Technology and Innovation
Smartphones Connect Disease Data Faster
Credit: David Snyder, CDC Foundation.
Across the globe, CDC experts are using smartphones to find and stop outbreaks at their source.
In Thailand, a CDC-developed smartphone app allows people who work with poultry and swine to report human and animal sicknesses or deaths with the click of a few buttons. In Kenya, CDC helped roll out a new mobile app that enables veterinary practitioners to enter, transmit, and analyze surveillance data from the palm of their hand. Health workers in Sierra Leone are using a smartphone app to report critical health information to the country’s CDC-supported surveillance network. With technical assistance from CDC, Zambia was the first country to conduct a new mobile phone survey to track noncommunicable diseases and related risk factors using adaptable, open-source technology. In Guatemala, smartphones are being used to track potential outbreaks of flu by having users report influenza-like symptoms using a smartphone app created by CDC.
The real-time use of data collected through these apps has led to several successful outbreak investigations, helping to contain diseases before they spiral into epidemics. The successes in these countries can serve as a model for other countries on how to harness the power of technology to detect disease outbreaks faster.
Innovation in the Field: The Measles-Rubella Box

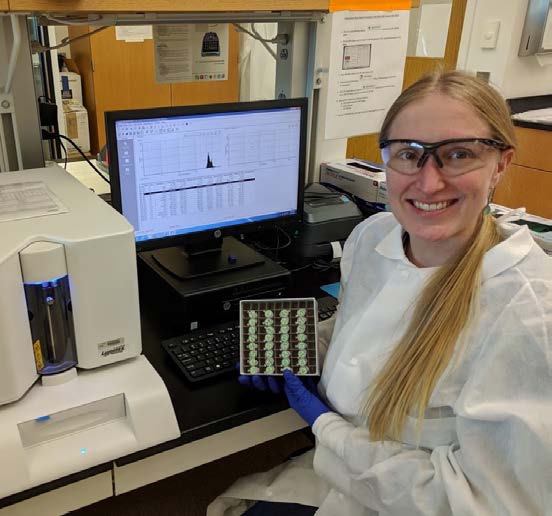
Dr. Aimee Summers preparing whole blood samples for DMF-ELISA at a Health Center in Biyela, Kinshasa Province, DRC. Credit: Alaine Knipes.
Since 2016, CDC has been testing an innovative new technology, the Measles-Rubella Box (MR Box). The technology, developed by scientists from the University of Toronto, has the potential to confirm active measles and rubella infections in the field to help stop outbreaks faster.
In the Democratic Republic of the Congo (DRC), measles and rubella tests have to be sent to the national laboratory in the capital of Kinshasa. DRC is a large country, and transporting blood samples can be difficult. Even the fastest results take a minimum of a week to get back.
The MR Box has the potential to solve this issue. It is portable, easy to use, and—at less than a dollar per chip—affordable. It is also compact, weighing less than 11 pounds. The technology inside each box, called digital microfluidics- enzyme-linked immunosorbent assay (DMF-ELISA), or “ELISA on a chip,” has some distinct advantages over other technologies used to detect measles and rubella. It can test samples from up to four people at the same time and yields results in less than an hour—much more efficient than transporting blood samples to the national lab and waiting several days for laboratory results. Since measles spreads rapidly, having technology that can provide immediate results in the field is a game changer.
Multiplex Immunoassay: A Cost-Effective Way to Conduct Surveillance
CDC microbiologists work with laboratory scientists around the world on a tool that can detect more than 35 pathogens with a single drop of blood.
CDC has developed and validated a multiplex immunoassay that detects antibodies for more than 35 viral, bacterial, and parasitic diseases and provides an assessment of vaccination coverage levels, using a single small blood sample. This test provides a more cost-effective approach to obtain critical public health information, as most surveillance costs are related to sample collection. Since late 2017, CDC has used the multiplex immunoassay to conduct integrated serosurveillance for infectious diseases in large-scale pilots in Brazil, Mexico, Paraguay, Thailand, and the United States. To respond to increasing requests, CDC has identified establishing a multiplex reference laboratory to assist country partners as a priority.
Leading Innovations in HIV Testing
CDC has developed an HIV rapid test that can diagnose HIV in minutes and distinguish recent (i.e., likely occurring within the past year) from long- standing HIV infection. This test, now commercialized by two manufacturers, is being integrated into routine HIV testing services in 17 PEPFAR-supported countries to establish a real-time HIV surveillance and response system. A main objective of the system is to identify clusters of recent transmission. It provides an opportunity to prevent onward transmission and link HIV services to those who require them. CDC continues to lead innovations in testing for recent HIV infection to ensure wider accessibility and use of the tool.
Understanding Insecticide-Resistant Mosquitoes
Mosquitoes can transmit a wide range of diseases, including malaria, dengue fever, chikungunya, and West Nile virus. Using insecticides is one way to control mosquitoes and the diseases they spread. However, mosquitoes have become increasingly resistant to insecticides, thus compromising mosquito control efforts. In 2018, CDC research demonstrated that insecticide exposure impacts bacteria that colonize mosquitoes (the mosquito microbiota). The presence of insecticide-metabolizing bacteria in resistant mosquitoes could potentially be used to predict insecticide resistance in the field. More research is needed to fully understand insecticide resistance in mosquitoes.

The CDC Bottle Bioassay determines if particular ingredients are able to kill an insect vector, such as a mosquito, at a specific location at a given time. Credit: David Snyder, CDC Foundation.