Recommendations for Fully Vaccinated People
COVID-19 Homepage
Update on COVID-19–Related Deaths
Interpretive Summary for November 18, 2022
Update on COVID-19–Related Deaths
Deaths from COVID-19 have substantially decreased in the United States in recent months. This is likely due to high levels of population immunity, either through vaccination or prior infection, as well as improvements in early treatment for patients at risk for severe disease.
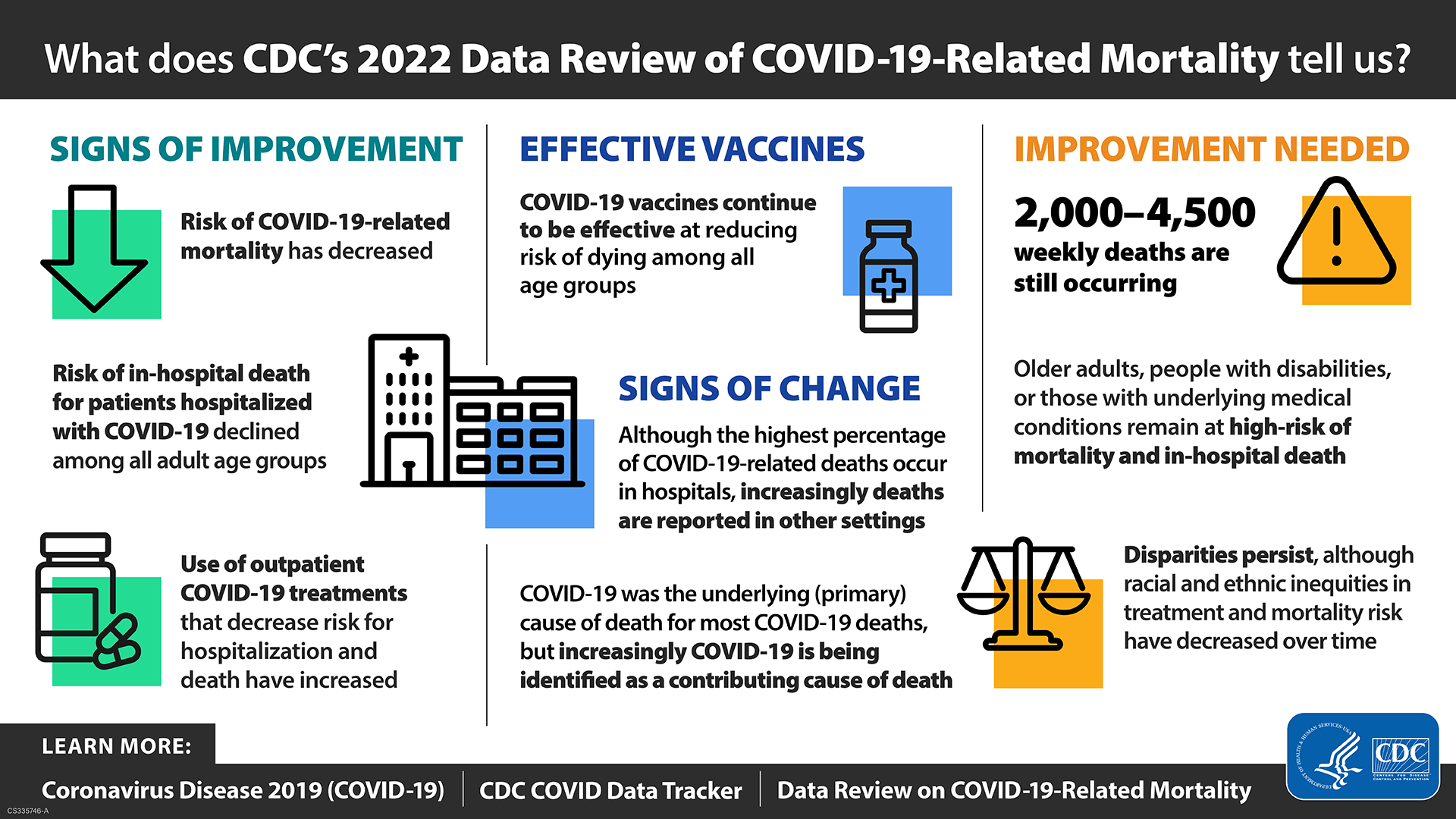
On November 16, 2022, CDC released a new COVID-19 Data Review: Update on COVID-19–Related Mortality that examines recent and overall trends in COVID-19–related mortality among adults in the United States. Currently, the virus poses the highest risk of COVID-19–related death for older adults (especially those older than age 85 years), people who have underlying medical conditions, people with disabilities, and people who are not up to date with COVID-19 vaccinations.
CDC continues to monitor changes in the virus to inform individual and community-level actions. We now have many tools to protect ourselves and those around us who remain at higher risk for severe illness.
- COVID-19 vaccines and treatments remain the best lines of defense against severe illness, hospitalization, and death.
- Stay up to date on your COVID-19 vaccinations. People of any age who are vaccinated have a lower risk of dying, with the most protection observed among people who have received boosters or additional doses. Use CDC’s booster tool to find out if and when to get your COVID-19 updated (bivalent) booster. Find a vaccine location in your community.
- If you are immunocompromised, talk with your healthcare provider about Evusheld, a preventive medication that is given before you get exposed or test positive.*
- If you test positive for COVID-19 and are more likely to get very sick, other treatments (such as Paxlovid) can reduce your chances of hospitalization and death.*
- People can also protect themselves and others by wearing a mask or respirator, getting tested if needed, staying home if experiencing COVID-19 symptoms, improving ventilation when indoors, and using other layered prevention measures. COVID-19 Community Levels can help you make an informed decision about how to protect yourself and others.
Every life lost to COVID-19 is a tragedy and should be a reminder to continue taking precautions to prevent further serious illness and death. As the virus continues to spread and change over time, everyone should continue to take steps to protect themselves and others.
See the A Closer Look section for more detailed information from the COVID-19 Data Review: Update on COVID-19–Related Mortality.
*Medications to treat COVID-19 must be prescribed by a healthcare provider and started as soon as possible after diagnosis to be effective. Contact a healthcare provider right away to determine if you are eligible for treatment, even if your symptoms are mild. Visit the Treatment LocatorExternal to find a location that offers testing and treatment or a pharmacy where you can fill your prescription.
Note to Readers: CDC will not publish the COVID Data Tracker Weekly Review on Friday, November 25, 2022, due to the Thanksgiving holiday. Publication will resume on Friday, December 2, 2022.
- COVID Data Tracker’s Vaccine Confidence tab was updated to include new national survey indicators on updated (bivalent) booster uptake and intent to receive bivalent booster among children and teens ages 5–17 years.
- COVID Data Tracker’s Vaccine Trends tab was updated to display a new metric that displays a daily count of people receiving an updated (bivalent) booster dose by date of vaccine administration.
- COVID-19–Associated Hospitalizations Among U.S. Infants Aged <6 Months — COVID-NET, 13 States, June 2021–August 2022
- Perception of Local COVID-19 Transmission and Use of Preventive Behaviors Among Adults with Recent SARS-CoV-2 Infection — Illinois and Michigan, June 1–July 31, 2022
- Sociodemographic Variation in Early Uptake of COVID-19 Vaccine and Parental Intent and Attitudes Toward Vaccination of Children Aged 6 Months–4 Years — United States, July 1–29, 2022
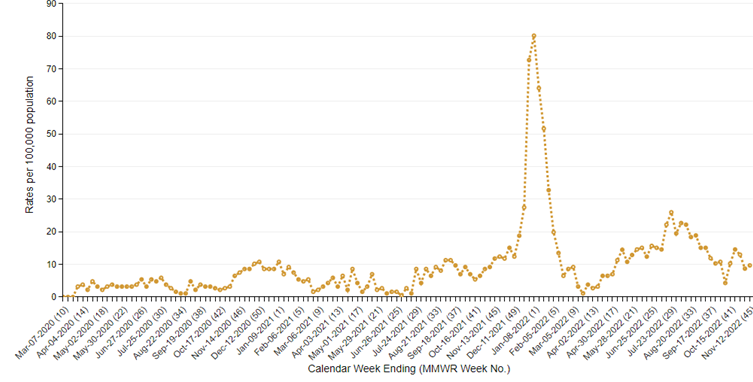
COVID-19 Community Levels*
As of November 17, 2022, there are 90 (2.8%) counties, districts, or territories with a high COVID-19 Community Level, 537 (16.7%) counties with a medium Community Level, and 2,590 (80.4%) counties with a low Community Level. Compared with last week, this represents a minor increase (+0.2 percentage points) in the number of high-level counties, a minor decrease (-4.3 percentage points) in the number of medium-level counties, and a minor increase (+4.1 percentage points) in the number of low-level counties. Overall, 43 out of 52 jurisdictions** had high- or medium-level counties this week. Delaware, District of Columbia, Georgia, Hawaii, Massachusetts, Mississippi, New Hampshire, Rhode Island, and South Carolina are the only jurisdictions to have all counties at low Community Levels.
To check your COVID-19 Community Level, visit COVID Data Tracker. To learn which prevention measures are recommended based on your COVID-19 Community Level, visit COVID-19 Community Level and COVID-19 Prevention.
*CDC recommends use of COVID-19 Community Levels to determine the impact of COVID-19 on communities and to take action. CDC also provides Community Transmission Levels to describe the amount of COVID-19 spread within each county. Healthcare facilities use Community Transmission Levels to determine infection control interventions.
**Includes the 50 states, the District of Columbia, and Puerto Rico.
Reported Cases
As of November 16, 2022, the current 7-day average of weekly new cases (40,102) decreased 3.2% compared with the previous 7-day average (41,412). A total of 98,174,364 COVID-19 cases have been reported in the United States as of November 16, 2022.
Variant Proportions
CDC Nowcast projections* for the week ending November 19, 2022, estimate the proportion of ten lineages designated as Omicron with estimates above 1%: BA.5—and five of its sublineages (BQ.1, BQ.1.1, BF.7, BA.5.2.6, and BF.11)—BA.4.6, BA.2, and BA.2.75.
The predominant Omicron lineage is BQ.1, projected to be 25.5% (95% PI 22.1-29.1%). Additionally, other variants represent 3.1% of circulating viruses, largely composed of the Omicron-derived XBB lineage.
See COVID Data Tracker for the proportions of all relevant lineages currently circulating.
98,174,364
Total Cases Reported
40,102
Current 7-Day Average**
41,412
Previous 7-Day Average
-3.2%
Change in 7-Day Average since Previous Period
*CDC uses Nowcast projections to predict current variant proportions circulating in the United States. The median time from specimen collection to sequence data reporting is about 3 weeks. As a result, weighted estimates for the most recent few weeks may be unstable or unavailable. View Nowcast estimates on CDC’s COVID Data Tracker website on the Variant Proportions page.
**Historical cases are excluded from weekly new cases and 7-day average calculations until they are incorporated into the dataset for the applicable date. No historical cases reported at this time.
Vaccinations
COVID-19 Vaccine Primary Series
As of November 16, 2022, 650.8 million vaccine doses have been administered in the United States. Overall, about 267.5 million people, or 80.6% of the total U.S. population, have received at least one dose of vaccine. About 228.2 million people, or 68.7% of the total U.S. population, have completed a primary series.*
650,810,290
Vaccine Doses Administered
267,476,279
People who received at least one dose (80.6% of the U.S. population)
228,154,832
People who have completed a primary series* (68.7% of the U.S. population)
+0.2
Percentage point change from last week
+0.1%
Percentage point change from last week
*Represents the number of people who have received the second dose in a two-dose COVID-19 vaccine series (such as the Pfizer-BioNTech, Moderna, or Novavax vaccines) or one dose of the single-shot Johnson & Johnson’s Janssen vaccine.
COVID-19 Vaccine Boosters
Of those who have completed a primary series, about 113.9 million people have received a booster dose,* and more than 35.4 million people have received an updated (bivalent) booster dose. But 48.7% of the total booster-eligible population has not yet received a booster dose. Booster dose eligibility varies by age and health condition. Learn more about who is eligible.
152,791,406
Booster Doses Administered
113,844,972
Population ≥ 5 Years of Age with a 1st booster dose*
31,178,010
Population ≥ 50 Years of Age with a 2nd booster dose**
50.1%
Percentage of the Population ≥ 5 Years of Age with a 1st booster dose
46.3%
Percentage of the Population ≥ 50 Years of Age with a 2nd booster dose
+0.2
Percentage point change from last week
+1.3
Percentage point change from last week
*Represents the number of people who have completed a primary series and have received another dose of COVID-19 vaccine since August 13, 2021. This includes people who received their first additional dose or booster dose.
**Represents the number of people who have completed a primary series and have received two subsequent doses of COVID-19 vaccine since August 13, 2021. This includes people who received two booster doses and people who received one additional dose and one booster dose.
5,516,552
Total New Admissions
3,444
Current 7-Day Average
3,460
Prior 7-Day Average
-4.4%
Change in 7-Day Average
The start of consistent reporting of hospital admissions data was August 1, 2020.
Daily Trends in Number of New COVID-19 Hospital Admissions in the United States
New admissions are pulled from a 10 am EDT snapshot of the HHS Unified Hospital Data – Analytic Dataset. Due to potential reporting delays, data from the most recent 7 days, as noted in the figure above with the grey bar, should be interpreted with caution. Small shifts in historic data may also occur due to changes in the Centers for Medicare & Medicaid Services (CMS) Provider of Services file, which is used to identify the cohort of included hospitals.
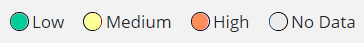
COVID-NET: Trends in Hospitalization Rates among Infant Ages 6 months and Younger
CDC’s Coronavirus Disease 2019-Associated Hospitalization Surveillance Network (COVID-NET) shows that for the week ending October 29, the rate of COVID-19-associated hospitalizations for infants ages 6 months and younger, who are not eligible for vaccination, is 13 per 100,000 population—the highest among all pediatric age groups. The rate had, in general, declined from July through September, but in October it began to increase.
This new report using COVID-NET data contains additional information on COVID-19-associated hospitalizations among infants ages 6 months and younger.
Weekly Rates of COVID-19-Associated Hospitalizations among Infants Ages 6 Months and Younger
The Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET) is an additional source for hospitalization data collected through a network of more than 250 acute-care hospitals in 14 states (representing ~10% of the U.S. population). Detailed data on patient demographics, including race/ethnicity, underlying medical conditions, medical interventions, and clinical outcomes, are collected using a standardized case reporting form.
Deaths
The current 7-day average of new deaths (317) decreased 5.3% compared with the previous 7-day average (335). As of November 16, 2022, a total of 1,073,115 COVID-19 deaths have been reported in the United States.
1,073,115
Total Deaths Reported
317
Current 7-Day Average*
335
Prior 7-Day Average
-5.3%
Change in 7-Day Average Since Prior Period
*Historical deaths are excluded from the weekly new deaths and 7-day average calculations until they are incorporated into the dataset by their applicable date. Of 1,037 historical deaths reported retroactively, none were was reported in the current week and 5 were reported in the prior week.
Testing
The percentage of COVID-19 NAATs (nucleic acid amplification tests)* that are positive is increasing in comparison to the previous week. The 7-day average of percent positivity from NAATs is now 8.3%. The 7-day average number of tests reported for November 4–10, 2022, was 359,953, down 10.0% from 400,073 for the prior 7 days.
982,269,493
Total Tests Reported
359,953
7-Day Average Tests Reported
8.3%
7-Day Average % Positivity
8.2%
Previous 7-Day Average % Positivity
+0.11
Percentage point change in 7-Day Average % Positivity since Prior Week
*Test for SARS-CoV-2, the virus that causes COVID-19
Wastewater Surveillance
COVID Data Tracker’s Wastewater Surveillance tab tracks levels, changes, and detections of SARS-CoV-2* viral RNA in wastewater at over 1,200 testing sites across the country.
Currently, about 48% of the country is reporting moderate to high SARS-CoV-2 levels in wastewater. About 17% of sites reporting wastewater data are currently seeing some of the highest levels for those sites since December 1, 2021. About 44% of sites are experiencing a decrease in SARS-CoV-2 levels, and about 50% are reporting an increase.
For more information on how to use wastewater data, visit CDC’s wastewater surveillance website.
*The virus that causes COVID-19
SARS-CoV-2 Levels in Wastewater by Site
0% denotes that levels are the lowest they have been at the site; 100% denotes that levels are the highest they have been at the site.
The A Closer Look section presents more detailed information for readers who want to learn more about current issues of interest.
COVID-19 Data Review: Update on COVID-19–Related Mortality
As of November 16, 2022, a total of 1,073,115 deaths due to COVID-19 have been reported in the United States.
Each year during 2020–2022, COVID-19 has been identified as the third leading cause of death among U.S. adults, trailing only heart disease and cancer. On November 16, 2022, CDC released a new COVID-19 Data Review: Update on COVID-19–Related Mortality that examines recent and overall trends in COVID-19–related mortality among adults in the United States. Data presented in this report point to a rapid reduction in COVID-19–related mortality in the U.S. population in March 2022, with sustained lower levels from April through early November 2022.
Throughout the pandemic, CDC has provided information on COVID-19–related mortality, including data on COVID Data Tracker and in scientific publications. This report builds on previous work and contains preliminary results, as well as pertinent data from previously published analyses, that can improve understanding of COVID-19–related deaths, drive public health action, and inform further scientific inquiry.
The report examines six questions. The first page, which includes a summary, report limitations, and top takeaway messages, can be downloaded as a PDF. The full report includes data visualizations and full descriptions of the data sources and findings. Key findings from the report are briefly presented here.
Top Takeaway Messages
- There were signs of improvement in COVID-19–related mortality in the United States.
- Vaccines continue to be effective in reducing COVID-19-related mortality.
- Where and how COVID-19–related deaths occur appeared to be changing.
- Improvement is needed to decrease the risk for COVID-19-related mortality.
Questions
- 1. Has the risk of COVID-19–related mortality changed overall and for specific demographic groups?
- Hospitalizations and deaths from COVID-19 have substantially decreased in the United States in recent months and remained relatively low during April–early November 2022. Outside of the initial waves of COVID-19–related deaths in 2020 and early 2021, which coincided with widespread transmission of the first SARS-CoV-2 variants in the United States, the largest peaks in COVID-19 deaths occurred during the Delta (July–October 2021) and early Omicron periods (January–March 2022). In these periods, a large peak in COVID-19 cases was followed by a peak in COVID-19–associated hospitalizations and, subsequently, large increases in COVID-19–related deaths. An increase in COVID-19 cases in July 2022 resulted in proportionally fewer deaths than seen during earlier periods in the pandemic.
- From April through September 2022, COVID-19–related mortality rates remained relatively stable; to date, this has been the longest interval during the pandemic in which the COVID-19–related mortality rate was less than 22 deaths per 100,000 for all age groups. However, during this period, 2,000–4,500 COVID-19–related deaths were reported weekly, and a higher number of all-cause deaths occurred in the United States compared to what was expected based on previous years of data (excess deaths).
- Adults aged 85 years and older remain at particularly high risk of dying, with the proportion of COVID-19–related deaths accounted for by adults in this age group increasing during April–September 2022 from ~28% to ~40% of COVID-19–related deaths. This is the highest proportion of any age group―despite adults ages 85 years and older accounting for only about 2% of the U.S. population. Throughout the pandemic, the COVID-19–related mortality rate among men has been higher than among women.
- During January–April 2022, mortality rates decreased significantly for all race and ethnicity groups among both younger people (under 65 years old) and older adults (ages 65 years and older). Although racial and ethnic disparities in COVID-19–related mortality have decreased over the course of the pandemic, disparities continued to exist.
- 2. How effective are vaccines at reducing the risk of dying due to COVID-19?
- COVID-19 vaccines continue to reduce the risk of dying among all age groups, including older adults, with the most protection observed among people with at least 2 booster doses.
- Despite changes in circulating variants over time, adults ages 65 years and older who are unvaccinated continue to have a much greater risk of dying from COVID-19 than people who are vaccinated; the same pattern exists for deaths across all age groups. Additional booster doses provide added protection; for example, in August 2022, adults aged 50 years and older with at least 2 booster doses had 3 times lower risk of dying from COVID-19 than adults of the same age with one booster dose.
- 3. Is COVID-19 the underlying (primary) cause of all reported COVID-19–related deaths?
- The majority of COVID-19–related deaths continue to have COVID-19 listed as the underlying (primary) cause; however, over time a larger proportion of COVID-19-related deaths have COVID-19 listed as a contributing cause of death rather than the underlying cause. This pattern is occurring across both younger and older age groups and means that people are now more likely to have another health condition listed as their underlying cause of death. During January–September 2022, 77–80% of COVID-19-related deaths had COVID-19 listed as the underlying cause of death, compared to 91–92% of deaths in 2020.
- 4. Where do most COVID-19—related deaths occur?
- Although the highest proportion of COVID-19–related deaths continue to occur in hospitals, increasingly, these deaths have occurred in other settings such as homes, long-term care facilities and hospice facilities.
- During January 2020–April 2022, the majority (57–78%) of COVID-19–related deaths among adults aged 65 years and older occurred in the hospital. But since April 2022, inpatient hospital deaths have accounted for less than 50% of COVID-19–related deaths in this age group.
- 5. What do we know about patients who died in the hospital while hospitalized for COVID-19?
- The people most at risk of COVID-19–related in-hospital death continue to be older adults (ages 65 years and older), people with underlying medical conditions, people with disabilities, and people who are not up to date with COVID-19 vaccinations.
- Risk of dying while hospitalized for COVID-19 declined steeply during March–April 2022 and remained lower through August 2022 compared to rates observed during June 2021–February 2022. The risk of in-hospital death has varied in the periods when the predominant circulating SARS-CoV-2 strains have differed. The Delta variant period (July–October 2021) had the highest crude mortality risk overall compared to during January–June 2022 when the predominant circulating strains were Omicron variants and subvariants. Among patients hospitalized primarily for COVID-19, the proportion requiring intensive medical intervention such as noninvasive mechanical ventilation or invasive medical intervention declined between the Delta period and the January–June 2022 Omicron periods.
- COVID-19–related in-hospital deaths are rare (less than 1%) among younger adults; those that do occur are most often among unvaccinated patients. During May–August 2022, among adults aged 18–49 years old who died in-hospital due to COVID-19, 79% were not vaccinated.
- 6. Which evidence-based COVID-19 medications that can reduce COVID-19–related mortality are being used, and in which patients?
- Use of outpatient COVID-19 medications, like Paxlovid, has increased. Early evidenceExternal suggests that hospital admission rates and death rates are lower among those treated with medications compared to those who are not treated. The proportion of COVID-19 patients receiving outpatient COVID-19 medication during April–July 2022 was highest among adults ages 65–79 years (~50%).
- Findings from a recent study, included in the report, showed racial and ethnic disparities in outpatient COVID-19 treatment through July 2022. During April–July 2022, the percentage of COVID-19 patients ages 20 years and older treated with Paxlovid was 36% lower among Black patients than among White patients, and Hispanic patients were 30% less likely to receive it than non-Hispanic patients. The study found that these disparities existed among all age groups and patients with immunocompromising conditions.