Recommendations for Fully Vaccinated People
COVID-19 Homepage
COVIDView Summary ending on April 4, 2020
This CDC report provides a weekly summary and interpretation of key indicators that have been adapted to track the COVID-19 pandemic in the United States. While influenza-like-illness (ILI) declined, it is still elevated and laboratory confirmed COVID-19 activity continues to increase as do COVID-19 severity indicators (hospitalizations and deaths).
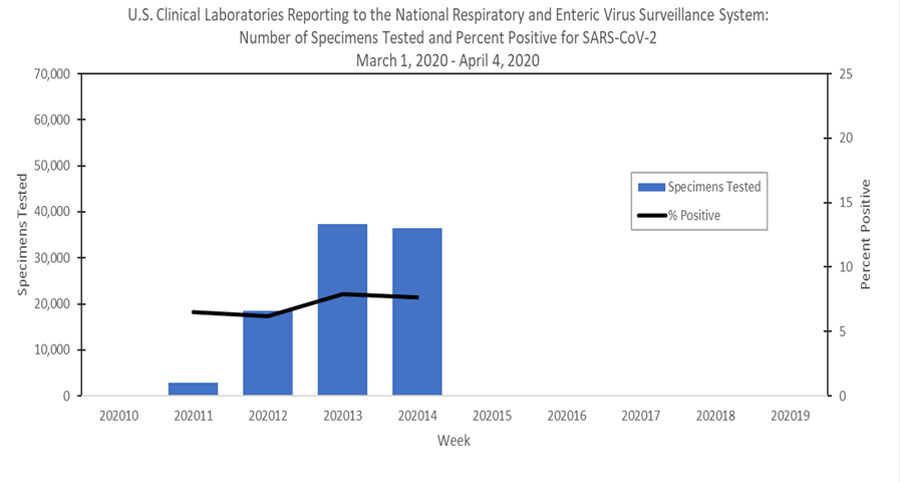
Public health, commercial and clinical laboratories are all testing for SARS-CoV-2 and reporting their results. The national percentage of respiratory specimens testing positive for SARS-CoV-2 is increasing overall and for week 14 is distributed as follows:
- 18.5% at public health laboratories, and
- 7.7% at clinical laboratories.
Since the start of the outbreak, 17.6 % of specimens tested at commercial laboratories have been positive for SARS-CoV-2.
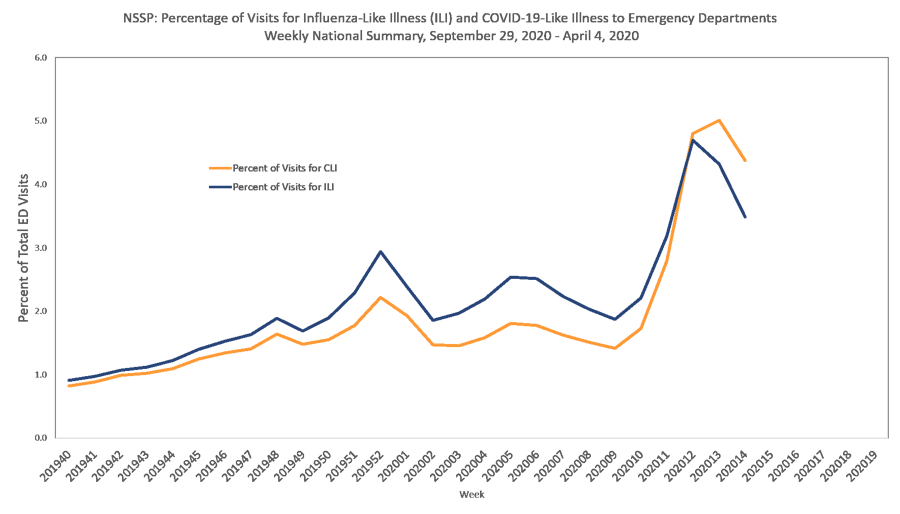
Two indicators from existing surveillance systems are being monitored to track outpatient or emergency department (ED) visits for potential COVID-19 illness.
- Nationally, the percentages of visits for influenza-like illness (ILI) and COVID-19-like illness (CLI) are elevated compared to what is normally seen at this time but decreased compared to last week.
Recent changes in health care seeking behavior are likely impacting both networks, making it difficult to draw further conclusions at this time. Tracking these systems moving forward will give additional insight into illness related to COVID-19.
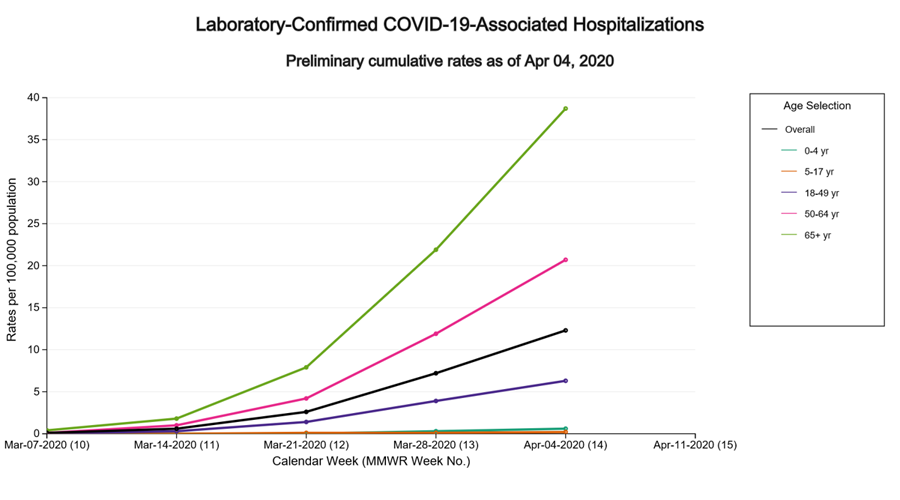
Cumulative COVID-19-associated hospitalization rates since March 1, 2020, will be updated weekly. The overall cumulative hospitalization rate is 12.3 per 100,000, with the highest rates in persons 65 years and older (38.7 per 100,000) and 50-64 years (20.7 per 100,000).
Based on death certificate data, the percentage of deaths attributed to COVID-19 increased from 4.0% during week 13 to 6.9% during week 14. The percentage of deaths due to pneumonia (excluding COVID-19 or influenza) decreased from 7.5% during week 13 to 7.2% during week 14.
All data are preliminary and may change as more reports are received.
A description of the surveillance systems summarized in COVIDView, including methodology and detailed descriptions of each data component, is available on the surveillance methods page.
- CDC is modifying existing surveillance systems, many used to track influenza and other respiratory viruses annually, to track COVID-19.
- Nationally, the percentage of laboratory specimens testing positive for SARS-CoV-2 continued to increase.
- Visits to outpatient providers and emergency departments (EDs) for illnesses with symptoms consistent with COVID-19 are elevated compared to what is normally seen at this time of year but decreased compared to levels reported last week. At this time, there is little influenza virus circulation so the elevated proportion of people presenting with these symptoms is likely due to COVID-19, but may be tempered by a number of factors including less ILI overall because of widespread adoption of social distancing efforts as well as changes in healthcare seeking practices.
- The overall cumulative COVID-19 associated hospitalization rate is 12.3 per 100,000, with the highest rates in persons 65 years and older (38.7 per 100,000) and 50-64 years (20.7 per 100,000). Hospitalization rates for COVID-19 in older people are higher than what is typically seen early in a flu season.
- Based on death certificate data, the percentage of deaths attributed to COVID-19 increased from 4.0% during week 13 to 6.9% during week 14. The percentage of deaths due to pneumonia (excluding COVID-19 or influenza) decreased from 7.5% during week 13 to 7.2% during week 14.
The number of specimens tested for SARS-CoV-2 and reported to CDC by public health laboratories and a subset of clinical and commercial laboratories in the United States are summarized below. At this point in the outbreak, all laboratories are performing primary diagnostic functions; therefore, the percentage of specimens testing positive across laboratory types can be used to monitor trends in COVID-19 activity. As the outbreak progresses, it is possible that different types of laboratories will take on different roles, and the data interpretation may need to be modified. The lower percentage of specimens testing positive in the clinical laboratories compared to the public health and commercial laboratories is likely due to the amount of COVID-19 activity in areas with reporting laboratories and a larger proportion of specimens from children.
| Week 14 (March 29 – April 4, 2020) |
Cumulative since March 1, 2020 | |
|---|---|---|
| No. of specimens tested | 102,385 | 1,562,201 |
| Public Health Laboratories | 65,917 | 225,850 |
| Clinical Laboratories | 36,468 | 95,137 |
| Commercial Laboratories | 1,241,214 | |
| No. of positive specimens | 14,975 (14.6%) | 257,986 (16.5%) |
| Public Health Laboratories | 12,177 (18.5%) | 32,437 (14.4%) |
| Clinical Laboratories | 2,798 (7.7%) | 7,095 (7.5%) |
| Commercial Laboratories | 218,454 (17.6%) |
* Commercial and clinical laboratory data represents select laboratories and does not capture all tests performed in the United States.
Public Health Laboratories
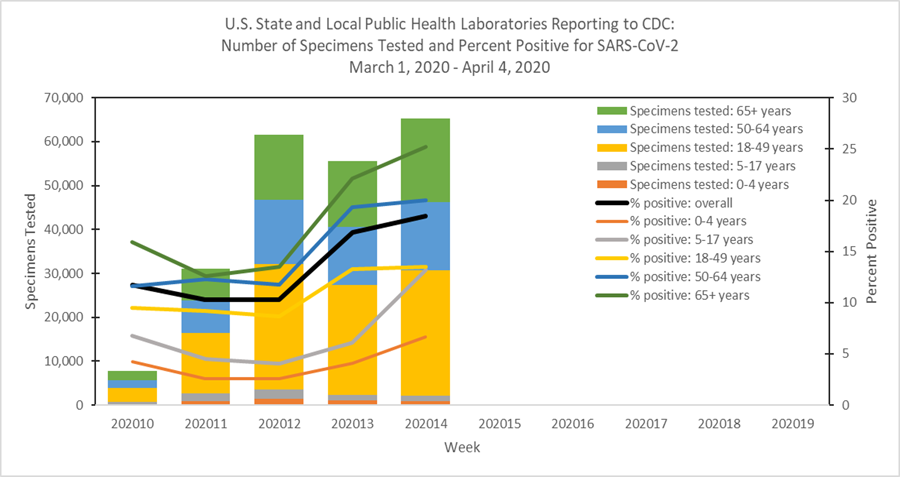
Clinical Laboratories
Additional virologic surveillance information: Surveillance Methods
Two syndromic surveillance systems are being used to monitor trends in outpatient and emergency department visits that may be related to COVID-19. Each system monitors a slightly different syndrome, and together these systems provide a more comprehensive picture of mild to moderate COVID-19 illness than either would individually. Both systems are currently being affected by recent changes in health care seeking behavior, including increasing use of telemedicine and recommendations to limit emergency department (ED) visits to severe illness, as well as increased social distancing. These changes affect the numbers of people and their reasons for seeking care in the outpatient and ED settings.
ILINet
The U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet) provides data on visits for influenza-like illness (ILI) (fever [≥100○F] and cough and/or sore throat) to approximately 2,600 primary care providers, emergency departments and urgent care centers in all 50 states, Puerto Rico, the District of Columbia and the U.S. Virgin Islands. Mild COVID-19 illness presents with symptoms similar to ILI, so ILINet is being used to track trends of mild COVID-19 illness and allows for comparison with prior influenza seasons.
Nationwide during week 14, 3.9% of patient visits reported through ILINet were due to ILI. This percentage is above the national baseline of 2.4%, but represents the second week of a decline after three weeks of increase beginning in early March. The percentage of visits for ILI decreased in all age groups. Nationally, laboratory confirmed influenza activity as reported by clinical laboratories decreased to levels usually seen in summer months which, along with changes in healthcare seeking behavior and the impact of social distancing, is likely driving the decrease in ILI activity.
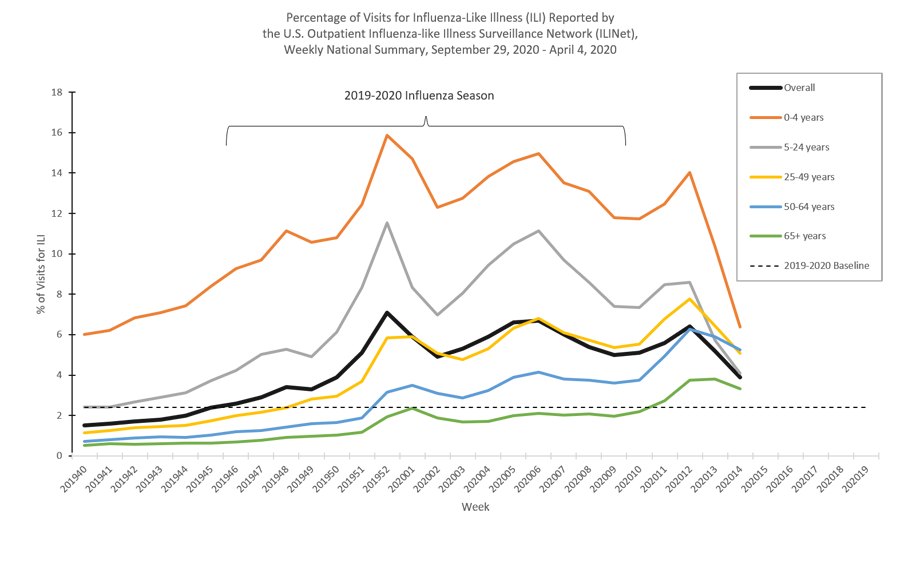
* Age-group specific percentages should not be compared to the national baseline.
On a regional levelExternal, the percentage of outpatient visits for ILI ranged from 2.4% to 10.0% during week 14; all regions reported a decreased percentage of outpatient visits for ILI compared to week 13 but remained above their regions-specific baselines.
ILI Activity Levels
Data collected in ILINet are used to produce a measure of ILI activity for all 50 states, Puerto Rico, the District of Columbia and New York City. The mean reported percentage of visits due to ILI for the current week is compared to the mean reported during non-influenza weeks, and the activity levels correspond to the number of standard deviations below, at or above the mean.
The number of jurisdictions at each activity level during week 14 and the change compared to the previous week are summarized in the table below and shown in the following maps. The decreasing percentage of visits for ILI described above are reflected in this week’s ILI activity levels.
| Activity Level | Number of Jurisdictions | |
| Week 14 (Week ending April 4, 2020) | Compared to Previous Week | |
| Very High | 8 | -6 |
| High | 13 | -4 |
| Moderate | 4 | -1 |
| Low | 12 | +5 |
| Minimal | 16 | +6 |
| Insufficient Data* | 1 | No change |
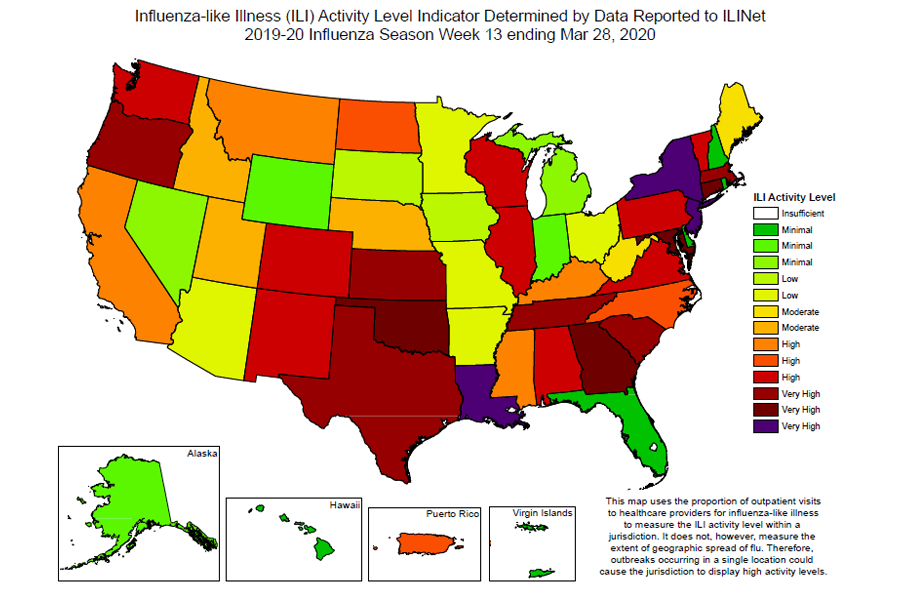
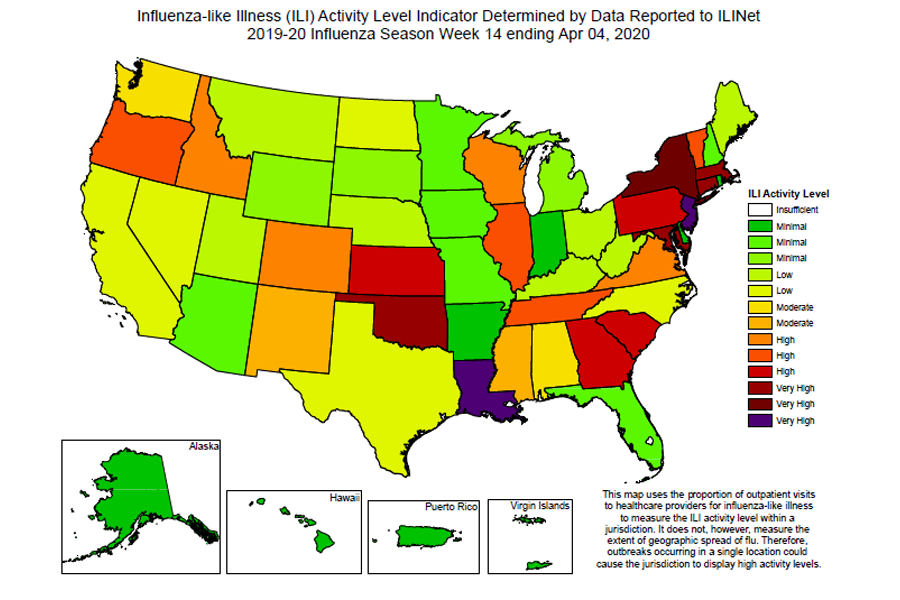
The “very high” activity level was recently developed and will be reflected in other postings of the ILINet activity map when the map is updated on April 17, 2020.
National Syndromic Surveillance Program (NSSP): Emergency Department (ED) Visits
NSSP is a collaboration among CDC, federal partners, local and state health departments, and academic and private sector partners to collect, analyze and share electronic patient encounter data received from multiple health care settings. To track trends of potential COVID-19 visits, visits for COVID-19-like illness (CLI) (fever and cough or shortness of breath or difficulty breathing) and ILI to a subset of emergency departments in 47 states are being monitored.
Nationwide during week 14, 4.4% of emergency department visits captured in NSSP were due to CLI and 3.5% were due to ILI. This is the second week of decline in percentage of visits for ILI and the first week of decline in percentage of visits for CLI. All 10 HHS regionsExternal experienced a decline in percentage of visits for ILI and CLI.
Additional information about medically attended outpatient and emergency department visits for ILI and CLI: Surveillance Methods
The COVID-19-Associated Hospitalization Surveillance Network (COVID-NET) conducts population-based surveillance for laboratory-confirmed COVID-19-associated hospitalizations in select counties participating in the Emerging Infections Program (EIP) and Influenza Hospitalization Surveillance Project (IHSP) states. COVID-NET-estimated hospitalization rates will be updated weekly.
A total of 4,001 laboratory-confirmed COVID-19-associated hospitalizations were reported by COVID-NET sites between March 1, 2020, and April 4, 2020. The overall cumulative hospitalization rate was 12.3 per 100,000 population, with the highest rates in those aged 65 years and older (38.7 per 100,000) followed by adults aged 50-64 years (20.7 per 100,000).
Additional hospitalization surveillance information: Surveillance Methods | COVID-Net interactive data
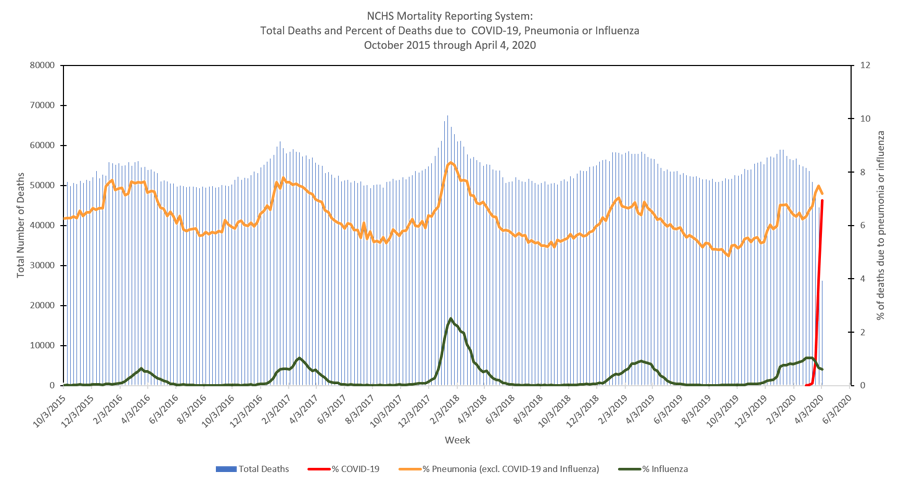
The National Center for Health Statistics (NCHS) collects death certificate data from vital statistics offices for all deaths occurring in the United States. Based on death certificate data available on April 9, 2020, 6.9% of all deaths occurring during the week ending April 4, 2020 (week 14) had COVID-19 listed as a cause of death, 7.2% had pneumonia (excluding deaths involving COVID-19 or influenza) listed as a cause of death, and 0.6% had influenza listed as a cause of death. The weekly percentage of deaths due to COVID-19 has increased each week since the start of the COVID-19 outbreak in the United States. The percentage of deaths due to pneumonia (excluding deaths involving COVID-19 or influenza) decreased during week 14 compared to week 13.
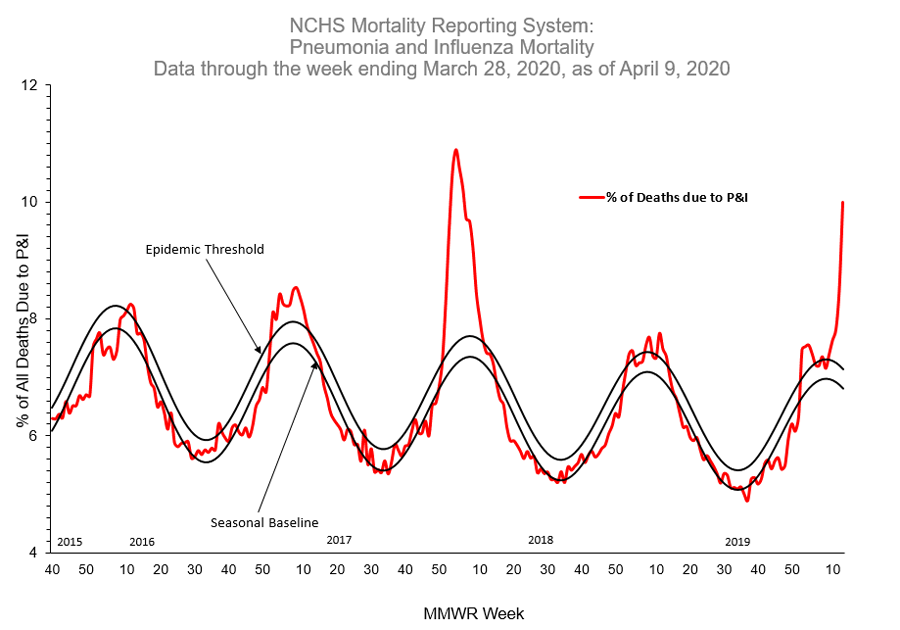
NCHS data are also used to monitor the percentage of death occurring in a given week that had pneumonia and/or influenza (P&I) listed as a cause of death. When the percentage of P&I deaths exceeds the epidemic threshold, that indicates that significantly more P&I deaths occurred than would be expected at that time of year. During the most recent week for which these data are available (week ending March 28, 2020), 10.0% of deaths were due to P&I. This percentage is above the epidemic threshold of 7.1% for that week. The increase in P&I percentage is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19.
Additional NCHS mortality surveillance information: Surveillance Methods | Provisional Death Counts for COVID-19