Diabetes and COVID-19
‹View Table of Contents

The ongoing COVID-19 pandemic has further underscored the importance of type 2 diabetes prevention and diabetes management. Adults with some underlying medical conditions, such as cancer, heart conditions, chronic lung diseases, and diabetes, are more likely than others to become severely ill if infected with COVID-19.29 As a result, they are more likely to need hospitalization, be admitted into an intensive care unit, need a ventilator to help them breathe, or die.30
Early surveillance data reported to CDC from January to May 2020 indicated that COVID-19 hospitalizations were 6 times higher and deaths 12 times higher for people with COVID-19 and an underlying medical condition such as diabetes, heart disease, or chronic lung disease.31 Other factors, such as increased age, a larger number of underlying medical conditions, and lower socioeconomic position, can further increase a person’s risk of severe illness.29
Evidence collected since the beginning of the pandemic shows that:
- Patients hospitalized with COVID-19 were more likely to be readmitted to the same hospital within 2 months of discharge if they had certain chronic conditions, such as diabetes or chronic kidney disease.32
- Among patients hospitalized with severe COVID-19 complications, 39.7% also had diabetes as an underlying medical condition. The percentage increased to 46.5% for patients 50 to 64.11
- People younger than 18 with COVID-19 were up to 2.5 times more likely to be newly diagnosed with diabetes in the months after infection than those without COVID-19 and those who had other respiratory infections before the pandemic.33
- During the pandemic, CDC worked with state health departments to expand the use of telehealth, text, and video chats with diabetes care and education specialists. These efforts helped ensure that patients got the diabetes management services they needed when in-person visits were not possible.
- CDC helped develop systems to collect data on comorbidities related to COVID-19. The agency also shared the latest science and data on COVID-19 and diabetes with clinicians, partners, and the public.
- CDC provided guidance and resources to allow the National DPP lifestyle change program to be delivered virtually instead of in person. Most organizations that deliver the program have made the transition to virtual classes.34
Medical Service Usage
It is crucial for people who experience any life-threatening conditions to seek immediate emergency care, even during rare events like the COVID-19 pandemic. For people with diabetes, that may mean going to an emergency department for help to prevent uncontrolled high blood sugar or other serious complications. A lack of blood sugar management and other self-management routines, even for a short time, can have lasting negative consequences for people with diabetes.
The COVID-19 pandemic affected how often people accessed emergency services. One study found that emergency department visits declined 42% during the early weeks of the COVID-19 pandemic.35 Another study found a 10% decline in visits for hyperglycemic crisis during the first 10 weeks of the pandemic.36
People with diabetes were also less likely to use the regular services they needed to manage their condition during the pandemic. In particular, young adults 18 to 29 reported the largest disruption in access to and use of medical care, including difficulty getting diabetes medications. This age group also reported low engagement in COVID-19 prevention methods, including intention to get vaccinated.37

Health Disparities
The COVID-19 pandemic highlighted the persistent problem of health disparities for some populations.38 For example, some racial and ethnic minority groups are at higher risk of severe complications from COVID-19 because of higher rates of diabetes, heart disease, and other underlying conditions. Hospitalization rates associated with COVID-19 are highest among American Indian, non-Hispanic Black, and Hispanic populations.39
Figure 10 highlights the racial and ethnic disparities of hospitalizations associated with COVID-19 since the pandemic started. These rates are similar to the racial and ethnic disparities among people diagnosed with diabetes (Figure 4). These groups also have higher rates of obesity, which is a primary risk factor for type 2 diabetes.
Figure 10. Cumulative Laboratory-Confirmed Hospitalizations Associated With COVID-19, by US Racial or Ethnic Group, March 2020–May 14, 2022
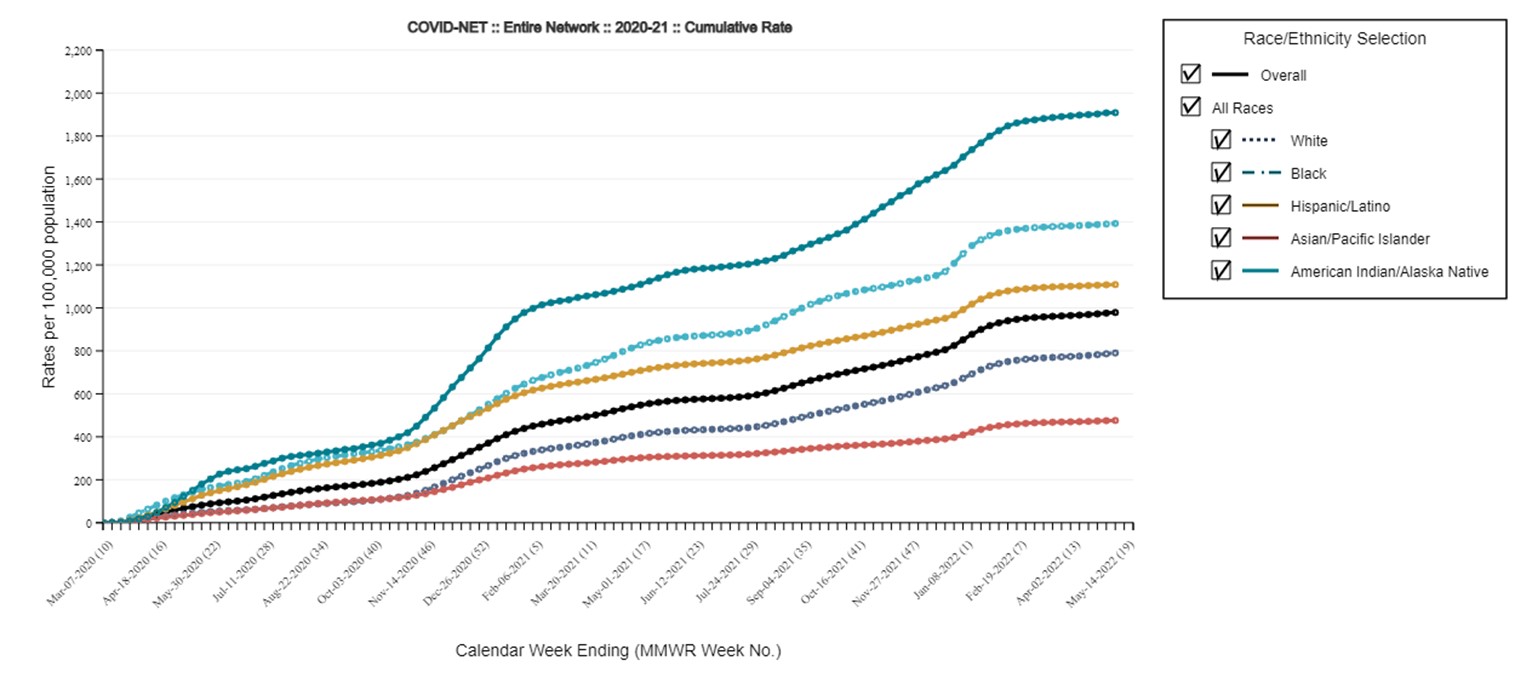
Notes: Figure is adapted from CDC’s Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET), weekly summary of U.S. COVID-19 Hospitalization Data. This figure is a cumulative rate of COVID-19 hospitalization by racial and ethnicity. The Morbidity and Mortality Weekly Report (MMWR) week is the week of the year that local or state health departments use for disease incidence reporting and publishing.
Data source: Laboratory-Confirmed COVID-19-Associated Hospitalizations, COVID NET, Centers for Disease Control and Prevention.