Overview of Influenza Vaccination among Health Care Personnel
Health Care Personnel (HCP) Categories
HCP include, but are not limited to, the following groups:
- Physicians
- Nurses
- Nursing assistants
- Therapists
- Technicians
- Emergency medical service personnel
- Dental personnel
- Pharmacists
- Laboratory personnel
- Autopsy personnel
- Students and trainees
- Non-employee contracted staff
Additional At-Risk HCP
Persons not directly involved in patient care, but who could still be exposed to infections in healthcare, are also considered HCP and include:
- Clerical
- Dietary
- Engineering
- Housekeeping
- Laundry
- Security
- Maintenance
- Administration
- Billing
- Volunteers[3]
HCP Working in Post-acute and LTC Facilities
As of 2014, over three million individuals delivered direct care as a part of LTC services; this was approximately one-fifth of the overall healthcare workforce [1]. By 2050, the number of HCP providing direct care in LTC settings is projected to increase to between 5.7-6.6 million [2]. Even staff who are not directly involved in patient care are considered HCP since they can be exposed to infections in healthcare settings. HCP can be defined as: all paid and unpaid persons working in healthcare settings who have the potential for exposure to patients and/or to infectious materials, including body substances, contaminated medical supplies and equipment, contaminated environmental surfaces, or contaminated air [3] (and includes staff not involved in direct patient care).
Each year influenza causes outbreaks in LTC facilities. The impact of influenza on LTC facilities can be particularly devastating since influenza can be a serious health threat, especially for people vulnerable to influenza complications, including older adults and people living with certain long-term medical conditions. People older than age 65 are at highest risk for hospitalization and complications from influenza and account for the majority of influenza hospitalizations and deaths in the United States each year [4].
Influenza Vaccination Coverage among HCP
The Advisory Committee on Immunization Practices (ACIP) recommends all HCP be vaccinated against influenza each year [6]. However, during the 2018–19 influenza season, influenza vaccination coverage was 68% among HCP working in long-term care settings, versus 95% among HCP working in hospitals [7]. This has been the trend for the past 8 influenza seasons [7]. Healthcare employers can take steps to improve voluntary uptake of vaccination by HCP, such as providing vaccine without charge at convenient times and locations and educating HCP about the importance of vaccination. The highest rates of vaccination are in settings that require it as a condition of employment. The Society for Post-acute and Long-Term Care Medicine advocates mandatory influenza vaccination of HCP (regardless of patient contact) in LTC facilities with exceptions made only in the case of medical contraindications to influenza vaccine [8]. Various other professional organizations also have policies supporting mandatory influenza vaccination of HCP.
Percentage of health care personnel who received influenza vaccination, by work setting* — Internet panel surveys,† United States, 2010–11 through 2018–19 influenza seasons
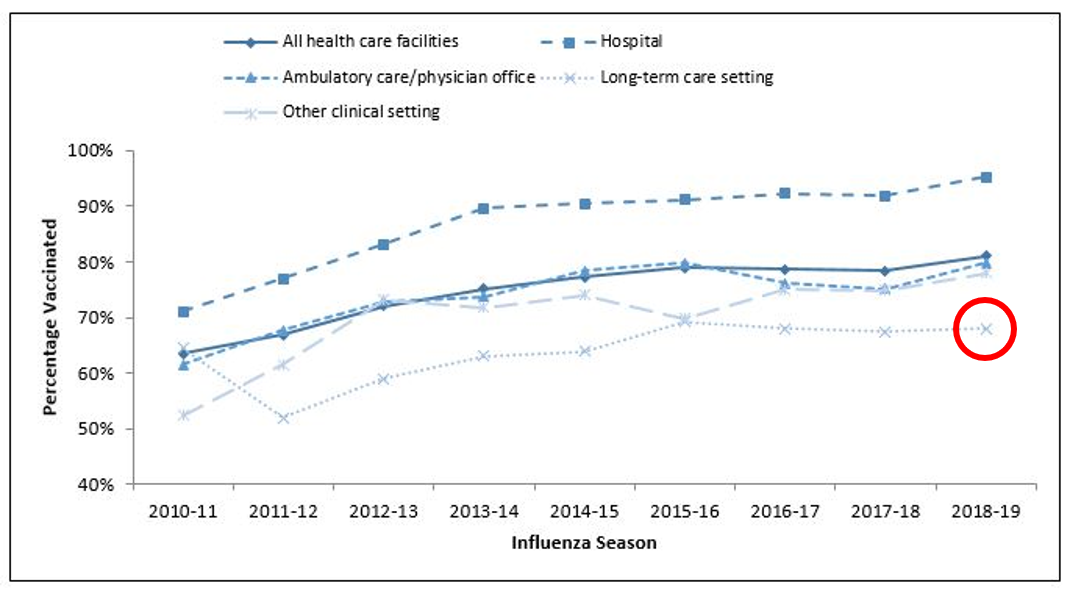
* Persons who worked in a place where clinical care or related services were provided to patients, or whose work involved face-to-face contact with patients or who were ever in the same room as patients.
† Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata.
Vaccinating HCP working in post-acute and LTC facilities is vital for preventing influenza transmission to residents
Benefits of Influenza Vaccination
Several studies have demonstrated that vaccination in healthcare settings decreases influenza transmission from HCP to patients, particularly in LTC settings [9, 10]. Studies in LTC facilities have shown that staff vaccination against influenza has been associated with reductions in all-cause mortality among residents [9, 10], influenza-like illness (ILI) [11], and hospitalizations of individuals with ILI. In addition, one LTC study suggested that although staff vaccination rates did not independently predict ILI outbreaks, high rates of vaccination among both staff and residents substantially reduced the rate and impact of influenza outbreaks [12].
- U.S. Government Accountability Office. Long-Term Care Workforce: Better Information Needed on Nursing Assistants, Home Health Aides, and Other Direct Care Workers. August 2016. https://www.gao.gov/products/gao-16-718. Accessed June 26, 2020.
- U.S. Long-term Care Workforce at a Glance: https://www.ahcancal.org/research_data/staffing/Documents/WorkforceAtAGlance.pdf. Accessed June 10, 2020.
- lnfluenza Vaccination of Health-Care Personnel: Recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP). MMWR 2006;55(RR02):1-16.
- Havers F, Sokolow L, Shay DK, et al. Case-control study of vaccine effectiveness in preventing laboratory-confirmed influenza hospitalizations in older adults, United States, 2010-2011. Clin Infect Dis 2016; 63(10): 1304-11.
- Stott DJ, Kerr G, Carman WF. Nosocomial transmission of influenza. Occupational medicine 2002; 52(5): 249-53.
- Centers for Disease Control and Prevention. Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices – United States, 2018-19 Influenza Season. 2018. MMWR 67 (RR-3); 1-20.
- Centers for Disease Control and Prevention. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2018–19 Influenza Season. https://www.cdc.gov/flu/fluvaxview/hcp-coverage_1819estimates.htm. Accessed August 10, 2020.
- The Society for Post-acute and Long-Term Care Medicine. Policy Statement on Influenza Vaccination of Health Care Personnel. https://paltc.org/sites/default/files/AMDA%20Flu%20Vaccine%20Policy%20Final2.pdf. Accessed June 10, 2020.
- Carman WF, Elder AG, Wallace LA, et al. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet 2000; 355(9198): 93-7.
- Potter J, Stott DJ, Roberts MA, et al. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis 1997; 175(1): 1-6.
- Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ 2006; 333(7581): 1241.
- Shugarman LR, Hales C, Setodji CM, Bardenheier B, Lynn J. The influence of staff and resident immunization rates on influenza-like illness outbreaks in nursing homes. Journal of the American Medical Directors Association 2006; 7(9): 562-7.