethnic Minority Groups
CDC’s Coronavirus Disease 2019-Associated Hospitalization Surveillance Network (COVID-NET) shows that since the start of the COVID-19 pandemic, people from racial and ethnic minority groups have been at increased risk for COVID-19-associated hospitalizations compared to non-Hispanic White people. The cumulative hospitalization rates* for many groups demonstrate how much some communities were disproportionately impacted by the pandemic. For the week ending July 3, 2021, the cumulative rate of hospitalizations was 1129.8 per 100,000 population for American Indian/Alaska Native people, 880.4 per 100,000 population for non-Hispanic Black people, and 733.0 per 100,000 population for Hispanic people. In comparison, the cumulative rate of COVID-19-associated hospitalizations in non-Hispanic White people is 422.1 per 100,000 population.
*While these rates are not adjusted for differences in age, additional data on age-adjusted rates by race/ethnicity for COVID-19-associated hospitalizations can be found here.
Trends in Hospitalizations in People in Racial and Ethnic Minority Groups
The Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET) is an additional source for hospitalization data collected through a network of more than 250 acute-care hospitals in 14 states (representing ~10% of the U.S. population). Detailed data on patient demographics, including race/ethnicity, underlying medical conditions, medical interventions, and clinical outcomes, are standardized case reporting form.
Deaths
The current 7-day moving average of new deaths (211) has increased 26.3% compared with the previous 7-day moving average (167). As of July 14, a total of 605,905 COVID-19 deaths have been reported.
605,905
Total Deaths Reported
605,905
Total Deaths Reported
211
Current 7-Day Average*
211
Current 7-Day Average*
167
Prior 7-Day Average
167
Prior 7-Day Average
+26.3%
Change in 7-Day Average Since Prior Week
+26.3%
Change in 7-Day Average Since Prior Week
*Historical deaths are excluded from the daily new deaths and 7-day average calculations until they are incorporated into the dataset by their applicable date. Of 6,110 historical deaths reported retroactively, 9 were reported in the current week and 1 was reported in the prior week.
Daily Trends in Number of COVID-19 Deaths in the United States Reported to CDC

7-Day moving average
Recent COVID Data Tracker Updates
- A new Vaccination Equity tab displays a combined county-level view of vaccine coverage and Social Vulnerability Index (SVI) rating to visualize how each county’s vaccine coverage and estimated vulnerability level intersect
- Static bivariate maps that illustrate cases by vaccination coverage were added to the COVID Data Tracker Communications Toolkit