Core SVIPP Success Stories

The following success stories highlight how Core SVIPP implement, evaluate and disseminate injury and violence prevention strategies into action.
Partnership
Suicide
Adverse Childhood Experiences and TBI
- Illinois Public Awareness Campaign Promotes Positive Parenting to Prevent and Reduce Child Abuse and Neglect
- Oklahoma Strengthens Pediatric Concussion Efforts Through School Survey
- Utah Provides Traumatic Brain Injury Training for Homeless Shelters
- Washington Pushes for Prevention-Focused TBI Legislation
- New York Creates Momentum for Change with Adverse Childhood Experiences Data
- Minnesota Evaluates Abusive Head Injury Education in Hospitals
- Colorado: Mapping Problem Hot Spots Makes Colorado Schools Safer
- Ohio: Enhancing Child Safety Seat Education through Ohio Buckles Buckeyes (OBB) Program
- Oklahoma Fighting Infant Mortality
- Wisconsin Adverse Childhood Experiences
Motor Vehicle Safety
- Arizona Increases Access to Child Passenger Safety Technicians in Tribal Communities
- Kentucky Targets Motor Vehicle Crash Hot Spots for Education and Enforcement
- Massachusetts: Infusing Injury into the State Highway Strategic Plan
- Nebraska: Graduated Drivers Licensing (GDL) Educational Card for Teens
Data drives action, and health professionals rely on statistics to make informed decisions. These decisions may include resource allocation, program development and implementation, and where to provide services. Maryland injury and violence prevention stakeholders needed increased access to state injury and violence data. Many of these stakeholders found it difficult to find and analyze the data they needed. To address this need, Maryland’s Core State Violence and Injury Prevention Program (Core SVIPP) developed a new way to share current state injury and violence-related data and provide a general understanding of how that data informs the work and priorities of health professionals/organizations.
The MD Core SVIPP presented the 2019 Maryland Violence and Injury Prevention Data Landscape at an annual statewide injury prevention forum hosted by MD Core SVIPP and the Partnership for a Safer Maryland (PSM). The consolidation of state-level injury and violence-related data into a digestible and engaging presentation helps data dissemination, access, and use by identifying multiple partner media platforms for dissemination and archiving data in centralized locations. Updated annual reports will be available on the Prevention and Health Promotion Administration webpage.
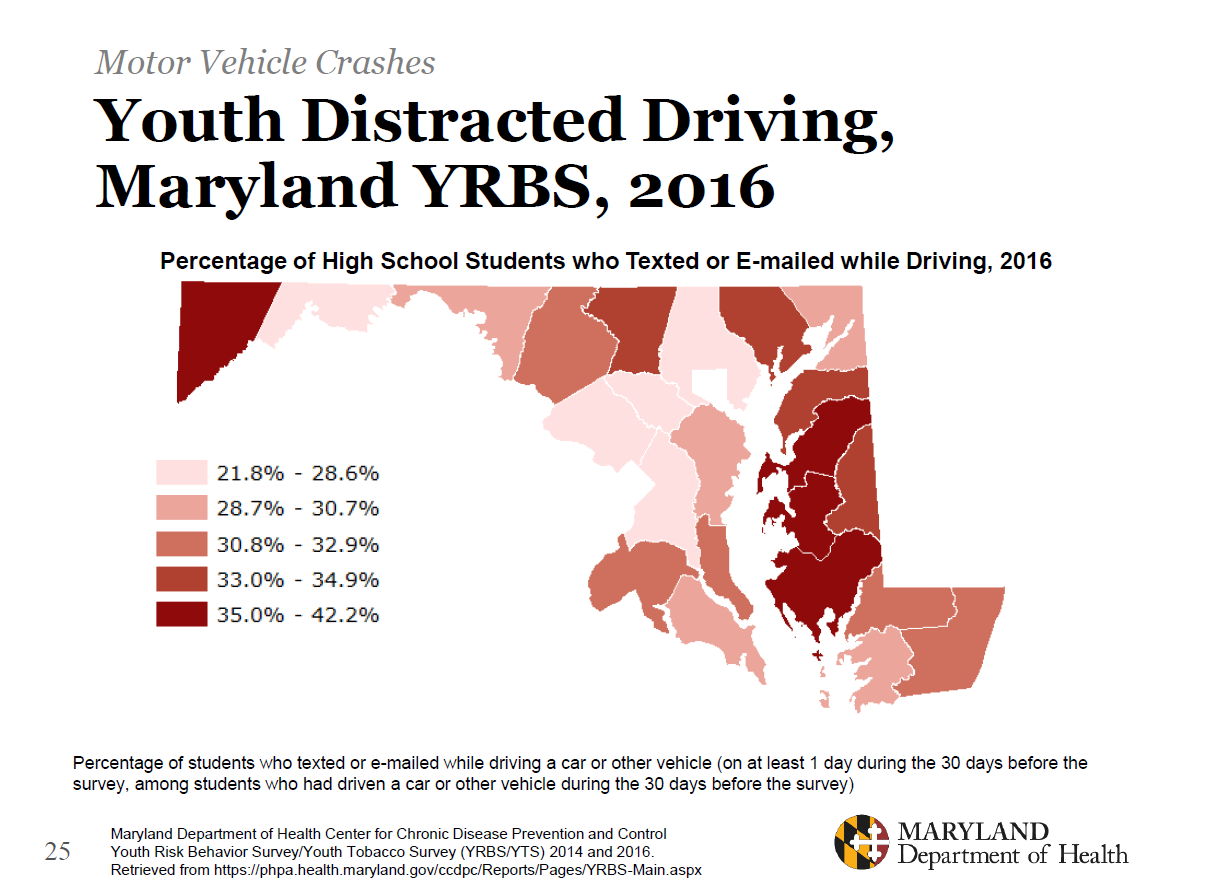
Here is an example of data found in 2019 Maryland Violence and Injury Prevention Data Landscape [PDF – 40 pages]:
Partnerships Were Key to Produce New Data Reports
MD Core SVIPP partnered with the Center for Injury Epidemiology within the Environmental Health Bureau (EHB) to provide the state’s injury-related mortality and nonfatal injury data and topic area-specific data. Several data resources were used such as unpublished data from the Health Services Cost Review Commission (HSCRC), the State Unintentional Drug Overdose Reporting System (SUDORS), and the Maryland Violent Death Reporting System (MVDRS). This included motor vehicle crashes and injuries, substance use, sexual violence/ intimate partner violence, and adverse childhood experiences. Not all Maryland jurisdictions have the epidemiological capacity to conduct injury and violence-related data collection and analysis and are directed to the Maryland Department of Health for data-related technical assistance.
Partners for this initiative include:
- Maryland Department of Health (MDH) staff from the EHB,
- MDH staff from the Behavioral Health Administration,
- local health department staff (Calvert, Charles, Prince Georges, and St. Mary’s counties),
- Partnership for a Safer Maryland,
- University of Maryland School of Law, and
- the Johns Hopkins Injury Control Research Center
MD Core SVIPP will continue to engage internal and external partners and regularly communicate with injury prevention professionals.
Suicide is a significant public health issue in Wisconsin. The suicide rate in Wisconsin increased by 40% from 2000-2017. In September 2020, Wisconsin (WI) released Suicide in Wisconsin: Impact and Response [PDF – 96 pages]. The two-part report includes state data and the state’s prevention plan. The data provide insight about the people and populations in WI who experience self-harm injuries, as well as suicidal thoughts, behaviors, deaths, and associated risk factors. The report then presents a comprehensive approach to reduce suicide attempts and deaths in WI. i
The plan consists of four strategies:
- Increase and enhance protective factors
- Increase access to care for at-risk populations
- Implement best practices for prevention in health care
- Improve surveillance of suicide and evaluation of prevention programs.
WI’s Core State Violence and Injury Prevention Program (SVIPP) anticipates this report will be used by local health departments and partners from multiple sectors to inform suicide prevention grants and program and policy development.
WI Core SVIPP and Partners Join Together to Address Suicide Prevention Statewide
WI Core SVIPP led a planning group with the WI Division of Public Health, Division of Care and Treatment Services; other sister state agencies, an academic injury research center, other state partners and advocates to develop a joint surveillance and prevention report. The report included data and guidance for suicide prevention for people of all ages, with specific recommendations to prevent adolescent suicide and self-harm The SVIPP epidemiologist and the WI Violent Death Reporting System coordinator collaborated with the Medical College of Wisconsin/Comprehensive Injury Center for the report’s surveillance data.
This was the first time WI’s Core SVIPP led partners with topical expertise in risk and protective factors all working together towards a combined report highlighting both the burden and prevention resources. The effort involved approximately 20 months of meetings, data review, prevention research review, and consensus-building among the planning group. The group gathered input from professional colleagues and advocates during the report development.
i Prevent Suicide Wisconsin. Suicide in Wisconsin: Impact and Response. September, 2020.
About 1 in 7 Children have Experienced Child Abuse and Neglect in the Last Year in the United States.
Child abuse and neglect can be physical abuse, sexual abuse, emotional abuse, medical abuse, educational abuse, and neglect. Children who are abused and neglected may suffer immediate physical injuries such as cuts, bruises, or broken bones, as well as emotional and psychological problems, such as impaired social-emotional skills or anxiety.
Most parents are not offered the opportunity to learn about positive parenting to address issues before they occur. Programs like Triple P are evidence-based options for upstream prevention of child abuse.
Core SVIPP Promotes the Triple P Program to Support Evidence-based Parenting Skills and Strategies
The Illinois Core State Violence and Injury Prevention Program (Core SVIPP) is working to reduce child abuse and neglect by promoting positive parenting through a public awareness campaign and connection to free community resources. Illinois Core SVIPP partnered with the Cook County Health Department (CCHD) to deliver a public awareness campaign to promote the Positive Parenting Program (Triple P) Model. The Triple P Model is a parenting and family support system designed to prevent and treat behavioral and emotional problems in children. Triple P provides parents with evidence-based parenting skills and strategies to support healthy relationships with their children. Core SVIPP and CCHD placed Triple P posters on public transportation in Chicago, Illinois. The posters highlighted three of the five Triple P core competencies:
- make life fun and safe for your child,
- be realistic about what your child can do, and
- take care of yourself.
The poster campaign guided families to ParentingAce.org for more resources, including where to find Triple P webinars and seminars. The campaign placed 371 posters and 8 digital screens on public transportation trains and buses for six weeks. The website had 548 page views and an average of 97 users a month.
Ad Campaign Reaches New Communities and Creates New Collaborations
ParentingAce hosted a free webinar about the Triple P program and two in-person Triple P seminars. The 30-minute informational webinar provided insight on the Triple P Positive Parenting Program Model. The webinar also informed attendees of the in-person seminars. The seminars are one type of training for providers and parents within the Triple P Model. They are 90-minute presentations on the basic concepts of positive parenting. The seminars took place in June 2019 with about 120 people including 13 providers.
The Triple P webinars have moved online since the COVID 19 shelter-in-place orders. Core SVIPP offers Triple P online codes on Facebook, through social workers at outpatient clinics, and to other organizations. Core SVIPP connected with the Brighton Park Neighborhood Network and provided the full series of Triple P seminars to one of the neighborhood schools. The principal made it mandatory that all the new kindergarten parents attend at least one session. She also invited all the other school parents to attend. Moving the Triple P Webinars online has broadened the program’s reach and increased its connection to the community.
The Illinois Core SVIPP program also connected with the Children’s Research Triangle, which partnered with Partnership for Resilience (P4R) to apply for the Substance Abuse and Mental Health Services Administration grant Project Linking Actions for Unmet Needs in Children’s Health. This grant promotes the wellness of children from birth to 8 years of age, by addressing the social, emotional, cognitive, physical, and behavioral aspects of their development. P4R and Children’s Research Triangle reached out to Parenting ACE to find out more about Triple P. They received the grant and are currently implementing Triple P in their parenting work.
Survey and Policy Review Creates New Concussion Prevention Efforts
Oklahoma (OK) Core State Violence and Injury Prevention Program (Core SVIPP) received 359 completed surveys from coaches and conducted reviews of concussion policies in 319 school districts. The results of the middle and high school coaches survey and policy review informed the development of new concussion education materials, concussion policy guidelines for school districts and youth sports organizations, and presentations at local, state, and national meetings and conferences. Education materials include audience-specific fact sheets for coaches, parents, and youth athletes and Return to Play and Return to Learn Protocols.
Partners in the Childhood Concussion Coalition helped to develop these materials. Regular meetings and communication with the Coalition have continued. The Coalition actively recruits new partners and community stakeholders as part of programmatic efforts. Previously no coordinated effort existed in the state representing healthcare, education, safety, community, and public health sectors. OK’s Regional Trauma Advisory Boards, composed of EMS, trauma, and first responder professionals, across the state received educational presentations on CDC’s Pediatric Mild Traumatic Brain Injury (mTBI) Guideline and healthcare provider mTBI materials.
Core SVIPP Evaluates Oklahoma Public Schools Concussion Policies and Coaches
OK Core SVIPP, known as Injury Prevention Service (IPS), recruited a diverse group of stakeholders and subject matter experts to serve on the Coalition. The Coalition set goals to strengthen prevention efforts across the state and to advise the IPS on related issues. The Coalition asked IPS to develop the middle and high school coaches survey and guidelines for concussion policy review. IPS collected, analyzed, and interpreted the data from the coaches survey and evaluated concussion policies from Oklahoma public school districts.
359 coaches completed the online survey. Some of the topics assessed included:
- years of coaching experience
- confidence in recognizing a concussion
- number of times removing an athlete for a suspected concussion in the past academic year
- level of perceived concussion prevention support
- sports coached
- grade level and gender coached
Overall, 88% of survey participants reported a high level of confidence in recognizing concussion symptoms and 55% of respondents reported removing an athlete from play for a suspected concussion 1-3 times over the past academic year. The most common qualitative responses from survey participants cited the lack of access to a licensed athletic trainer (AT) as a barrier to best practices for preventing and managing youth athlete concussions. OK Core SVIPP will use this information to advocate for the importance of ATs and for guiding programmatic efforts on education and training in schools.
IPS contacted 543 school districts for the school district concussion policy review and 319 responded (59% response rate). IPS received a total of 293 policies; 26 districts reported having no policy. The most frequently missing policy components required by OK law were requiring annual coach concussion training, setting penalties for not removing an athlete from play upon a suspected concussion, and not specifically prohibiting same-day return to play without written clearance from a healthcare provider.
OK Core SVIPP determined a need for a step-by-step guidance on policy developments, education, training, and individualized technical assistance addressing the missing policy components required by law. Core SVIPP developed two documents – Developing Concussion Policies: A Guide for Youth Sports Organizations and Developing Concussion Policies: A Guide for School Districts. These documents assist in writing and implementing policies for the prevention and management of sports-related and recreation-related concussions in accordance with Oklahoma state law. Guide dissemination and related training and education is anticipated during Summer 2021.
Concussion Data Underreported in Oklahoma
In OK, from 2016-2018, the Oklahoma State Department of Health, Health Care Information, Hospital Discharge Data reported 1,086 inpatient hospital discharges of children aged 0-18 years for traumatic brain injury (TBI), including concussions. The data underreport concussion prevalence as they do not account for injuries treated in other types of care settings or those not treated at all. According to CDC’s Management of Traumatic Brain Injury in Children: Opportunities for Action Report [PDF – 90 pages], 14% of children with a mild TBI will experience disability as a result of their injury.
High Rates of Traumatic Brain Injury Among People Who Experience Homelessness in Utah
A Utah Housing and Community Development Division report, Comprehensiveness Report on Homelessness, found that 25% of people experiencing homelessness who were surveyed in the greater Salt Lake Area reported suffering from TBI. Teams canvassed streets, parks, and waterways to survey 678 people experiencing homelessness, including both those staying in shelters and those not staying in shelters.
Core State Violence and Injury Prevention Program Trains Homeless Shelter Staff on TBI 101 Training
The Utah Brain Injury Council (UBIC) and the Utah Core Violence and Injury Prevention Program (Core VIPP) train caseworkers who work with youth who experience homelessness. The training is conducted at homeless shelters. The lifetime prevalence among homeless participants was 53% for any traumatic brain injury.i The Core VIPP staff is helping to coordinate additional traumatic brain injury (TBI) training and is continuing to expand partnerships between other local homeless shelters and UBIC. The modified training includes additional areas of concern and how to assess and assist those who experience homelessness with a history of TBI.
Partnerships formed as a result of the TBI 101 training. These partnerships helped ensure 30 staff members in homeless shelters received training on TBI in 2019. The UBIC plans to capture the number of individuals who experience homelessness and are connected to TBI services through the state’s TBI fund over the next year. The TBI Fund was established in 2008 by the Utah Legislature. The TBI Fund educates the general public and professionals on prevention and treatment of TBI.
Core State Violence and Injury Prevention Program Aided State in Creation of TBI 101 Training
The UBIC was asked by partners in the community who provide services to the homeless population to provide training on TBI to caseworkers and community health workers at the Road Home, a local homeless shelter. Utah VIPP co-facilitated the initial training along with another member of the council.
Before 2018, the TBI 101 training was not available for those that work with and support people who experience homelessness in Utah. The UBIC developed a new slide deck and brochure for TBI 101, which focused on the identification of TBI and strategies to support people who experience homelessness.
UBIC conducts community training for professionals who work within the health or social service systems. The TBI 101 training brings together community professionals to learn about the prevalence of TBI, signs and symptoms of a TBI, and what to do if you suspect someone has a TBI. UBIC members also share tips on preventing a TBI from occurring in the first place.
i: Hwang, Stephen W et al. “The effect of traumatic brain injury on the health of homeless people.” CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne vol. 179,8 (2008): 779-84. doi:10.1503/cmaj.080341
Comprehensive Plan Brings Focus on TBI Prevention
Washington State published its Comprehensive Statewide Plan [PDF – 20 pages] in January 2019. The plan focuses on a lifespan/developmental approach to traumatic brain injury (TBI). The plan looks at TBI prevention, TBI treatment, re-integrating into the community after the TBI, and living with a TBI long-term. The plan includes TBI prevention elements at each stage to make prevention a common theme. The plan is available to all citizens in Washington State on the Department of Social and Health Services (DSHS) TBI website.
The Comprehensive Statewide Plan is distributed by DSHS and Councilmembers through meetings, session hearings, presentations, and advocacy work. The TBI Council sponsors virtual support groups, seminars, symposiums, and conferences throughout the state focusing on prevention, education, and how to identify TBI symptoms.
Core Program Aids State in Creation of Comprehensive TBI Plan
The Washington State Department of Health (DOH) holds a seat on the TBI Council. This seat is currently filled by the Core State Violence and Injury Prevention Program (SVIPP) Health Services Consultant. The TBI Council develops a Statewide Comprehensive Plan to address TBI in Washington every 2 years.
The Core SVIPP representative educates the council on the importance of prevention across all severity levels of TBI. The representative encouraged a shift in focus from only post-injury support services to the prevention of TBI from an initial injury, and prevention of secondary injury if a TBI is sustained to reduce the likelihood of death. From February 2018 through December 2018, the TBI Council revised the Comprehensive TBI Plan with a focus on prevention.
With the assistance of the Core SVIPP representative, the Council prioritizes prevention activities such as up-stream approaches for prevention by developing a shared risk and protective factors framework in workgroups and final products.
The Public Health Burden of TBI is High
There were 5,940 people injured with a TBI in Washington in 2018. Washington State passed legislation to form the Traumatic Brain Injury Strategic Partnership Advisory Council (TBI Council) in 2007. The focus of this legislation is on support services after the injury. The TBI Council addresses the needs and gaps in services for people living with a TBI, and the Council has come to recognize that prevention is a valuable and necessary component of treatment, recovery, and long-term support services.
Adverse Childhood Experiences (ACEs) Are a Public Health Concern
ACEs are potentially traumatic events experienced by children under 18 years old. These events can have negative and lasting effects on health and well-being. They are linked to chronic health problems, mental illness, and substance misuse.
New York (NY) state had limited information on the burden of ACEs among its population and relied on national information and studies to drive its work. NY added questions regarding ACEs to its annual population health survey, the Behavioral Risk Factor Surveillance System (BRFSS) [PDF – 26 pages]. NY State Department of Health (DOH) surveyed more than 9,000 people over age 18. In NY, 6 out of 10 survey respondents (59%) reported experiencing at least one ACE, and 22% reported 3 or more ACEs. According to NY BRFSS, the higher the number of ACEs experienced, the higher the risk for unintentional and intentional injuries, negative health risk behaviors, and health conditions such as obesity, depression, suicide, and chronic obstructive pulmonary disease.
Core Program Data Expertise Critical to the State
The NY Core State Violence and Injury Prevention Program (SVIPP), housed within the DOH, analyzed and presented the survey data. During the analysis, NY Core SVIPP partnered with other programs within the DOH and other state agencies to create the BRFSS ACEs workgroup. NY Core SVIPP staff members provided subject matter expertise to interpret the data in meaningful ways, and they recommended ACEs-related interventions for use throughout the state.
Five action steps are recommended: [PDF – 26 pages]
- Facilitate cross-sectoral engagement in developing, implementing, and evaluating the action plan
- Offer technical support on best practices to prevent, reduce, and respond to ACEs
- Support alignment of actions to address ACEs
- Strengthen capacity for training and communications
- Collect data and information on ACEs and resilience periodically
Key Findings from State ACEs Report
For the first time, NY had state-based ACEs data to inform local action. The state’s ACEs report, Understanding and Responding to Adverse Childhood Experiences in New York State [PDF – 26 pages], was published online in June of 2018. Key findings were that experiencing three or more ACEs was higher among those who identified as lesbian, gay, bisexual, or transgender, those who had not graduated from college or technical school, and those with annual household incomes lower than $15,000. ACEs scores were lowest among adults 65 and older. ACEs were lower among men than women.
Participants who reported three or more ACEs were:
- Six times more likely to report being depressed
- Four times more likely to report HIV risk behaviors, including drug use
- Three times more likely to have arthritis or be current smokers
- Two times more likely to be obese, have asthma, or report binge drinking
These findings were reported in more than 14 presentations at local, regional, and national conferences. This report increased internal collaboration between the DOH Office of Public Health Practice and Opioid Overdose Prevention Program. The latter program hosted a conference called, “Integrating Adverse Childhood Experiences Science to Address Substance Use Disorders.” The conference brought together more than 120 people from state agencies, local health departments, and local offices for mental health. Attendees learned about the role ACEs can play in substance use disorder treatment and prevention. In addition, state agencies and non-profits used the data to apply for grants to conduct trauma-informed care and resiliency training.
NY Core SVIPP is working with partners through its Injury Community Implementation Group to support the efforts of local health departments and advocacy groups in using the report findings to prevent and address ACEs. Currently, NY Core SVIPP is collaborating with Prevent Child Abuse New York to develop a three-part training curriculum to change the service delivery of prevention services for child abuse and neglect. The curriculum will build and strengthen leaders at the community level.
Preventing ACEs and strengthening resilience are among the new statewide goals in the 2019-2024 Prevention Agenda, the state health improvement plan. As required by public health law, local health departments and non-profit hospitals in the state, in collaboration with community partners, must submit community health improvement plans that are aligned with the Prevention Agenda goals. The 2019-2021 local plans were submitted in December 2019.
Abusive Head Injuries Are a Leading Cause of Child Abuse Deaths in the United States.
Abusive head trauma (AHT), also known as shaken baby syndrome, is caused by violent shaking and/or with blunt impact. This causes damage to the brain and blood vessels as the brain repeatedly hits the skull. Nearly all victims of AHT suffer serious, long-term health consequences, such as vision problems, developmental delays, physical disabilities, and hearing loss. At least one of every four babies who experience AHT dies from this form of child abuse.
Core Program Implements Evidence-Base Approach to Address AHT
Dr. Mark S. Dias, a pediatric neurosurgeon, founded The New York Shaken Baby Prevention Project in 1998. The project educated parents of infants born in hospitals in Western New York about the dangers of violent infant shaking. Parents were taught about AHT in the hospital before being released to go home. This initiative reduced AHT injuries by 47% in Western New York. This became the foundation for implementing and evaluating this approach in Minnesota.
The Minnesota Core State Violence and Injury Prevention Program (Core SVIPP) partnered with the Brain Injury Interagency Leadership Council who developed a survey about AHT education. Hospital administrators at all birthing centers in the state completed the electronic survey, which asked if the hospital provided AHT education. The survey also asked if a signed statement was involved after the education was provided and if not, whether the hospital would be willing to incorporate one into its routine. The signed statement ensures parents viewed the video and understood the content. In addition, a sample of mothers who had recently delivered a baby at one of Minnesota’s birthing hospitals was asked about their experiences in receiving AHT education through a survey. Parents completed the parent survey at home.
Survey Highlights Gaps in AHT Education
The survey results provided interesting insight into implementation of the statute:
- 95% of hospitals in Minnesota reported having a video or program about AHT available for viewing by parents of newborns.
- 67% of mothers reported education about AHT had been offered while in the hospital.
- 57% reported a video being available and 40% reported viewing the video.
Minnesota hospitals may have the video available, but it may not always be offered. From the parent survey, most mothers responded that education about this topic is important, but 48% felt the hospital was not the right place to view the video/program. The survey showed mothers feel the video/program should be offered multiple times, including while they are pregnant and after their babies are born. To address the survey results, Minnesota Core staff are working with hospitals to encourage all parents of newborns to view the video or attend a program. They are also working with healthcare providers who care for pregnant women to address this topic at prenatal visits. Minnesota hospitals that reported not having a video or program available were contacted, informed of the statute, and provided references to available resources.
What is the problem?
One in five Colorado high school students report being bullied at school, and almost one in 10 have been physically hurt by a dating partner according to Colorado’s Youth Risk Behavioral Surveillance System. Five percent of high school students report that they have missed school because they felt unsafe at school or on the way to school. Colorado youth who identify as female, gay, bisexual, questioning, or transgender experience more violence than their peers. Bullying, youth substance abuse, mental health, sexual harassment, and violence have been shown to have potentially far-reaching impacts in young people’s lives. School climate – including social norms as well as the environment and school building — has been shown to influence these health outcomes.
What did the Colorado Core SVIPP do?
Colorado high school students and community members collaborated with Colorado’s Core State Violence and Injury Prevention Program (Core SVIPP) program, and the eight community Rape Prevention and Education (RPE) programs to implement the Shifting Boundaries – Building Component in schools and communities across Colorado to create safer spaces and build connections. Together, the collaborators identified safe and unsafe spaces in eight high school buildings, mapped the unsafe areas, and recommended community-level strategies to improve safety in the defined environments. The youth representatives presented their recommended strategies to the key stakeholders responsible for implementing community-level strategies to improve safety.
Colorado’s Core SVIPP funding supported infrastructure, training, and technical assistance to RPE-funded grantees to implement hot spot mapping. In addition, Core SVIPP funding supported evaluation of the hot spot mapping strategy by assessing the impact of both the process of engaging youth to identify problem areas, and assessing impact of the selected strategy on a variety of violence outcomes.
What was the outcome?
The collaborators engaged other local partners to fix problem areas such as installing permanent privacy walls in locker rooms for students, moving the girls’ locker rooms to ensure greater privacy among students, and increasing adult presence in shared spaces such as hallways.
Because of the Shifting Boundaries-Building Component collaboration, RPE-funded programs have strengthened partnerships with young people, school administrators, and community members. They have successfully integrated this strategy into existing school programming (i.e. healthy relationship curricula and social norms campaigns) and community initiatives, such as Communities That Care. Communities That Care is a program that promotes health youth development, improves youth outcomes and reduces problem behaviors.
Colorado’s Core SVIPP is collecting outcome data to evaluate their mapping and follow up strategies. Outcomes of interest include decreased cultural norms that support aggression as measured by the percentage of students reporting they carry a weapon to school; increased connection and commitment to school; and number of grantees reporting increased number of connections with community partners participating in the process (for increased community support and connectedness).
Colorado’s Core SVIPP are tracking and measuring long term outcomes on teen dating violence including: decreased percentage of adolescents reporting someone they were dating physically hurt them on purpose in the last 12 months and decreased percentage of adolescents reporting they have ever been forced to have sexual intercourse.
What is the problem?
Motor vehicle injury is a leading cause of death for children across the nation. From 2012 to 2015, motor vehicle crashes remained the leading cause of injury deaths for Ohio children ages 5 to 9 and third-leading cause for ages 1 to 4. From 2012-2016, 44 Ohio children under eight were killed as occupants in motor vehicle traffic crashes.
What did Ohio Core SVIPP do?
The Ohio Core SVIPP recognized the need for child safety seat distribution and installation education. They supported the creation of the Ohio Buckles Buckeye (OBB) program and established local child safety seat distribution and education sites for low income families in every Ohio county. Regional coordinators held car seat safety events and over 3,546 car seats were checked. Ohio is collecting data about the number of car seats that were installed correctly and incorrectly from program sites and data will be available in 2019.
What was the outcome?
In six months, Ohio provided low-income families in 88 counties access to 2,640 car seats along with education on proper installation and usage. The state trained 92 new car safety seat technicians and leveraged funds from partners to increase sustainability of the program. For example, because of the OBB accomplishments, the Ohio Department of Health received $227,891 from the Ohio Highway Safety Fund to purchase car seats from July 2017 through January 2018, and will continue this program. The National Highway Transportation Safety Administration (NHTSA) provided funding from The Child Highway Safety Fund to purchase child safety seats for the state’s 88 OBB Programs for low-income families.
What is the problem?
Oklahoma has one of the highest infant mortality rates in the country. Abusive head trauma (AHT), which includes shaken baby syndrome, is a preventable and severe form of physical child abuse that results in an injury to the brain of a child. AHT is most common in children under age five, with children under one year of age at most risk. Many people are unaware of the increased period of crying in early infancy (the Period of PURPLE Crying) leaving uninformed caregivers stressed, overwhelmed, and unprepared to cope.
What did the Oklahoma Core SVIPP do?
The Oklahoma State Health Department used the news media to connect with individuals to solve a real problem in their state: infant mortality. They released a statewide news release describing The Period of PURPLE Crying and CLICK for Babies. The Period of PURPLE Crying is an evidence-based educational program designed to help parents understand their baby’s crying and that their child is normal and healthy despite potentially crying for hours. This program is delivered in birthing hospitals in Oklahoma and includes two videos, a booklet, and bedside education on normal crying patterns, how to cope with relentless crying, and the importance of never shaking a baby.
Click for Babies is a public education campaign collecting handmade purple baby caps to give new parents along with educational materials. CLICK for Babies supports implementation of The Period of PURPLE Crying by raising funds and awareness not just in the state, but the Injury Prevention community at large on the topic of abusive head trauma prevention. The caps are given to newborns in local hospitals to increase awareness and educate families about the Period of Purple Crying to prevent shaken and abusive head trauma of infants. The news release included a call to individuals who knit or crochet to donate purple baby caps. The new release was picked up in national and international news and social media.
What was the outcome?
The news release’s call to action was met with an overwhelming response and the topic of abusive head trauma prevention went viral in traditional news media sources and social media. The Oklahoma Health Department received an unprecedented number of donations. In total, 69,914 purple baby caps were received from 2,876 donors. Donations came from 41 states and territories including the District of Columbia Puerto Rico and other Caribbean islands, and multiple countries across Central America, South America, Africa, Asia, Europe, and Australia. The program received enough caps to meet their original goal sixteen times over and supplied 82% of the states’ birthing hospitals. Oklahoma’s The Period of PURPLE Crying tapped into a sizable community of knitters internationally to help prevent abusive head trauma in infants. The work done by the state captured the hearts of a global community, encouraged life-saving conversations, and likely helped provide safer homes to babies born in Oklahoma.
What is the problem?
In 2010 it was estimated that there were 2.7 million minor children with an incarcerated parent [PDF – 3 pages] in the United States and that at least 10 million children have experienced parental incarceration [PDF – 22 pages]. When released from incarceration, women are at higher risk of returning to jail if they lose custody of their children. Adverse childhood experiences are potentially traumatic experiences or events that can have negative, lasting effects on health and well-being. Having a parent who is in jail is an adverse childhood experience that places children at higher risk for a broad range of poor social, emotional, and physical health outcomes including injury and violence.
What did the Wisconsin Core SVIPP do?
The state of Wisconsin partnered with their state Child Abuse and Neglect Prevention Board to address child abuse and neglect and reducing returns to jail among formerly incarcerated mothers. They pilot tested parenting skills classes for women in a re-entry facility (The Benedict Center in Milwaukee) who plan to return to their families and regain custody of their children when they are released from re-entry program. The Triple P Positive Parenting Program provides classes to build positive parenting skills and increase family support and connectedness. These are shared protective factors that increase families’ resilience to multiple forms of violence, including child abuse and neglect and suicidal behavior, and decrease rates of parents losing custodial rights of their children.
What was the outcome?
This pilot intervention focused on strengthening parenting skills among women in the process of being released from incarceration in order to reduce child abuse and neglect and loss of custody of their children. In the longer term, this program will potentially reduce Adverse Childhood Experiences by decreasing not only child abuse and neglect, but also recidivism and re-incarceration among these mothers. Triple P parenting education is not typically delivered in incarcerated settings. The short-term outcome of the pilot project was the establishment of a relationship between the service provider, the re-entry facility, and the department of corrections – where no relationship existed prior. Incarcerated and soon-to-be released women have an interest in parenting education and support classes, and several departments of correction and county detention facilities have been willing to allow service providers access to female inmates to provide the Triple P parenting classes. There are multiple locations supporting the delivery of Triple P classes in incarcerated settings in Wisconsin. Triple P International and regional staff are interested in the model and are working with providers to adjust the training guidelines. Triple P International is also interested in chairing a national work group to pursue the revision/adaptation of the Triple P parenting classes.
What is the problem?
American Indian and Alaska Native (AI/AN) children 0 to 12 years old have the highest traffic death rate of all racial/ethnic groups in the United States. Though AI/AN child safety and booster seat use rates vary greatly, AI/AN use rates are much lower than that of other racial groups. In a study of six Northwest tribes, proper restraint use among AI/AN children aged 7 years and younger ranged from 23% to 79%. In 2015, proper restraint use among children aged 0 to 7 years ranged from 63% to 87%. Using age and size appropriate car seats, booster seats, and seat belts significantly reduce the risk of injury and death among children in a crash.
What did the Arizona Core SVIPP do?
The Arizona Core State Violence and Injury Prevention Program (Core SVIPP) program provided a car seat technician training at the Salt River Pima-Maricopa Indian Community. They trained 20 new car seat technicians to administer the Children are Priceless Passengers (CAPP) class and conduct car seat inspections. This program educates the public on the effectiveness of proper use of child safety seats to reduce infant and toddler deaths and injuries. Nationally certified child safety seat technicians must teach each class. Core SVIPP staff coordinated the training and fostered a strong partnership with the Indian Health Service (IHS) to ensure community engagement. The lead instructor for the course was from IHS and trained previously through Core SVIPP. Arizona’s Core SVIPP also leveraged funds to purchase car seats and stepped in when funding was cut to the IHS Tribal Injury Prevention Cooperative Agreement Program grants to continue funding the passenger safety outreach.
What was the outcome?
Since becoming certified Child Passenger Safety (CPS) certified, instructors have held seven car seat compliance checkpoints trainings. There have been 20 curbside checkpoints where 247 car seats were inspected for their tribal communities. Currently, the CAPP Program has expanded to nine locations throughout the state. The CAPP Program has been recognized both nationally and statewide as a model community partnership program.
Kentucky’s seat belt rate is lower than the national average. In 2016, over half of those who died in motor vehicle crashes on Kentucky roads were not wearing their seatbelts at the time of death. Motor vehicle crashes affect crash victims, their families, friends, communities, first responders, medical personnel, and taxpayers. Enforcing existing laws can increase seatbelt use. Seat belt use can prevent motor vehicle crash injuries, minimize injury trauma, save lives, and decrease emergency and medical costs.
What did the Kentucky Core SVIPP do?
The Kentucky Office of Highway Safety (KOHS) and the Kentucky Violence and Injury Prevention Program (KVIPP) created a motor vehicle risk index hot spot map. It mapped motor vehicle collisions, human factors, fatalities, emergency department visits, and hospitalizations by county of residence. They identified ten counties with poor motor vehicle safety outcomes to target seat belt education and enforcement efforts.
Together with the Kentucky Safety and Prevention Alignment Network (KSPAN), KOHS and KVIPP implemented the Local Heroes campaign in the targeted high-risk rural counties. It ran during the national Click It Or Ticket campaign, a highly visible enforcement seatbelt campaign. The Local Heroes campaign spotlights well-known law enforcement in a local, community setting as the face of the campaign to encourage seatbelt use and increase connection between officers and their communities. Local officers participated in video, digital, and print public service announcements. The KOHS also used the hot spots map to target seat belt enforcement projects in the high-risk areas.
What was the outcome?
After the first year of the Local Heroes campaign, more drivers in the high-risk rural counties were observed wearing seat belts, and more citations were written by law enforcement.
The partnership between KOHS and KVIPP increased the number of pickup truck drivers wearing seat belts in high-risk counties in Kentucky by 0.6%. In addition, Kentucky’s overall seatbelt use percentage increased 0.3%. The collaboration between transportation and public health enables Kentucky to refine their education and enforcement efforts, and prioritize their efforts in high-risk counties.
What is the problem?
Motor vehicle crashes are a leading cause of death and disability across the life span in Massachusetts. They are also a leading cause of traumatic brain injury and share common risk and protective factors, such as substance use and misuse, with other injury and violence outcomes.
What did the Massachusetts Core SVIPP do?
The Massachusetts Department of Public Health was renewing the state highway strategic plan. This plan typically focuses on roadway design and engineering, and less on public health or behavior. The Injury Prevention and Control Director assessed the agenda and assigned a member from the Division of Violence and Injury Prevention to each emphasis area based on known overlap between programs and risk and protective factors linked to motor vehicle crashes.
Additionally, Core SVIPP staff took on the role of coordinating two emphasis areas: Young Drivers and Impaired Driving.. Core SVIPP staff worked to assure the public health voice was well represented and continues to be heard during the state highway strategic plan process. They identified areas that needed their involvement by using an overarching risk and protective factor approach for motor vehicle. The staff attended meetings, provided data, reviewed behavior and behavior change strategies, and provided context to additional programs, services, and gaps in the Commonwealth that would have otherwise been missed.
What was the outcome?
The State Highway Strategic Plan was launched on October 30, 2018. Core SVIPP staff members, and other injury and violence prevention practitioners within the Department of Public Health have identified new partners, learned about existing programs, and identified gaps. Further, the public health approach and data available about motor vehicle crashes are now better understood among state agencies involved in this process.
What is the problem?
Motor vehicle crashes are the leading cause of death for Nebraska teens. Graduated Drivers Licensing (GDL) was first implemented in Nebraska in 1998 with additional changes to strengthen the law in 2008. Nebraska’s GDL provisions work to reduce a teen’s exposure to high risk situations in order to reduce their involvement in a crash. Nebraska’s GDL allows new drivers time to develop critical driving skills under low risk conditions while reducing those things that cause greater risk. Nebraska teen crashes have been reduced by at least 60% since the implementation of the GDL law in 1998.
What did the Nebraska Core SVIPP do?
The Nebraska Department of Health and Human Services Injury Prevention program created, tested, and distributed a Graduated Driver Licensing (GDL) education card for parents and teens. The card contains information about important elements of the GDL law. It highlights laws against teen drivers using cell phones, driving under the influence of alcohol, and engaging in nighttime driving from midnight to 6 am unless the teen driver is going to or from school activities or work. The card also explains limitations on the number and age of passengers that teen drivers are allowed to transport and a requirement that all occupants riding with a GDL permit holder must wear a seat belt. The GDL card has shown to increase parent and teen knowledge about GDL driving restrictions, leading to better enforcement of the law by parents and better compliance by teens.
What was the outcome?
Nebraska Core SVIPP conducted an evaluation of a pilot program that distributed education cards to schools. Responses demonstrated the card increased both parent and teen knowledge of GDL, with over 70% of parents and 80% of teens responding “agree” or “strongly agree” to their willingness to use a parent-teen driving agreement. The GDL card encourages parent-teen driving agreements. For parents and teens not using a parent-teen driving agreement, 79% indicated willingness to use one after receiving the GDL card. The educational card was disseminated throughout the state in 2018.