Recommendations for Fully Vaccinated People
COVID-19 Homepage
Contact Tracer’s Interview Tool: Notifying People About an Exposure to COVID-19
Universal case investigation and contact tracing are not recommended. This tool can be used to notify priority close contacts.
A successful notification of exposure allows for an exchange of information with the person exposed to COVID-19 (close contact) and offers an opportunity to answer questions and provide referrals for testing, medical evaluation, vaccination, and other support services. The goals of this interaction are to inform the person that they may have been exposed to COVID-19, assess their medical condition and other risk factors, and gather information for continued monitoring and support. Developing trust and an empathetic rapport, while maintaining a professional relationship, is key to connecting persons exposed to COVID-19 to resources for quarantine, testing, and vaccination.
Case investigators and contact tracers have a primary purpose of preventing further spread of COVID-19 through timely identification of cases and contacts to isolate or quarantine if indicated. Prompt case investigation and contact tracing should remain the primary goal of the case investigation and contact tracing workforce. These public health workers can also help connect people to important prevention services and resources, such as COVID-19 vaccination.
This document provides suggested communication approaches for COVID-19 contact tracing. Scripts may need to be modified to address locality-specific needs, including but not limited to highlighting available resources, cultural nuances, exposure sites, and the capture of epidemiological data. Public health workers should use what is helpful and the best fit for the interaction; all questions or statements may not be required, and additional probing questions may be necessary. Programs are encouraged to share best practices in framing and phrases as they are identified.
Principles for Interacting with People Exposed to COVID-19
Language is important. Language sets the stage to build rapport with people exposed to COVID-19 and opens the door to honest dialogue. It is critical to establish open communication with people exposed to COVID-19 so they feel comfortable expressing what they need to safely quarantine if indicated and seek help if they develop symptoms.
When supportive statements and genuine concern are combined with active listening and open-ended questions, powerful information can be shared to interrupt the spread of the virus. Asking open-ended questions prompts a dialogue and elicits more detailed information. Oftentimes, the information is helpful in learning more about the person and their circumstances. Remember, each person is unique, and this is not intended as a script. The interviewer should carefully listen to responses and add or subtract questions as appropriate.
Principles for Interacting with People Exposed to COVID-19:
- Ensure and protect confidentiality.
- Demonstrate ethical and professional conduct.
- Create a judgement-free zone.
- Be open-minded (everyone has a unique story).
- Be attentive and respectful.
- Be aware of your own bias (cultural humility).
- Establish open dialogue and pause often to listen.
- Ask open-ended questions.
- Use reflective listening techniques.
- Use culturally and linguistically appropriate language.
- Employ critical thinking and problem solving.
- Adapt to address concerns and information that arise naturally during conversation.
- Identify areas of need and link to appropriate resources.
- Don’t overstep or overpromise.
- Set the stage for ongoing communication and support during quarantine.
Aims: Contact tracers introduce themselves and establish credibility. Verify contact information, build rapport, and address confidentiality.
Note to Contact Tracer: The primary focus of the contact tracing workforce should remain prompt testing and quarantine if indicated to prevent further spread of COVID-19, identify additional cases, and provide referrals for care to prevent disease complications. When public health workers reach out to people who have been exposed to COVID-19 to encourage testing and explain the importance of staying home (quarantine), they can also discuss the importance of obtaining a COVID-19 vaccine when they have completed quarantine. Public health workers can also explain vaccine eligibility, answer questions, dispel myths, and assist with vaccine scheduling when people are eligible.
Introduction
- May I speak with [respondent name]?
- Am I speaking with [respondent name]?
- Hello, this is [interviewer’s name stated and spelled out]. I am a/an [title] with the <xxxx health department>, calling for [respondent name].
- [For minors] Who is their/your parent/guardian? How can I reach their/your parent/guardian?
- What language(s) do you feel most comfortable speaking?
- [If language barrier and interpreter available] We can work with an interpreter (provide information on if that person will be connected or if will need to call back).
- [If language barrier and team member who speaks the individual’s preferred language is not available] A team member who speaks (language) will call you back.
- I am following up with you to discuss an important health matter. This call is private and intended to assist you with this matter. Is now a good time to talk privately? If not, what time works best for you?
- If you are not available now, let’s schedule a time to talk. We have some important health information for you and want to be sure that you can get the referrals and resources you may need, and answer questions that you may have.
Verifying Identity
- It is important for me to ensure that I am speaking with the right person. What is your full name and date of birth, please?
- Before we get started, I would like to make sure that the information we received is correct. Please spell your full name, and what name do you go by/what do people call you? What would you like me to call you?
Confidentiality and Privacy
- Before we go into detail, I want to be sure you understand that everything we discuss is confidential. This means that your personal and medical information will be kept private and only shared with those who may need to know, like your healthcare provider.
- What questions do you have about your privacy/confidentiality?
Reason for Call
- It has come to our attention that you may have been recently exposed to COVID-19.
- Has anyone already talked to you regarding your possible COVID-19 exposure? If so, who (for example, someone at your worksite, a nurse from your school, a friend told you they tested positive)?
- [If asked why someone would expose them] Some of the early symptoms of COVID-19 can look similar to other illnesses, and sometimes, people have no COVID-19 symptoms. You may have been exposed by someone who had no idea they were sick with COVID-19.
- [If asked] I don’t know who gave your information, but even if I did, I wouldn’t be able to share it with you, just like I cannot share your personal information with others. That information is protected by law.
- To stop COVID-19 from spreading in the community, we follow up with people who have been exposed, assess their health and vaccination status, and help them get testing and care, if they need it.
- We also ask them to quarantine, if indicated, and watch for symptoms. Quarantine helps prevent the spread of disease that can occur before a person knows they are sick or if they are infected with the virus without feeling symptoms.
- If people with recent exposure to COVID-19 test positive or have symptoms of COVID-19, we encourage them to isolate or stay home until it’s safe for them to be around others, wear a well-fitting mask (if able) when they need to be around other people, and monitor their symptoms until it is safe to discontinue home isolation. Do not go to places where you are unable to wear a mask.
- Someone cared enough about you to make sure that you were able to get this information, and the testing and medical care necessary to keep you, your family, and others healthy.
- This type of information can be overwhelming for many people. We want to work with you to help you get the care that you may need.
- I would like to review some important information and questions with you, so we can provide you with support and work together to stop the spread of COVID-19 in our city/county/town.
Q&A with Person Exposed to COVID-19
- What questions can I answer for you before we start?
Aims: Verify demographic and locating information. Establish the best way to reach the contact. Obtain information on residence, work and emergency contact numbers.
Introduction
- The next information that we will cover includes questions about you, where you live and who you live with. This information will help us make sure that your demographic information is correct and find out the best way to contact you.
Demographics
- I know that I already confirmed your name. Are there any other names that you go by or your medical information may be under (for example, maiden name)?
- What is your gender?
- What is your race?
- What is your ethnicity? Are you of Hispanic origin?
- Do you have a tribal affiliation? If so, which tribe?
- [For women] Are you currently pregnant? (If yes) How far along are you (months, weeks)?
- What is your [any other locally specific socio-demographic information]?
Locating and Contact Information
- Where do you stay (or live)? What is your address?
- Where else have you lived (or stayed) during the past month?
- [If person indicates that they ‘live on the street’] If you don’t have a regular place that you stay, where is it best to find you? [Probe for cross streets, site description, name of building/shelter, where they receive mail, etc.]
- Who else lives with you? (Who else stays at that address?)
- How many people regularly stay at that address?
- What is your cell phone number? Who else might answer that phone? What is the best time to contact you?
- What other ways do you like to communicate? (For example, email, app)
Work
- What do you do for work (name, location[s], hours)?
- Tell me about your work. What do you do there?
- Where do you work (name, location[s], hours)?
- Where else do you work (name, location[s], hours)?
- When was the last time you were at work?
Emergency Contact
- In case of an emergency, if I could not reach you, who would I call? What is their number? What is that person’s relation to you?
Aims: Gain insight regarding person’s knowledge of COVID-19. Provide disease-specific information. Assess potential COVID-19 symptoms, underlying health conditions and vaccination status. Make referrals for medical care, testing, and vaccination as appropriate.
Note to Contact Tracer: Case investigators and contact tracers assisting with vaccine navigation have access to case management databases with information on individuals from COVID-19 interviews and investigations. The information can be used to identify individuals at-risk of re-infection, those living in congregate settings, and those infected earlier in the pandemic who may have waning immunity. Case investigators and contact tracers can also work with epidemiologists to use surveillance and other data to identify “hotspots” of COVID-19 transmission and low vaccine uptake and prioritize areas for case investigation and contact tracing.
Assessment of vaccination status, prior COVID-19 diagnosis, and potential COVID-19 symptoms impact next steps for testing, quarantine, and isolation. The following recommendations should inform decision making:
- Most people who are up to date with COVID-19 vaccines with no COVID-like symptoms do not need to quarantine or be restricted from work. However, people who are up to date with COVID-19 vaccines should still be tested at least 5 days following an exposure to someone with suspected or confirmed COVID-19 and wear a well-fitting mask around others for a full 10 days after their last close contact with someone with COVID-19.
- People who are up to date should still monitor for symptoms of COVID-19 for 10 days after being around someone with COVID-19. Any person who experiences symptoms consistent with COVID-19 should isolate themselves from others, wear a well-fitting mask, and test for SARS-CoV-2 if indicated. The symptomatic person should inform their healthcare provider of their vaccination status at the time of presentation to care.
- People who have tested positive for COVID-19 within the past 90 days do not have to quarantine or get tested again as long as they do not develop new symptoms. People who have recovered from laboratory-confirmed COVID-19 within the past 90 days who develop symptoms consistent with COVID-19 should isolate immediately and get tested. Wear a well-fitting mask around other people. Do not go to places where you are unable to wear a mask. If you test negative but have symptoms of COVID-19 you should isolate away from others and contact your healthcare provider about your symptoms, follow-up testing, and how long to isolate.
Information collected about vaccination status, prior COVID-19 diagnosis, and potential COVID-19 symptoms, combined with state, tribal, local, and territorial (STLT) policies and procedures should guide recommendations for testing. Below are general testing recommendations:
- People who should consider testing for SARS-CoV-2 include people who have symptoms of COVID-19, people who have come into close contact with someone with COVID-19, people who are not up to date with their vaccines who are prioritized for community screening for COVID-19, and people who have been referred to get testing by their school, workplace, healthcare provider or health department.
Testing referrals, appointments, and turnaround time for test results should be modified to reflect locally relevant information, including primary care and other healthcare settings, local COVID-19 test sites, and health department resources.
Introduction
- I would like to take a few minutes to talk with you about the virus, check in on your health, and discuss how to keep you as healthy as possible and support you during this time. How does that sound?
Disease Comprehension
- There is a lot of information out there about COVID-19, and sometimes, it’s hard to know what is fact and what is myth. What questions do you have for me about the virus?
Prior COVID-19 Diagnosis
- Have you previously tested positive for SARS-CoV-2 or been diagnosed with COVID-19 by a healthcare provider?
- [If yes, to prior positive test or diagnosis] Tell me about why you first went to be tested/diagnosed for COVID-19? What was the date of your diagnosis? What type of test did you receive? What were the results? What symptoms did you have at that time? Have your symptoms resolved? Have you been tested again since that time? What were those results?
Symptoms of COVID-19
- COVID-19 can cause a variety of symptoms. Some COVID-19 symptoms can seem like a common cold, and others are more severe. Sometimes people have no symptoms. Please let me know if you have had any of the following symptoms and when they started.
[Note to Contact Tracer: See Appendix A for a table of COVID-19 symptoms, with space to indicate onset and duration. This information can help to identify contacts who will need to be referred for medical evaluation due to current symptom presentation and allow for discussion of which symptoms the contact should be “on the lookout” for during quarantine.]
- What symptoms were you having? [Note to Contact Tracer: See Appendix A for a table of COVID-19 symptoms, with space to indicate onset and duration.] When did those symptoms start?
- [If person states any of the emergency warning signs (for example, trouble breathing, persistent pain or pressure in the chest, new confusion, inability to wake or stay awake, or bluish lips or face) refer them for emergency medical attention immediately!]
- From what you are describing, it sounds as though you should be seen by a healthcare provider to further evaluate your symptoms as soon as possible. You need to call 911 or go to the emergency room. Wear a mask when an ambulance comes to get you and during your visit to the medical provider. Let them know that you received a call from the health department to notify you of possible exposure to COVID-19.
- [If yes to symptoms] If you have any of these symptoms, have you gone to see the doctor/ER/ healthcare provider (yes/no).
- [If yes, contact already seen by healthcare provider]
- What happened at the visit to your healthcare provider? Did you talk about COVID-19?
- Did your doctor/nurse/healthcare provider test or diagnose you with COVID-19? What type of test did you receive? What were your test results?
- How are you feeling now?
- We want to make sure that we can best support you, so we will have a health department liaison follow-up with you to discuss your health care visit and symptoms in more detail.
- [If contact not yet seen by healthcare provider]
- Given the symptoms you have described, it seems that you should be seen by a healthcare provider.
- Who is your primary medical care provider? What is their office location and phone number? Would you like to reach out to them today or would you like us to have <insert local public health services> follow-up with you to help with a referral for testing and a medical assessment? What is the best number for them to reach you at today?
- How will you get to your healthcare provider? Do you have a mask to wear during transport and while in the office? [Note to Contact Tracer: Discussing and problem-solving challenges, providing local resources is essential.]
- [If no to symptoms] It is good that you have not noticed any symptoms. It can take between 1–14 days for COVID-19 symptoms to show up, and in some instances, people with COVID-19 do not show any obvious symptoms, but they can still spread the virus. We don’t know yet if you have the virus or not. Let’s talk about some other risk factors for COVID-19 and then we can talk about next steps.
- What questions do you have for me at this time about COVID-19?
Underlying Health Conditions and Other Risk Factors
- Some other health conditions may impact how COVID-19 affects the body. Sometimes we may need to do extra monitoring for people who have other health conditions to be sure that we can get them help if they need it. Have you ever been diagnosed by your healthcare provider with any health conditions that might mean you should have extra monitoring for COVID-19? If so, what health condition(s) were you diagnosed with? [Note to Contact Tracer: If the local area is collecting data on specific co-morbidities, you may ask about those specific health conditions after asking this question.]
Verifying Vaccination Status
- Have you already received a vaccination for COVID-19?
If Respondent Says “Yes”: Which vaccine did you receive?
[If the person reports receiving a 2-dose series, such as the Pfizer or Moderna vaccine]: Did you receive both doses? When did you receive the second dose?
- [If the person reports receiving a single-dose vaccine, such as the Johnson & Johnson vaccine]: When did you get the single dose?
- [Ask if the person received a booster(s) dose]: Have you received a booster dose? Which one did you receive? When did you receive the booster?
- Option 1 [if the respondent is up to date with their vaccines]
- If your vaccine status is up to date and you’ve been around someone who has COVID-19 (close contact), you do not need to stay away from others (quarantine), or be restricted from work unless you develop COVID-like symptoms. We recommend that you wear a well-fitting mask for 10 full days after you last had close contact to someone with COVID-19 (the date of last close contact is considered day 0), and get tested at least 5 days after you last had close contact with someone with COVID-19.
- People who are up to date with their vaccine should still monitor for symptoms of COVID-19 for 10 days after being around someone with COVID-19. You should also wear a well-fitting mask in public indoor settings and monitor for symptoms for 10 days. Do not go to places where you are unable to wear a mask. You should isolate if you test positive. If you experience COVID-like symptoms, you should isolate from others for 5 full days after the start of your symptoms, wear a well-fitting mask, be clinically evaluated for COVID-19, and get tested. Tell your health care provider if you are up to date with your vaccines for COVID-19.
- Want to learn more about these recommendations? Read CDC’s Recommendations for Staying Up To Date with COVID-19 Vaccines.
- Option 2 [if respondent is not up to date on their vaccines]
- Since you are not up to date on your COVID-19 vaccines, you should quarantine for 5 full days, wear a well-fitting mask for 10 full days, get tested at least 5 days after close contact, and watch for symptoms. We will step through the specifics of this in a moment.
If Respondent Says “No, They Have Not Been Vaccinated” or Reports Receiving Only 1 Dose Out of a 2-Dose Series or have not received a booster dose: If quarantine is indicated, you will be eligible to receive vaccination or a booster, after completion of your quarantine period. In some situations close contacts can receive a vaccine during their quarantine period if it is offered by the health department in response to an outbreak. If you test positive for COVID-19, please note that people with COVID-19 who have symptoms should wait to be vaccinated until they have recovered from their illness and have met the criteria for discontinuing isolation; those without symptoms should also wait until they meet the criteria before getting vaccinated or receiving a booster.
This guidance also applies to people who get COVID-19 before they are fully up to date on their COVID-19 vaccines, including booster dose.
Testing for SARS-CoV-2
- Viral testing is recommended for close contacts of persons with COVID-19. If you are given a Nucleic Acid Amplification Test, or NAAT, it should take about <xxx> days to get your test results back. If you are given an antigen test, your test results might get back sooner. Once we know those results, we can determine the next steps. If you decide to use an at-home test, please communicate a positive result to your healthcare provider, who is responsible for reporting your test results to the health department. If the at-home test has an app that allows you to report your results to the state health department, inform your healthcare provider whether or not you used that app for results reporting.
- Following exposure to someone with suspected or confirmed COVID-19, people who are up to date with their COVID-19 vaccines should be tested at least 5 days after exposure to someone with suspected or confirmed COVID-19 and wear a well-fitting mask for 10 days after exposure. It is of particular importance that individuals who are up to date with their COVID-19 vaccines, including booster in the following settings get tested if exposed:
– Residents and employees of non-healthcare congregate settings (i.e., correctional facilities and shelters) who are up to date with their COVID-19 vaccines.
– Employees of high-density workplaces (e.g., poultry processing plants) who are up to date with their COVID-19 vaccines.
– Dormitory residents (or similar high-density housing settings) at educational institutions who are up to date with their COVID-19 vaccines.
Let’s talk about which of these circumstances may apply to you.
-
- [Where testing is indicated] When is the last time that you were tested for COVID-19?
- [If not tested since recent exposure] Since you have recent exposure to SARS-CoV-2, it is important to go in for testing as soon as possible. When will you be able to go for testing?
- Would you like to get testing for COVID-19 through your primary care provider or at the <insert local testing sites>? We have a list of test sites available. Let’s talk about which one is most convenient for you. How will you get to the testing site?
- What challenges do you anticipate with getting to the testing site? Will you have any difficulties with transportation to get to a testing site? Do you have other caregiver responsibilities, where you can’t leave someone alone? [Note to Contact Tracer: Discussing and problem-solving challenges, providing local resources is essential.]
- [If contact states that they have already been tested] So you have previously been tested for COVID-19? Where? When? What were the results?
- A negative result will mean that you didn’t have COVID-19 at the time you were tested. But we don’t know if you will develop the virus during the next <xxx> days or not, it is very important that you stay at home and quarantine [if indicated] starting today, to keep your family, household members, and others in the community safe.
- If your viral test results come back positive, that means that you have COVID-19 (regardless of whether or not you have symptoms). All people (regardless of vaccination status) with positive diagnostic test results should isolate at home or, if in a healthcare setting, be placed on appropriate precautions.
- If your test is positive, tell your close contacts that you have COVID-19 right away so that they can stay at home, wear a well-fitting mask, and get tested. Choosing to help us slow the spread of COVID-19 helps protect you, your family, and your community.
Q&A with Person Exposed to COVID-19
- This was quite a bit of information. What questions do you have that you would like to discuss?
- Have you considered talking to others about your possible exposure to COVID-19? Who would you want to tell?
Aims: Discuss parameters and importance of quarantine recommendations. Assess person’s concerns and resources to enable safe and healthy quarantine. Cooperatively identify potential areas for support and referral.
Note to Contact Tracer: Information from the prior section (assessment of vaccination status, prior COVID-19 diagnosis and potential COVID-19 symptoms) and STLT policies and procedures should guide recommendations for quarantine and isolation and health monitoring. Below are general recommendations for the use the components of this guide:
- Quarantine Recommendations relevant for unvaccinated persons that have recent exposure to COVID-19 but have not tested positive or experienced symptoms
- Isolation Recommendations relevant for all persons with positive viral tests or experiencing symptoms of COVID-19
- Assessing Concerns, Living Situation and Other Supports, Disclosure Coaching relevant to those for whom quarantine or isolation is recommended
- Health Monitoring and Responding to Changes in Health Status relevant for ALL persons with recent exposure to SARS-CoV-2
- Conclusion relevant for ALL persons with recent exposure to SARS-CoV-2
There may be additional exceptions to the 5-day recommendation for quarantine for people with recent exposure to SARS-CoV-2. These include:
- People who are up to date with their COVID-19 vaccines with no COVID-like symptoms do not need to quarantine, but should be tested at least 5 days after last exposure to someone with COVID-19. People who are up to date on vaccines do not need to quarantine, but should still watch for symptoms of COVID-19 and wear a well-fitting mask for 10 days following an
- People who have been diagnosed with COVID-19 within the last 90 days and recovered do not have to quarantine or get tested again as long as they do not develop new People who do not need to quarantine should still monitor for symptoms of COVID-19 and wear a well-fitting mask for 10 full days following an exposure.
- People experiencing COVID-19 symptoms within 90 days of recovering from another bout of COVID-19 may need to isolate and be tested again if there is no other cause identified for their People should wear a well-fitting mask for 10 full days after symptoms start. Do not go to places where you are unable to wear a mask.
Recommendations for isolation include:
- People who have symptoms consistent with COVID-19 should get tested. While waiting for test results, they should stay away from others, including staying apart from those living in their household. (See If You Are Sick).
- People who experience symptoms consistent with COVID-19 should isolate themselves from others, get tested, and wear a well-fitting m ask for 10 full days after symptoms start. They should inform their healthcare provider of their vaccination status at the time of presentation to
- People who have been diagnosed with COVID-19 within the last 90 days and recovered that develop symptoms should isolate immediately and get tested.
- All persons (independent of vaccination status) with positive diagnostic test results should isolate at home or, if in a healthcare setting, be placed on appropriate precautions.
Quarantine Recommendations
- Now, I’d like to talk with you about home quarantine, review the recommendations, and identify what you may need to support you and keep you and your family and other household members healthy. How does that sound?
- First, let’s talk about who should quarantine. You do not have to quarantine after exposure to COVID-19, as long as you do not develop new symptoms, if you:
- Are up to date on your COVID-19 vaccines and do not currently have symptoms, or
- Have tested positive for and recovered from COVID-19 within the past 90 days and do not currently have symptoms.
From what we discussed earlier, it appears that <xxx>, applies to you, so you won’t need to quarantine. However, with recent COVID-19 exposure, both people who are up to date on their COVID-19 vaccines and those who have tested positive for COVID-19 within the past 90 days should still monitor for symptoms of COVID-19 for 10 days following an exposure and wear a well-fitting mask for 10 days after the exposure. If you experience symptoms, you should stay at home and away from others, contact your healthcare provider to discuss your symptoms, vaccination status, and next steps (for example, testing).
- [For people recommended to quarantine] Since we don’t know yet if you will develop COVID-19, you will need to stay at home. During quarantine you will need to:
- Stay at home for 5 full days from the day when you were exposed toCOVID-19. That means staying at home for <xxx> days or until [date].
- Wear a well-fitting mask for 10 full days after exposure. Do not go to places where you are unable to wear a mask.
- To take care of yourself and others, limit your interactions with people in your household, staying 6 feet (2 meters) away from them. To minimize your contact with others, if at all possible, stay in your room and have food, other necessities, and recreational items left outside the
- When interacting with others in your household, you should wear a well-fitting mask over your nose and mouth to help protect others in case you’re infected but don’t have symptoms. Your caregiver should also wear a well-fitting mask when caring for you. Children under age 2 or anyone who has trouble breathing should not wear a mask.
- If at all possible, you should avoid contact with other people (unless they live in the same home and had the same exposure as you), regularly wash your hands, and follow other measures outlined in the CDC guidance of how to protect yourself and others.
- Monitor your health and watch for symptoms. Watching for fever (100.4°F), cough, shortness of breath, or other symptoms of COVID-19, and contacting your healthcare provider if you develop symptoms
- There are a number of things you can do to protect your family and other household members. I will provide information on how to clean and disinfect your home (for those sharing space with others).
- It will be important to identify other people to assist you with daily life activities during quarantine. You may need others to support you in grocery shopping, picking up medications, and caring for others during this time. If you have pets, you should treat them as you would other human family members to protect them from a possible COVID-19. So, you may need assistance in taking care of them. In accordance with the Americans with Disabilities ActExternal, service animals are permitted to remain with their handlers. COVID-19 and Animals Frequently Asked Questions.
- Have you already started staying at home and away from others (quarantine)? When did you begin quarantine?
Isolation Recommendations
- [Discuss if symptomatic] People with recent exposure, who have symptoms of consistent with COVID-19 should get tested. While waiting for test results they should isolate or stay away from others, including staying apart from those living in their household. (See When You Are Sick).
- [Discuss as relevant] Any person who experiences symptoms consistent with COVID-19 should stay at home and be clinically evaluated for COVID-19, including SARS-CoV-2 testing, if indicated. They should wear a well-fitting mask and inform their healthcare provider of their vaccination status at the time of presentation to care.
- [Discuss as relevant] People who have been diagnosed with COVID-19 within the last 90 days and recovered that develop symptoms again should isolate immediately and get tested.
- [Discuss with those who have a positive test result] All people (independent of vaccination status) with positive diagnostic test results should isolate at home or, if in a healthcare setting, be placed on appropriate precautions.
- A health department liaison will follow up with you to talk about your COVID-19 diagnosis and next
Assessing Concerns
-
- What would quarantine look like for you?
- What concerns do you have about the situation that I just described? [Note to Contact Tracer: Validating concerns, exploring solutions, and offering support/resources (as appropriate) is essential.]
- Does this sound like something that would be hard or easy for you? Why? What could you do or what support would you need to address the hardest parts?
- What would be helpful for you to better understand or remember the instructions about quarantine?
Assessing Living Situation
- It may be helpful to talk about what kind of support you might need during quarantine.
- Let me just double check the address where you are staying (confirm address).
- What does your living situation look like? [Note for Contact Tracer: Probe for type of living environment: single flat, apartment, house, group home, treatment facility, single room only hotel, condo, tent encampment, etc. How many rooms, bedrooms, bathrooms? Are there shared common areas (for example, kitchen/dining room/living room/laundry/elevator)?]
- Tell me about the place where you live (Prompts: House? Apartment?). Who lives there with you? What are their names, ages, and relationships to you?
- Who else stays there from time to time? When was the last time they were there? What are their names, ages, and relationships to you?
- How many children do you have? Where do they live?
- What pets or other animals do you have in your household?
- Would it be possible for you to have access to your own room and bathroom?
- How safe do you feel in your current living situation? Have you ever felt threatened or been hit or hurt by someone who you live with? [Note for Contact Tracer: If person feels unsafe or answers yes to the second question]We have resources to support you <make domestic violence referral— insert local information>
- Is there an alternate place that you could stay?
- Would you consider moving to an offsite location to support you and protect your family/ household during your quarantine? If this were an option, what would be your concerns?
Assessing Other Supports
- When you think about what I have just described, what comes to mind? What challenges do you see? What kind of support would you need to overcome them?
- What do you think will be the hardest thing about quarantine? How will you deal with that?
- Do you have access to fresh water and enough food?
- Do you have access to a mask/face covering(s)?
- How will you prepare your own food? Who can assist you with getting meals?
- How will you get other household supplies (for example, toilet paper, soap, etc.)?
- What medications will you need to take? How long until your prescription needs to be refilled? What would home quarantine look like for you?
- Who do you provide care for in your household? Children? Parents? Older person? Sick person? Is there someone else that can take on that role?
- What kind of supplies will you need for your pets or other animals during your quarantine? Is there anyone else who can take care of your pets or animals?
- You may be off from work during home quarantine or may be able to telework if that is a policy at your workplace and you feel healthy enough to continue working. How will you approach this discussion with your employer?
- What concerns do you have about the financial impact that home quarantine will have?
- What types of medical or other important appointments do you have scheduled over the upcoming weeks? Let’s see how we can work to support you with those.
- What other supports might you need during your quarantine period? [Note to Contact Tracer: Explore bullets below. Local resources should be listed and discussedPdf.]
- Food
- Childcare
- Housing
- Prescriptions
- Non-COVID medical care
- Support with stress, resiliency, mental health
- Substance use treatment/support groups
- Communication (cell service, internet)
- Translation/interpretation
- Assistance caring for someone else
- Transportation
- Disability accommodations
- Financial assistance
- Other
Disclosure Coaching
- Given that there will need to be a plan for social distancing and also supports set in place to assist you while you are on home quarantine, it will be important to think about how to talk about this with those in your household.
- Who in the household are you planning on telling about your exposure to COVID-19? What do you expect that discussion to look like? [Note to Contact Tracer: Offer coaching if appropriate.] Would you like information on how to tell them about your exposure?
Q&A with Person Exposed to COVID-19
- What other concerns (e.g., someone may be sick, someone may have a pre-existing health condition) do you have regarding the home quarantine instructions, the members of your household or being separated from them during self-quarantine? Let’s discuss some steps to take that may address your concern(s).
- Who in your household has been sick recently? (If yes, what type of symptoms, when started for how long)
- Have they gone to the doctor or to get tested for COVID-19? (If yes, when and where, results?)
- What questions or concerns do you have about self-quarantine that we have not covered?
Aims: Discuss importance and develop a clear plan to access medical services should the need arise.
Responding if Symptoms Develop
- You will need to be aware of what is happening with your body, so that you can tell if you are developing any of the symptoms that we discussed.
- If you develop any of the symptoms we discussed earlier, you should reach out to your primary care provider or the health department liaison/public health nurse so that they can assist you in getting care.
- Sometimes people with COVID-19 can have complications. If you have any emergency warning signs (including trouble breathing, persistent pain or pressure in the chest, new confusion, inability to wake or stay awake, or bluish lips or face). If you have any of these or any other symptoms that are severe or concerning to you, please call your medical provider or go to the emergency room right away. Don’t wait for your daily check-in. If you call 911 or go to the emergency room, wear a mask when an ambulance comes to get you or if you visit a medical provider. Also let them know that you received a call from the health department to notify you of possible exposure to COVID-19.
- What is your plan if you develop symptoms? [Note to Contact Tracer: Feedback and suggestions should be provided as relevant ]
- How would you get to the emergency room if needed?
Medical Provider and Other Support
- What medical appointments/procedures do you have ahead of you? How comfortable do you feel communicating with them about being on quarantine?
- Who do you feel comfortable reaching out to if you develop symptoms and you feel like you need support?
Aims: Discuss importance and benefits of getting vaccinated. Assess person’s concerns and resources. Cooperatively identify potential areas for support and referral.
Note to Contact Tracer: Refer to CDC’s Interim Clinical Considerations for Use of COVID-19 Vaccines Currently Authorized in the United States and Different COVID-19 Vaccines webpage for information on vaccine eligibility. There is more information about vaccines on CDC’s Staying Up To Date With Your Vaccines webpage. Information that may be helpful to guide the discussion includes:
- Key Things to Know About COVID-19 Vaccines
- Frequently Asked Questions about COVID-19 Vaccination
- Engaging Patients for COVID-19 Vaccination
- COVID-19 Vaccines Factsheet
- How do I find a COVID-19 vaccine?
- COVID-19 Vaccine Information for Specific Groups
- Benefits of Getting Vaccinated
To assist with access to vaccination services, contact tracers should have information related to vaccine eligibility, safety, and availability. This includes access to:
- Vaccine locations
- Scheduling systems
- Digital tools (for example, mobile phones and tablets)
- Vaccine education for staff and people receiving assistance with access to vaccination services
- Key messages promoting vaccination
- Surveillance data (case, contact, and vaccine coverage)
-
- Once you are eligible to receive the vaccine, we highly recommend scheduling an appointment to get vaccinated or visiting a vaccination site that does not require an appointment. The federal government is providing the vaccine free of charge to all eligible people living in the United States, regardless of their immigration or health insurance status. Would you like our help with locating a testing site; finding a vaccination site; scheduling an appointment for you, your family members, or other close contacts; or sending you an appointment reminder?
- CDC recommends COVID-19 vaccination for all people who are eligible. This includes people who have previously had COVID-19. That’s because experts do not yet know how long you are protected from getting sick again after recovering from COVID-19. Even if you have already recovered from COVID-19, it is possible—although rare—that you could be infected with the virus that causes COVID-19 again.
- There are several ways you can look for vaccination providers near you.
- Visit Vaccines.gov to find vaccination providers near you. In some states, information may be limited while more vaccination providers and pharmacies are being added. Learn more about COVID-19 Vaccination Locations on Vaccines.gov.
- Text your zip code to 438829 or call 1-800-232-0233 to find vaccine locations near you.
- Check your local pharmacy’s website to see if vaccination appointments are available. Find out which pharmacies are participating in the Federal Retail Pharmacy Program.
- Check your local news outlets. They may have information on how to get a vaccination appointment.
- Safety is CDC’s top priority, and vaccination is a safer way to help build protection. The vaccines cannot give you COVID-19. All currently authorized and recommended COVID-19 vaccines are safe and effective, and CDC does not recommend one vaccine over another. The most important decision is to get a COVID-19 vaccination as soon as possible. Widespread vaccination, including boosters for those eligible, is a critical tool to help stop the pandemic.
- Some side effects are normal after you receive the COVID-19 vaccine. You can register for the
- V-safe After Vaccination Health Checker, a smartphone-based tool that uses text messaging and web surveys to provide personalized health check-ins after you receive a COVID-19 vaccine.
- We would like to connect you to vaccine services upon your release from quarantine. What would be most helpful to support you in getting your vaccine? Would you like us to follow up with you after your vaccination to provide additional support, if needed?
- What challenges do you think you may have with getting vaccinated? Will you have any difficulties with transportation to get to a vaccination site? Do you have other caregiver responsibilities, where you can’t leave someone alone? [Note to Contact Tracer: Discussing and problem-solving challenges, providing local resources is essential.]
- Is there anyone else in your household that could use assistance getting access to a COVID-19 vaccine?
Aims: Check-in on agreements. Answer remaining questions. Set stage for follow-up
Note for Contact Tracer: You or another public health worker can follow-up with people eligible for vaccination to ensure all doses have been received, ask if they experienced any side effects, and provide other support as needed. This may help build trust and promote vaccine services within the community.
Check-in, Questions and Agreements
- We have talked about a lot of topics today. I want to take a few minutes to check in on how you are feeling and discuss our agreements.
- How are you feeling about all of this?
- How can I (or my agency) be of additional assistance to you?
- What questions do you have about what will happen next with the information that we have discussed?
- And if you start to feel symptoms of COVID-19 your plan was to…?
Acknowledging the Difficulty and Keeping the Door Open for Contact
- I just want to check in to be sure that you know how to reach me if you have other questions or concerns after we get off the phone. My name is spelled, <insert name>, and my phone number is <insert phone number>.
- Either my colleague or I may reach out to you to check in to see if you are ok or whether you’ve connected with the other services we talked about today. They will also protect your privacy. We may have other questions that arise. Just wanted to confirm the best number to reach you is <repeat ‘best contact number’ provided by person>.
- I can’t thank you enough for talking to me and helping us stop the spread of COVID-19 in [location]. I know this is a very difficult time for you and your family, and we truly want everything to go well for you.
- Before we hang up, I just want to check on what additional questions you may have for me?
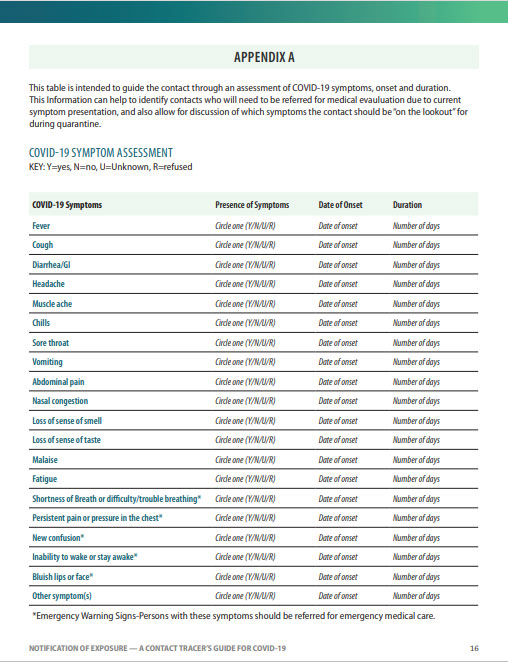
This table is intended to guide the contact through an assessment of COVID-19 symptoms, onset, and duration. This information can help to identify contacts who will need to be referred for medical evaluation due to current symptom presentation, and also allow for discussion of which symptoms the contact should be “on the lookout” for during quarantine.
COVID-19 Symptom Assessment
Key: Y=yes, N=no, U=Unknown, R=refused
*Emergency Warning Signs-People with these symptoms should be referred for emergency medical care.
PdfDownload Notification of Exposure Guide