How to Increase COVID-19 Vaccination upon Discharge from Hospitals, Emergency Departments & Urgent Care Facilities
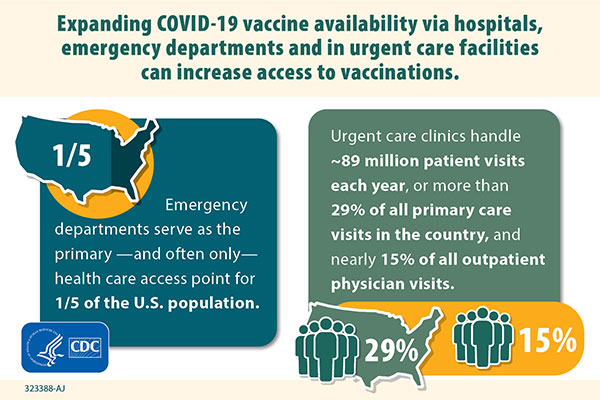
Hospitals, emergency departments (EDs), and urgent care facilities (UCs) in the United States can play an influential role in building confidence in and improving COVID-19 vaccine uptake, as healthcare providers are the most trusted source of health information.
On this page, the Centers for Disease Control and Prevention (CDC) provides information for state health departments and jurisdictions, as well as healthcare providers, on the administration of COVID-19 vaccinations to patients upon discharge from hospitals, EDs, and UCs.
- Allocate vaccines to EDs and UCs to be administered during patient discharge. Prioritizing facilities located in counties with a high Social Vulnerability Index (SVI) ranking to help increase health equity in COVID-19 vaccination is recommended.
- Consider enrolling hospitals designated by the Centers for Medicare & Medicaid Services (CMS) as Disproportionate Share Hospitals (DSH), hospitals included in the Health Resources & Services Administration (HRSA) Small Rural Hospital Improvement Program (SHIP), and other hospitals that serve many people who have no other routine source of care, even if not located in high SVI counties.
- Encourage enrolled hospitals to expand COVID-19 vaccination efforts at discharge to all hospital departments. For example, postpartum discharges and patients being discharged to long-term care or rehabilitation facilities could be important additions to vaccination at discharge efforts.
- Know existing jurisdictional vaccine supply will be used to vaccinate patients upon discharge from hospitals, EDs, and UCs; no separate allocation will be provided.
- Ensure all enrolled facilities receive training for the proper vaccine storage, handling, preparation, administration, billing, and reporting requirements of the CDC COVID-19 Vaccination Provider Agreement.
- Educate hospitals, EDs, and UC facilities to offer vaccination to every eligible person at discharge, regardless of citizenship or state of residence.
- Ensure providers do not miss an opportunity to vaccinate every eligible patient by training facilities to follow clinical best practices for vaccination as well as best practices when managing inventory to maximize vaccination and minimize dose wastage.
- Assess vaccination status at triage, in the patient’s medical history, and during medication reconciliation by asking patient, checking electronic medical/health records, and linking with the jurisdiction’s immunization information system (IIS).
- Address vaccine hesitancy with all patients and those that accompany them as part of routine practice.
- Strongly encourage and offer vaccination to all eligible patients and any friends or family who are accompanying them.
- Consider using a pharmacist assigned to the facility to help with medication management to support confirming vaccination status before vaccination.
- Utilize personnel not involved in the direct care of the patient, if available, to administer vaccines if the department is very busy and it would help work flow.
- Offer vaccination services either at bedside or in special vaccination areas during discharge process.
- Encourage patients to enroll in v-safe.
- Document receipt and/or refusal in chart and IIS.
- Complete and provide a COVID-19 Vaccination Record Card to the patient and print out a list of the vaccination(s) given, particularly for patients being transferred/ discharged to rehab, long-term care, or psychiatric facilities.
- Arrange for second dose appointment, if applicable.
- Place patients in the waiting area for the 15-minute observation period after vaccination is complete to assist in improved flow and reduction of crowding.
EDs and UCs can bill the patient’s insurance company for administration of COVID-19 vaccine; however, this should be billed separately from the services that were provided during the patient’s visit.
Patients cannot be charged directly for the vaccine administration fee if they do not have health insurance and cannot be denied vaccination because of a lack of insurance.
For further information on reimbursement requirements, please see the CDC COVID-19 Vaccination Program Provider Requirements and Support webpage.
Use CDC resources to assist with addressing patients’ concerns regarding vaccines and vaccination. Also address vaccine hesitancy with those who accompany a patient as part of routine practice.
Patients who are not moderately or severely ill and are being discharged from hospital admission, 24-hour observation, or an ED or UC visit may be vaccinated.
Patients with current COVID-19 infection should defer vaccination until they have met criteria to discontinue isolation.
If the patient is a minor, healthcare providers are to follow all state laws regarding consent of minors for vaccination.
Medicare will pay a doctor or other healthcare provider to administer the COVID-19 vaccine to a patient in their home, at no cost. Learn more at Medicare.gov.
Any COVID-19 vaccine product can be used for this activity.
For a product that requires two doses:
- Arrange for a second-dose appointment.
- Counsel patients why the second dose is important and encourage patients to return for it.
- Work with local and state government and local trusted CBOs to address social determinants of health that may pose barriers to receiving a second dose of vaccine, such as:
- Lack of transportation
- Nonflexible work schedules
- Primary language spoken
- Other factors
While continuing to follow best practices to use every dose possible, providers should not miss an opportunity to vaccinate every eligible person when they are ready to get vaccinated, even if it means puncturing a multidose vial to administer vaccine without having enough people available to receive each dose.