Vital Signs: Making Health Care Safer
Stop Infections from Lethal CRE Germs Now
March 2013



4% & 18%
About 4% of US hospitals had at least one patient with a CRE (carbapenem-resistant Enterobacteriaceae) infection during the first half of 2012. About 18% of long-term acute care hospitals* had one.

42
One type of CRE infection has been reported in medical facilities in 42 states during the last 10 years.

1 in 2
CRE germs kill up to half of patients who get bloodstream infections from them.
Untreatable and hard-to-treat infections from CRE germs are on the rise among patients in medical facilities. CRE germs have become resistant to all or nearly all the antibiotics we have today. Types of CRE include KPC and NDM. By following CDC guidelines, we can halt CRE infections before they become widespread in hospitals and other medical facilities and potentially spread to otherwise healthy people outside of medical facilities.
Health Care Providers can
- Know if patients in your facility have CRE.
- Request immediate alerts when the lab identifies CRE.
- Alert the receiving facility when a patient with CRE transfers, and find out when a patient with CRE transfers into your facility.
- Protect your patients from CRE.
- Follow contact precautions and hand hygiene recommendations when treating patients with CRE.
- Dedicate rooms, staff, and equipment to patients with CRE.
- Prescribe antibiotics wisely.
- Remove temporary medical devices such as catheters and ventilators from patients as soon as possible.
*Long-term acute care hospitals provide complex medical care, such as ventilation or wound care, for long periods of time.
Action is needed now to stop these deadly infections.
CRE germs have found ways to beat antibiotics.
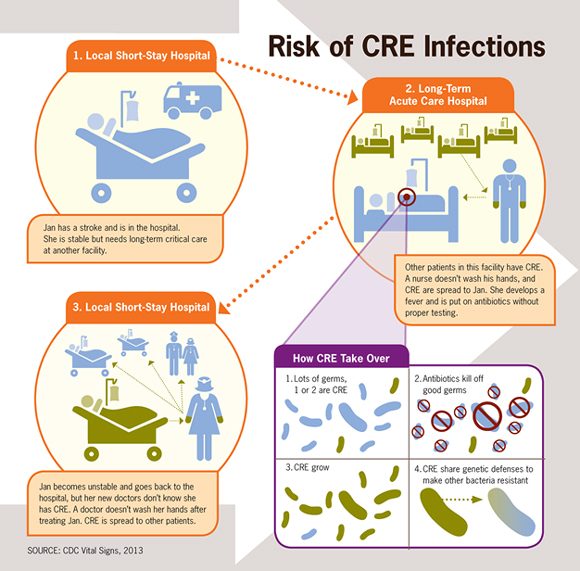
- CRE infections are caused by a family of germs that are a normal part of a person’s healthy digestive system. These germs can cause infections when they get into the bladder, blood, or other areas where germs don’t belong.
- Some of these germs have become resistant to all or almost all antibiotics, including last-resort drugs called carbapenems. These resistant germs are called CRE.
- Almost all CRE infections happen to patients receiving serious medical care. CRE infections are hard to treat, and in some cases, untreatable. CRE kill up to half of patients who get bloodstream infections from them.
- In addition to spreading among people, CRE easily spread their antibiotic resistance to other kinds of germs, making those potentially untreatable as well.
CRE infections are spreading, and urgent action is needed to stop them.
- Although CRE germs are not very common, they have increased from 1% to 4% in the past decade. One type of CRE has increased from 2% to 10%.
- CRE are more common in some US regions, such as the Northeast, but 42 states report having had at least one patient test positive for one type of CRE.
- About 18% of long-term acute care hospitals and about 4% of short-stay hospitals in the US had at least one CRE infection during the first half of 2012.
- CRE’s ability to spread themselves and their resistance raises the concern that potentially untreatable infections could appear in otherwise healthy people.
CRE infections can be prevented.
- Medical facilities in several states have reduced CRE infection rates by following CDC’s prevention guidelines (see box).
- Israel decreased CRE infection rates in all 27 of its hospitals by more than 70% in one year with a coordinated prevention program.
- The US is at a critical time in which CRE infections could be controlled if addressed in a rapid, coordinated, and consistent effort by doctors, nurses, lab staff, medical facility leadership, health departments/states, policy makers, and the federal government.

Colorado Department of Public Health and Environment
- Colorado requires laboratories to report CRE and actively tracks the germs’ presence.
- CDC, Colorado, and several facilities implemented CDC recommendations to control an outbreak of CRE.
- Result: The outbreak was stopped.

Colorado Department of Public Health and Environment
- Colorado requires laboratories to report CRE and actively tracks the germs’ presence.
- CDC, Colorado, and several facilities implemented CDC recommendations to control an outbreak of CRE.
- Result: The outbreak was stopped.

Florida Department of Health
- CDC worked with Florida to stop a year-long CRE outbreak in a long-term acute care hospital.
- Improved use of CDC recommendations such as educating staff; dedicating staff, rooms, and equipment to patients with CRE; and improving use of gloves and gowns.
- Result: The percentage of patients who got CRE at the facility dropped from 44% to 0.

Florida Department of Health
- CDC worked with Florida to stop a year-long CRE outbreak in a long-term acute care hospital.
- Improved use of CDC recommendations such as educating staff; dedicating staff, rooms, and equipment to patients with CRE; and improving use of gloves and gowns.
- Result: The percentage of patients who got CRE at the facility dropped from 44% to 0.
Federal Government is
- Monitoring the presence of and risk factors for CRE infections through the National Healthcare Safety Network (NHSN) and Emerging Infections Program (EIP).
- Providing CRE outbreak support such as staff expertise, prevention guidelines, tools, and lab testing to states and facilities.
- Developing detection methods and prevention programs to control CRE. CDC’s “Detect and Protect” effort supports regional CRE programs.
- Helping medical facilities improve antibiotic prescribing practices.
States and Communities can
- Know CRE trends in your region.
- Coordinate regional CRE tracking and control efforts in areas with CRE. Areas not yet or rarely affected by CRE infections can be proactive in CRE prevention efforts.
- Require facilities to alert each other when transferring patients with any infection.
- Consider including CRE infections on your state’s Notifiable Diseases list.
Health Care CEOs/Medical Officers can
- Require and strictly enforce CDC guidance for CRE detection, prevention, tracking, and reporting.
- Make sure your lab can accurately identify CRE and alert clinical and infection prevention staff when these germs are present.
- Know CRE trends in your facility and in the facilities around you.
- When transferring a patient, require staff to notify the other facility about infections, including CRE.
- Join or start regional CRE prevention efforts, and promote wise antibiotic use.
Health Care Providers can
- Know if patients with CRE are hospitalized at your facility, and stay aware of CRE infection rates. Ask if your patients have received medical care somewhere else, including another country.
- Follow infection control recommendations with every patient, using contact precautions for patients with CRE. Whenever possible, dedicate rooms, equipment, and staff to CRE patients.
- Prescribe antibiotics wisely. Use culture results to modify prescriptions if needed.
- Remove temporary medical devices as soon as possible.
Patients can
- Tell your doctor if you have been hospitalized in another facility or country.
- Take antibiotics only as prescribed.
- Insist that everyone wash their hands before touching you.
- Vital Signs Issue details: Carbapenem-Resistant Enterobacteriaceae Morbidity and Mortality Weekly Report (MMWR)
- CDC Feature- Patients Face More Untreatable Infections from CRE
- Vital Signs – Making Health Care Safer [PODCAST – 0:60 seconds]
- Making Health Care Safer [PSA – 0:60 seconds]
- Vital Signs – SPANISH (Making Health Care Safer) [PODCAST – 0:60 seconds]
- Carbapenem-resistant Enterobacteriaceae (CRE)
- 2012 CRE Toolkit – Guidance for Control of Carbapenem-resistant Enterobacteriaceae (CRE)
- Get Smart for Healthcare
- Hand Hygiene in Healthcare Settings
- National Healthcare Safety Network
- Safe Healthcare Blog Discussions on CRE
- Healthcare-Associated Infections
- New Carbapenem-Resistant Enterobacteriaceae Warrant Additional Action by Healthcare Providers
CDC on Medscape
- Vital Signs Issue details: Carbapenem-Resistant Enterobacteriaceae Morbidity and Mortality Weekly Report (MMWR)
- CDC Feature- Patients Face More Untreatable Infections from CRE
- Vital Signs – Making Health Care Safer [PODCAST – 0:60 seconds]
- Making Health Care Safer [PSA – 0:60 seconds]
- Vital Signs – SPANISH (Making Health Care Safer) [PODCAST – 0:60 seconds]
- Carbapenem-resistant Enterobacteriaceae (CRE)
- 2012 CRE Toolkit – Guidance for Control of Carbapenem-resistant Enterobacteriaceae (CRE)
- Get Smart for Healthcare
- Hand Hygiene in Healthcare Settings
- National Healthcare Safety Network
- Healthcare-Associated Infections
- New Carbapenem-Resistant Enterobacteriaceae Warrant Additional Action by Healthcare Providers
