Estimated Influenza-Related Illnesses, Medical Visits, Hospitalizations, and Deaths in the United States — 2019–2020 Influenza Season – Estimates represent data as of October 2021
Archived: The content of this page has be archived for historical purposes. The updated preliminary burden estimates for the 2019-2020 season have been updated and are available online. The overall burden of influenza (flu) for the 2019-2020 was an estimated 35 million flu illnesses, 16 million flu-related medical visits, 380,000 flu-related hospitalizations, and 20,000 flu deaths.
For the past several years, CDC has estimated the numbers of influenza illnesses, medical visits, hospitalizations, and deaths1–4. More information on How CDC Estimates Flu Burden and Why CDC Estimates Flu Burden is available.3
2019–2020 Burden Estimates
Influenza activity in the United States during the 2019–2020 season began to increase in November and was consistently high through January and February. The season was characterized by two consecutive waves of activity, beginning with influenza B viruses and followed by A(H1N1)pdm09 viruses. Overall, influenza A(H1N1)pdm09 viruses were the most commonly reported influenza viruses this season. Activity began to decline in March, perhaps associated with community prevention measures for COVID-19 (5-6). The 2019-20 season is described as having moderate severity; however, the effect of influenza differed by age group and the severity of the season in some age groups was higher. Hospitalization rates among children 0-4 years old and adults 18-49 years old were higher than observed during the 2009 H1N1 pandemic (6).
CDC estimates that the burden of illness during the 2019–2020 season was moderate with an estimated 38 million people sick with flu, 18 million visits to a health care provider for flu, 400,000 hospitalizations for flu, and 22,000 flu deaths (Table 1). The number of cases of influenza-associated illness, medically attended illnesses, hospitalizations, and deaths were lower than some more recent seasons and similar to other seasons where influenza A(H1N1)pdm09 viruses dominated (7, 8).
The 2019–2020 influenza season was atypical in that it was severe for children aged 0-4 years and adults 18-49 years where rates of infections, medically attended illnesses, hospitalizations, and deaths were higher than those observed during the 2017-2018 season, a recent season with high severity (7). The burden of influenza and the rates of influenza-associated hospitalization are usually higher for the very young and the very old, and while this was observed during the 2019–2020 season, rates of hospitalization in adults aged 18-49 years were the highest seasonal rates seen since the 2017-2018 season (Table 2). These rates mean that an estimated 15 million cases of influenza in younger adults (aged 18-49 years), which is the highest number of infections for this age group since CDC began reporting influenza burden estimates in the 2010-11 season.
CDC’s estimates of hospitalizations and mortality associated with the 2019–2020 influenza season show the effects that influenza virus infections can have on society. More than 52,000 hospitalizations occurred in children aged < 18 years and 86,000 hospitalizations among adults aged 18-49 years. Forty-three percent of hospitalizations occurred in older adults aged ≥65 years. Older adults also accounted for 62% of deaths, which is lower than recent previous seasons. These findings continue to highlight that older adults are particularly vulnerable to severe disease with influenza virus infection. An estimated 7,800 deaths (36% of all deaths) occurred among working age adults (aged 18–64 years), an age group for which influenza vaccine coverage is often low (9). This also underscores that influenza viruses can affect individuals of any age and prevention measures such as vaccination are important to reducing the impact of the seasonal epidemics on the population and healthcare system.
Deaths in children with laboratory-confirmed influenza virus infection have been a reportable disease in the United States since 2004; 199 deaths were reported for the 2019-20 season as of May 27, 2021. However, influenza-associated pediatric deaths are likely under-reported, as not all children whose death was related to an influenza virus infection may have been tested for flu (10,11). Therefore, we used a mathematical model to estimate the total number of pediatric deaths based on hospitalization rates and the frequency of death in and out of the hospital using death certificates. We estimate that at least 434 deaths associated with influenza occurred during the 2019-2020 season among children aged <18 years.
Conclusion
During the 2019-2020 influenza season, CDC estimates that influenza was associated with 38 million illnesses, 18 million medical visits, 405,000 hospitalizations, and 22,000 deaths. The influenza burden was higher in young children (0-4 years) and adults (18-49 years) compared with a recent season with the 2017-2018 season, a recent season with high severity, and provides evidence to support how severe seasonal influenza can be at any age.
Burden Estimates Limitations
These estimates are subject to several limitations.
First, rates of influenza-associated hospitalizations are based on data reported to the Influenza Hospitalization Surveillance Network (FluSurv–NET) through September 2, 2020. Final case counts may differ slightly as further data cleaning from the 2019-2020 season are conducted by FluSurv–NET sites. The most updated crude rates of hospitalization for FluSurv-NET sites are available on FluView Interactive (6).
Second, national rates of influenza-associated hospitalizations and in-hospital death were adjusted for the frequency of influenza testing and the sensitivity of influenza diagnostic assays, using a multiplier approach (3). However, data on testing practices during the 2019–2020 season were not available at the time of estimation. We adjusted rates using the lowest multiplier from any season between 2010–2011 and 2017–2018. Burden estimates from the 2019–2020 season will be updated at a later date when data on contemporary testing practices become available.
Third, estimates of influenza-associated illness are made by multiplying the number of hospitalizations by the ratio of illnesses to hospitalizations; estimates of medical visits are made by a similar process. These multipliers are based on data from a prior season, which may not be accurate if patterns of care-seeking have changed.
Fourth, our estimate of influenza-associated deaths relies on information about location of death from death certificates to calculate ratios of deaths occurring in the hospital to deaths occurring outside of the hospital by categories of causes of death. However, death certificate data during the 2019–2020 season were not available at the time of estimation. We used death certification data from all influenza seasons from 2010–2011 through 2017–2018 where these data were available from the National Center for Health Statistics. To calculate these ratios, first we calculate the frequency of flu-related deaths reported from our FluSurv-NET surveillance system that have cause of death identified as pneumonia or influenza (P&I), other respiratory or cardiovascular (other R&C), or other non-respiratory, non-cardiovascular (non-R&C). Next, to account for deaths occurring outside of a hospital, we use information from national death certificates to calculate the proportion of deaths from these causes that occur in and out of the hospital. Data to generate these frequencies were not available from the 2019–2020 season at the time of estimation, so we used the average frequencies of location of death for each of the cause categories from previous seasons, 2010–2011 through 2017–2018.
Fifth, estimates of burden were derived from rates of influenza-associated hospitalization, which is a different approach than the statistical models used in older published reports. This makes it difficult to directly compare our estimates for seasons since 2009 to those older reports, though the estimates from our current method are largely consistent with estimates produced with statistical models for similar years (12–13). However, it is useful to keep in mind that direct comparisons to influenza disease burden decades ago are complicated by large differences in the age of the US population and the increasing number of adults aged ≥65 years.
Why are these estimates lower than the preliminary in-season burden estimates last updated in April 2020?
These estimates are an update to the preliminary in-season 2019-20 burden estimates published April 2020 and are based on more recently available information. The current 2019-20 burden estimates are lower than those provided in April 2020 because of expected changes in available data on flu testing practices in patients hospitalized with flu, as well as unexpected data delays due to the onset of the COVID-19 pandemic in Spring 2020.
There is a trade-off between timeliness and accuracy of burden of disease estimates. To provide timely burden estimates to the public, clinicians, and public health decision-makers, CDC uses preliminary data that may lead to over- or under-estimates of the true burden. However, each season’s estimates will be finalized when data on testing practices and deaths for that season are available.
For these estimates, we included additional information to better capture flu testing practices at sites in the hospital-based surveillance system, FluSurv-NET, that collects data on patients hospitalized with laboratory-confirmed flu. Flu testing is done at the request of individual clinicians, but not everyone is tested, and flu tests are not perfectly accurate. Thus, reports of laboratory-confirmed flu-related hospitalizations to FluSurv-NET are underestimates of the true number of hospitalizations. To adjust for this, CDC collects data annually from participating FluSurv-NET sites on the amount of flu testing and the type of tests used at the site. This information is used to correct for the underestimates of flu-related hospitalizations. These testing data are often not available for up to 2 years after the end of a flu season, and thus the burden estimates are revised when additional testing data become available.
The preliminary in-season 2019-20 burden estimates were made using the highest flu testing rate for each age-group from the 2010-2011 through the 2016-2017 seasons. The current estimates were made using the highest testing rate for each age-group from the 2010-2011 through the 2017-2018 seasons. The additional data from the 2017-2018 flu season, which had high rates of flu testing, resulted in the 2019-2020 flu burden estimates being lower than those estimated earlier.
In addition to expected changes in available data on testing practices and patients hospitalized for flu, there were unexpected data delays due to the onset of the COVID-19 pandemic in Spring 2020. The method used to estimate flu-related deaths relies on additional data from FluSurv-NET and the National Center for Health Statistics (NCHS) (data on cause of death and numbers of deaths that occur inside versus outside of the hospital). The additional mortality data from FluSurv-NET are typically not available for up to 2 years after the end of a flu season. However, data from FluSurv-NET that is usually available at the end of flu season was delayed in 2020 due to the onset of the COVID-19 pandemic.
The 2019-2020 estimates that are presented here remain preliminary because not all of the data needed for final estimates are available. When additional data become available, these estimates will be updated again, and the results may change.
More answers to frequently asked questions about CDC’s influenza burden estimates are available.
†95% Uncertainty intervals
*Some of the data used to calculate burden estimates are incomplete or not yet available. These estimates will change as those data become available and the estimates are updated.
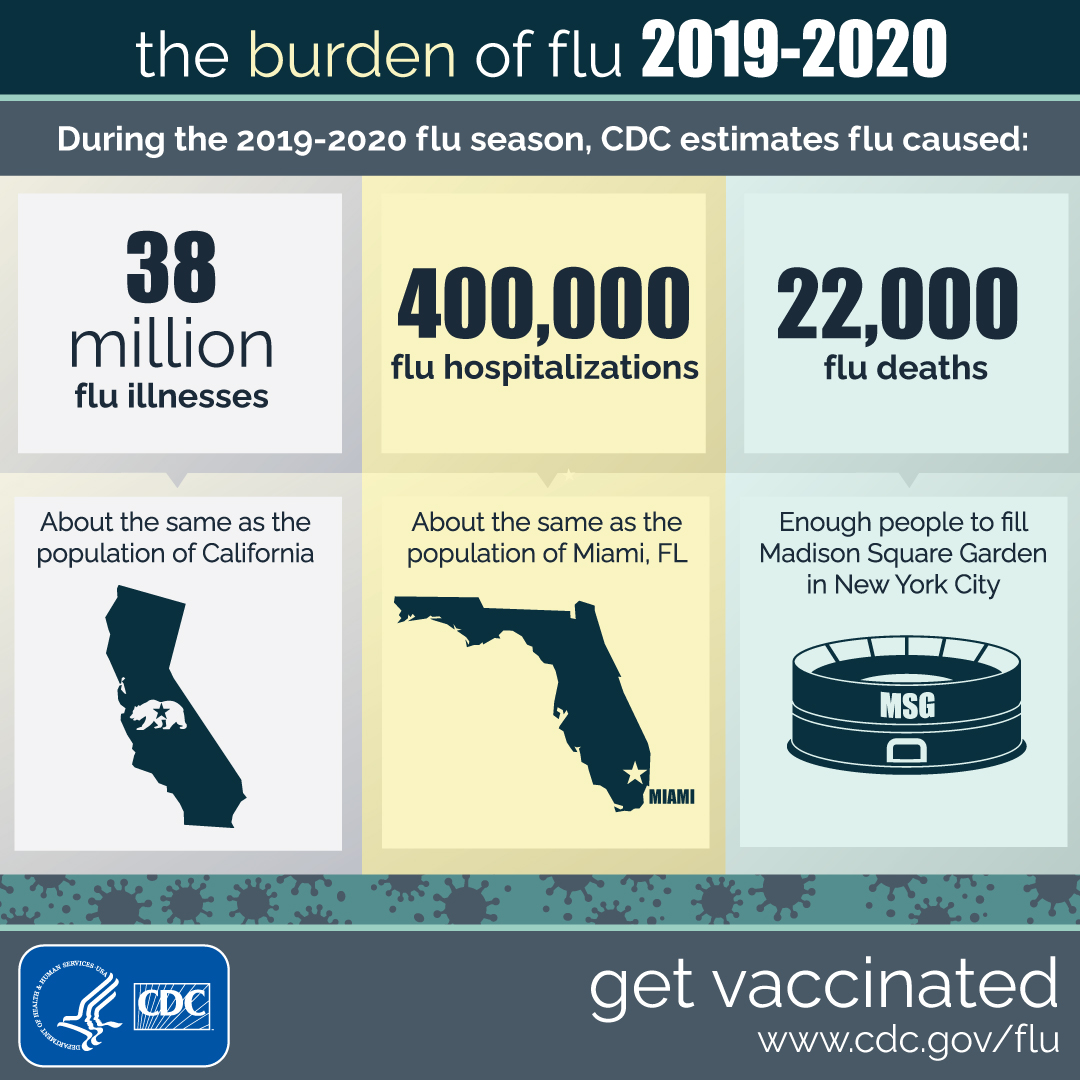
The Burden of Flu: 2019-2020 Infographic (Text Version)
The Burden of Flu: 2019-2020
During the 2019-2020 flu season, CDC estimates flu caused:
38 million flu illnesses, about the same as the population of California.
400,000 flu hospitalizations, about the same as the population of Miami, FL.
22,000 flu deaths, enough people to fill Madison Square Garden in New York City.
CDC logo
Get vaccinated.
References:
- Reed C, Chaves SS, Daily Kirley P, Emerson R, Aragon D, Hancock EB, et al. Estimating influenza disease burden from population-based surveillance data in the United States. PLoS One. 2015;10(3):e0118369.
- Rolfes MA, Foppa IM, Garg S, et al. Annual estimates of the burden of seasonal influenza in the United States: A tool for strengthening influenza surveillance and preparedness. Influenza Other Respir Viruses 2018; 12(1): 132–7.
- Centers for Disease Control and Prevention. Estimated influenza illnesses and hospitalizations averted by influenza vaccination – United States, 2012-13 influenza season. MMWR Morb Mortal Wkly Rep. 2013 Dec 13;62(49):997-1000.
- Reed C, Kim IK, Singleton JA, Chaves SS, Flannery B, Finelli L, et al. Estimated influenza illnesses and hospitalizations averted by vaccination–United States, 2013-14 influenza season. MMWR Morb Mortal Wkly Rep. 2014 Dec 12;63(49):1151-4.
- Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased Influenza Activity During the COVID-19 Pandemic — United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1305–1309. DOI: http://dx.doi.org/10.15585/mmwr.mm6937a6n
- Control, C.f.D. Flu Activity & Surveillance. 7/8/2020 [cited 2020 9/22/2020]; Available from: https://www.cdc.gov/flu/weekly/fluactivitysurv.htm.Garten R,
- Blanton L, Elal AIA, Alabi N, Barnes J, Biggerstaff M, et al. Update: Influenza Activity in the United States During the 2017-18 Season and Composition of the 2018-19 Influenza Vaccine. MMWR Morb Mortal Wkly Rep. 2018 Jun 8;67(22):634-42.
- Past Seasons Estimated Influenza Disease Burden. 2020. Available at: https://www.cdc.gov/flu/about/burden/past-seasons.html. Accessed September 30, 2020.
- Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2018-19 Influenza Season. September 26, 2019 [cited 2020 September 30]; Available from: https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm
- Shrestha SS, Swerdlow DL, Borse RH, Prabhu VS, Finelli L, Atkins CY, et al. Estimating the Burden of 2009 Pandemic Influenza A (H1N1) in the United States (April 2009–April 2010). Clin Infect Dis. 2011;52(suppl_1):S75-S82.
- Lees CH, Avery C, Asherin R, Rainbow J, Danila R, Smelser C, et al. Pandemic (H1N1) 2009–associated Deaths Detected by Unexplained Death and Medical Examiner Surveillance. Emerg Infect Dis. 2011;17(8):1479-83.
- Martin K, Strain A, Reagan-Steiner S, Lynfield R, DeVries A, Lees C, et al. Influenza-associated Pediatr Deaths Identified Through Minnesota’s Unexplained Critical Illness and Death Project – Minnesota, 2004-2017; Abstract 9836. Council of State and Territorial Epidemiologist. West Palm Beach, FL; 2018.
- Centers for Disease Control and Prevention. Estimates of deaths associated with seasonal influenza — United States, 1976-2007. MMWR Morb Mortal Wkly Rep. 2010 Aug 27;59(33):1057-62.
- Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004 Sep 15;292(11):1333-40.
- Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003 Jan 8;289(2):179-86.

