Breaking Down Barriers to ED Care for People with SCD
Partner Toolkit
People with sickle cell disease (SCD) frequently visit the emergency department (ED) to seek care and manage symptoms related to their disease. Many people with SCD have reported unique barriers and challenges, such as long wait times and lack of provider knowledge related to SCD, when seeking treatment in emergency care settings.
The Centers for Disease Control and Prevention (CDC) and the American College of Emergency Physicians (ACEP) held a webinar June 16, 2022, for healthcare providers, policymakers, and SCD advocates that explored the intersection of SCD and emergency care.
If you weren’t able to participate in the webinar on June 16, you can access it here now. The webinar is free and approximately 1 hour long. Please share the webinar link with colleagues, fellow providers, and hospital administrators.
You can also use this toolkit to find more resources from ACEP and CDC on how to improve treatment for people with SCD who visit emergency care settings.
Share the graphics and sample messages to spread the word about this important webinar through your professional networks.
Related Resources
For Providers
- Managing Sickle Cell Disease in the ED: This ACEP resource provides strategies for effectively treating pain in the ED.
- 3 Tips About Sickle Cell Disease Every Emergency Provider Needs to Know: Get tips from CDC on how you can improve the experiences people with SCD have when seeking care in the ED.
For People with SCD
- Tips for Receiving Better Care in the ED for Sickle Cell Disease: Do you use the ED for care of SCD? Check out this CDC fact sheet to learn what you need to know before you go.
Sample Messages
Use the sample social media graphics and messages below to share the webinar, highlight voices of people with SCD, and share SCD trivia and facts. Right click on an image and select “Save as …” to download and share.
Share the Webinar
Interested in applying new strategies to break down barriers for people w/ #SickleCellDisease (SCD)? View a webinar cosponsored by CDC and the American College of Emergency Physicians (@ACEPNow) that will improve care in emergency departments (ED). Hear stories from people with SCD and family members of people with SCD. Watch now: https://bit.ly/3TguYTQ #SCDintheED
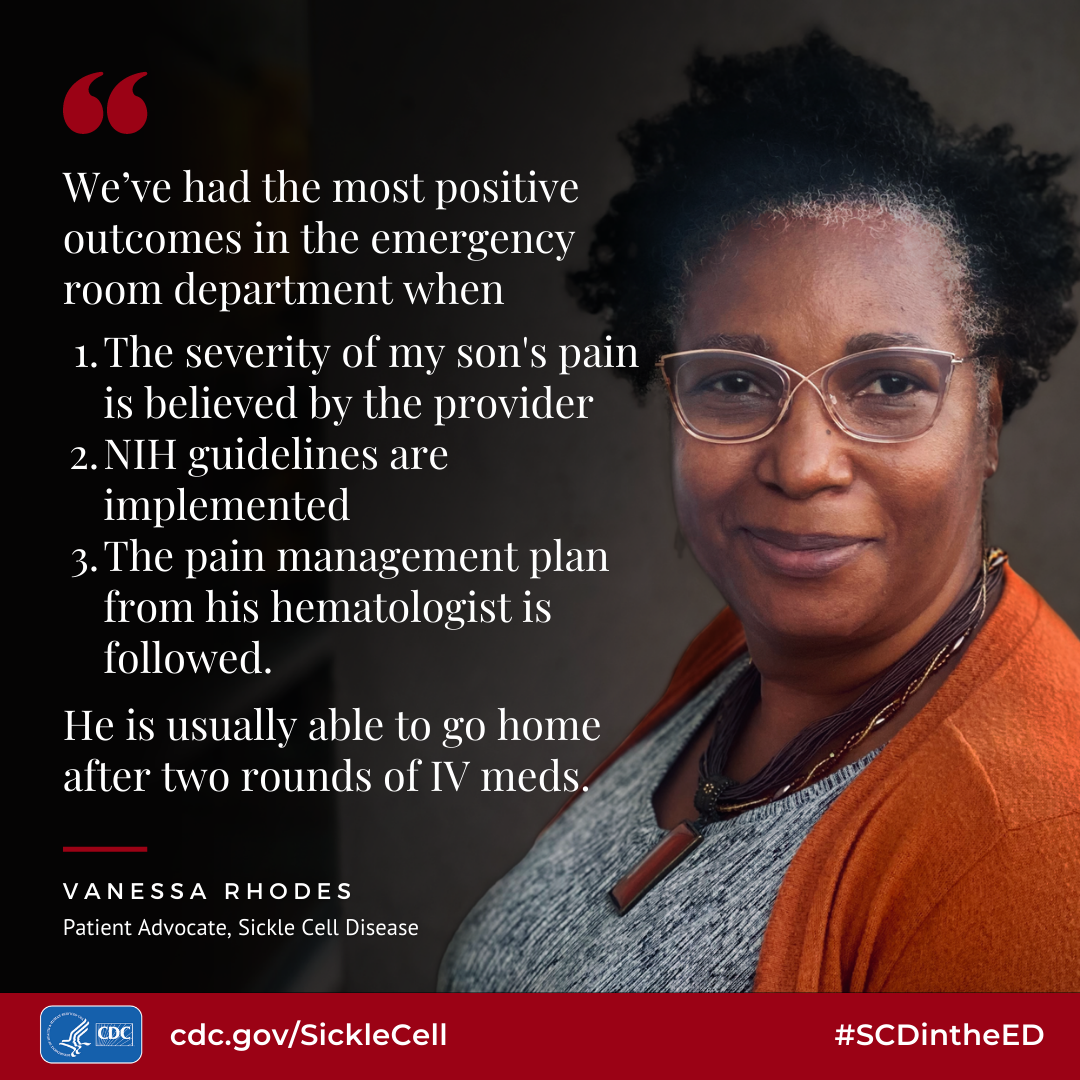
Highlight Voices of People with SCD
Clayton, who has #SickleCellDisease, shares the challenges he has faced at the emergency department (ED). Hear from him and others in a webinar hosted by CDC and the American College of Emergency Physicians (@ACEPNow): https://bit.ly/3TguYTQ #SCDintheED
![When I have go to the emergency department for treatment, I feel anxiety and preemptive frustration in anticipation of the possible foolishness I mav encounter from the medical staff: Will they take me seriously? Will they accuse me of (drug] seeking? How long before I receive the treatment I need? Will it be the correct dosage, or will they low-ball me? - Clayton Andrews, Patient Advocate, Sickle Cell Disease](./index_html_files/scd-ed-care-quote-Clayton-Andrews.png)
Vanessa shares her story of advocating to get her son prompt and quality care for #SickleCellDisease in the emergency department (ED) with the hope of improving care and helping others. Watch now: @ACEPNow: https://bit.ly/3TguYTQ #SCDintheED
Andre, who lost his son with #SickleCellDisease, shares his perspective on the challenges patients and their families face in receiving care in the emergency department (ED). Hear from him and others in a free webinar hosted by CDC and the American College of Emergency Physicians (@ACEPNow): https://bit.ly/3TguYTQ #SCDintheED
Learn from Nilda’s experiences facing barriers to care as a person with #SickleCellDisease (SCD) in the emergency department (ED) and what strategies can improve care in a free webinar by CDC and the American College of Emergency Physicians (@ACEPNow): https://bit.ly/3TguYTQ #SCDintheED
Morica shares her ideal care experience when coming into the emergency department (ED) for a sickle cell crisis. Get more tips on providing better care for people with #SickleCellDisease on a webinar hosted by CDC and the American College of Emergency Physicians (@ACEPNow). Watch now: https://bit.ly/3TguYTQ #SCDintheED
Blaze shares one change he would like to see in emergency care for people with #SickleCellDisease (SCD). To hear more insights from people with SCD, watch a free webinar hosted by CDC and the American College of Emergency Physicians (@ACEPNow): https://bit.ly/3TguYTQ #SCDintheED

If I could change one thing about the care provided to people with sickle cell disease in the emergency department (ED), it would be “timeliness.” Sickle cell disease is a serious disorder and patients in the ED are going through extreme pain. Patients can wait hours before they are even taken back to triage. According to the National Institutes of Health’s evidence-based guidelines, a patient should receive medication within an hour of registration and 30 minutes of triage. Even though these guidelines exist that is not the case for myself or my peers living with this blood disorder. Last year I even made a petition to bring more attention to this problem and create change. The petition can be found below. bit.ly/38auo7M
Blaze Eppinger
Patient Advocate, Sickle Cell Disease
#SCDintheED
The Arrington family shares how emergency providers can give parents of children with #SickleCellDisease (SCD) peace of mind and confidence when seeking care. Watch a webinar hosted by CDC and the American College of Emergency Physicians (@ACEPNow) for more information on providing patient-centered emergency department (ED) care for people of all ages with SCD: https://bit.ly/3TguYTQ #SCDintheED

If we could change one thing about the care provided to people with sickle cell disease (SCD) in the emergency department (ED), it would be to have all ED staff implement the Clinical Practice Guidelines for Treating Acute and Chronic Pain for SCD as outlined by the American Society of Hematology. When taking our 8-year-old daughter for emergency care, we never know what to expect, which makes us anxious and reluctant to seek care at an ED. A pediatric patient (or any patient with SCD) having a severe pain crisis should not have to wait two hours for pain-relieving medication, which is something we have dealt with in past situations. Implementing the standard Clinical Practice Guidelines would ensure that the patient has their pain assessed and medication administered within one hour of arrival at the ED. The parents and patient would have this tool as reassurance that they will receive care within a timely manner. Every patient and parent should have peace of mind and confidence in the emergency care available to them.
Chanel and Carsyn Arrington
Patient Advocates, Sickle Cell Disease
#SCDintheED
Lukhan emphasizes the importance of prompt treatment with IV fluids and pain medication for people who seek care in the emergency department (ED) for a sickle cell crisis. Watch a webinar hosted by CDC and the American College of Emergency Physicians (@ACEPNow), to learn more tips on improving ED care for people with #SickleCellDisease: https://bit.ly/3TguYTQ #SCDintheED

If I could change one thing about the care provided to people with sickle cell disease in the emergency department, it would be to bring on the IV fluids! It’s bad enough that we have to wait several hours; at least start an IV in the waiting room to begin fluids. We get severely dehydrated, and our pain increases and oxygen supply is limited to vital organs. If we could just get the IV fluids it will help us so that when we do get into a room, the pain medicines will work quicker because our pain won’t be as severe.
Lukhan Cooper
Patient Advocate, Sickle Cell Disease
#SCDintheED
Share Trivia and Facts
Emergency providers can improve care for people with #SickleCellDisease by treating their pain promptly. Learn more: https://bit.ly/3TguYTQ #SCDintheED
True or false
When a patient requests pain medication during a sickle cell crisis, providers should conduct tests to confirm their diagnosis.
False.
Requests for pain medicines are most commonly due to past experience, not drug-seeking behavior.
Did you know?
Excruciating pain is the most common reason for ED visits in people with sickle cell disease.
Build trust by believing your patients are in pain. Provide pain medication within 60 minutes of arrival.
#SCDintheED
The pain experienced by people with #SickleCellDisease (SCD) can be severe. Healthcare providers working in emergency care settings should ensure prompt pain relief when people with SCD seek treatment. Learn more: https://bit.ly/3TguYTQ #SCDintheED
Poll
What is the best way to confirm a sickle cell pain crisis?
A. Vital signs are abnormal
B. Lab tests show low hemoglobin levels
C. Patient report of pain
Answer: C. Patient report of pain is the gold standard
There are no vital sign changes or lab values that confirm or rule-out a sickle cell pain crisis.
Did you know?
People with sickle cell disease experience longer wait times on average than other patients.
Many people with sickle cell disease avoid or delay care due to bad experiences in the ED.
Treat sickle cell pain promptly. Do not delay pain relief while other tests are performed
#SCDintheED
#DYK: #SickleCellDisease can affect people from a variety of racial and ethnic backgrounds. Providers can make sure all people are properly diagnosed and treated. https://bit.ly/3TguYTQ #SCDintheED
Fact or myth?
Sickle cell disease only affects African Americans.
Myth
Sickle cell disease affects millions of people throughout the world.
The misunderstanding that sickle cell disease only affects African Americans may lead to delays in treatment for some patients.
Providers should know that sickle cell disease affects diverse groups so that all people can be properly diagnosed and treated.
#SCDintheED
People with #SickleCellDisease visit the emergency department (ED) often because of pain related to their condition. Learn how healthcare providers in emergency care settings can ensure people with sickle cell disease receive timely services that meet their needs. https://bit.ly/3TguYTQ #SCDintheED
Did you know?
How often do people with sickle cell disease seek care in the ED?
Poll
Average yearly ED visits among adults with sickle cell disease
A. One
B. Two
C. Three
D. Four
Answer: C. Three
Adults with sickle cell disease seek care in the ED an average of three times a year.
Make sure patients’ pain management plans are available in the EMR, especially those with frequent ED use.
#SCDintheED