Lesson 1: Introduction to Epidemiology
Section 11: Epidemic Disease Occurrence
Level of disease
The amount of a particular disease that is usually present in a community is referred to as the baseline or endemic level of the disease. This level is not necessarily the desired level, which may in fact be zero, but rather is the observed level. In the absence of intervention and assuming that the level is not high enough to deplete the pool of susceptible persons, the disease may continue to occur at this level indefinitely. Thus, the baseline level is often regarded as the expected level of the disease.
While some diseases are so rare in a given population that a single case warrants an epidemiologic investigation (e.g., rabies, plague, polio), other diseases occur more commonly so that only deviations from the norm warrant investigation. Sporadic refers to a disease that occurs infrequently and irregularly. Endemic refers to the constant presence and/or usual prevalence of a disease or infectious agent in a population within a geographic area. Hyperendemic refers to persistent, high levels of disease occurrence.
Occasionally, the amount of disease in a community rises above the expected level. Epidemic refers to an increase, often sudden, in the number of cases of a disease above what is normally expected in that population in that area. Outbreak carries the same definition of epidemic, but is often used for a more limited geographic area. Cluster refers to an aggregation of cases grouped in place and time that are suspected to be greater than the number expected, even though the expected number may not be known. Pandemic refers to an epidemic that has spread over several countries or continents, usually affecting a large number of people.
Epidemics occur when an agent and susceptible hosts are present in adequate numbers, and the agent can be effectively conveyed from a source to the susceptible hosts. More specifically, an epidemic may result from:
- A recent increase in amount or virulence of the agent,
- The recent introduction of the agent into a setting where it has not been before,
- An enhanced mode of transmission so that more susceptible persons are exposed,
- A change in the susceptibility of the host response to the agent, and/or
- Factors that increase host exposure or involve introduction through new portals of entry.(47)
The previous description of epidemics presumes only infectious agents, but non-infectious diseases such as diabetes and obesity exist in epidemic proportion in the U.S.(51, 52)
 Exercise 1.10
Exercise 1.10
For each of the following situations, identify whether it reflects:
- Sporadic disease
- Endemic disease
- Hyperendemic disease
- Pandemic disease
- Epidemic disease
- ____ 22 cases of legionellosis occurred within 3 weeks among residents of a particular neighborhood (usually 0 or 1 per year)
- ____ Average annual incidence was 364 cases of pulmonary tuberculosis per 100,000 population in one area, compared with national average of 134 cases per 100,000 population
- ____ Over 20 million people worldwide died from influenza in 1918–1919
- ____ Single case of histoplasmosis was diagnosed in a community
- ____ About 60 cases of gonorrhea are usually reported in this region per week, slightly less than the national average
Epidemic Patterns
Epidemics can be classified according to their manner of spread through a population:
- Common-source
- Point
- Continuous
- Intermittent
- Propagated
- Mixed
- Other
A common-source outbreak is one in which a group of persons are all exposed to an infectious agent or a toxin from the same source.
If the group is exposed over a relatively brief period, so that everyone who becomes ill does so within one incubation period, then the common-source outbreak is further classified as a point-source outbreak. The epidemic of leukemia cases in Hiroshima following the atomic bomb blast and the epidemic of hepatitis A among patrons of the Pennsylvania restaurant who ate green onions each had a point source of exposure.(38, 44) If the number of cases during an epidemic were plotted over time, the resulting graph, called an epidemic curve, would typically have a steep upslope and a more gradual downslope (a so-called “log-normal distribution”).
Figure 1.21 Hepatitis A Cases by Date of Onset, November–December, 1978
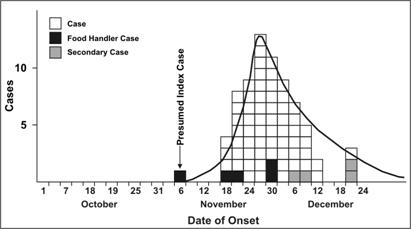
Source: Centers for Disease Control and Prevention. Unpublished data; 1979.
In some common-source outbreaks, case-patients may have been exposed over a period of days, weeks, or longer. In a continuous common-source outbreak, the range of exposures and range of incubation periods tend to flatten and widen the peaks of the epidemic curve (Figure 1.22). The epidemic curve of an intermittent common-source outbreak often has a pattern reflecting the intermittent nature of the exposure.
Figure 1.22 Diarrheal Illness in City Residents by Date of Onset and Character of Stool, December 1989–January 1990
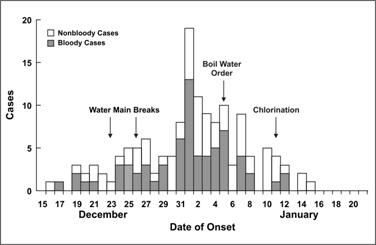
Source: Centers for Disease Control and Prevention. Unpublished data; 1990.
A propagated outbreak results from transmission from one person to another. Usually, transmission is by direct person-to-person contact, as with syphilis. Transmission may also be vehicleborne (e.g., transmission of hepatitis B or HIV by sharing needles) or vectorborne (e.g., transmission of yellow fever by mosquitoes). In propagated outbreaks, cases occur over more than one incubation period. In Figure 1.23, note the peaks occurring about 11 days apart, consistent with the incubation period for measles. The epidemic usually wanes after a few generations, either because the number of susceptible persons falls below some critical level required to sustain transmission, or because intervention measures become effective.
Figure 1.23 Measles Cases by Date of Onset, October 15, 1970—January 16, 1971
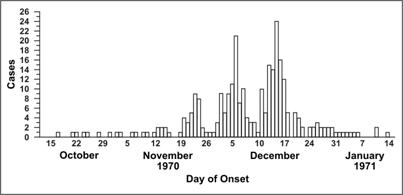
Source: Centers for Disease Control and Prevention. Measles outbreak—Aberdeen, S.D. MMWR 1971;20:26.
Some epidemics have features of both common-source epidemics and propagated epidemics. The pattern of a common-source outbreak followed by secondary person-to-person spread is not uncommon. These are called mixed epidemics. For example, a common-source epidemic of shigellosis occurred among a group of 3,000 women attending a national music festival (Figure 1.24). Many developed symptoms after returning home. Over the next few weeks, several state health departments detected subsequent generations of Shigella cases propagated by person-to-person transmission from festival attendees.(48)
Figure 1.24 Shigella Cases at a Music Festival by Day of Onset, August 1988
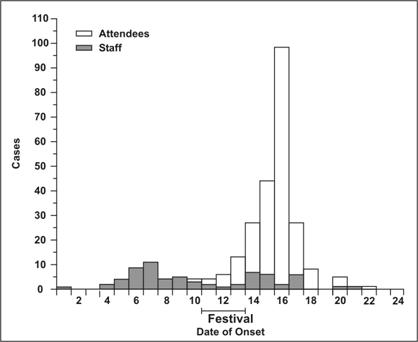
Adapted from: Lee LA, Ostroff SM, McGee HB, Johnson DR, Downes FP, Cameron DN, et al. An outbreak of shigellosis at an outdoor music festival. Am J Epidemiol 1991;133:608–15.
Finally, some epidemics are neither common-source in its usual sense nor propagated from person to person. Outbreaks of zoonotic or vectorborne disease may result from sufficient prevalence of infection in host species, sufficient presence of vectors, and sufficient human-vector interaction. Examples (Figures 1.25 and 1.26) include the epidemic of Lyme disease that emerged in the northeastern United States in the late 1980s (spread from deer to human by deer ticks) and the outbreak of West Nile encephalitis in the Queens section of New York City in 1999 (spread from birds to humans by mosquitoes).(49, 50)
Figure 1.25 Number of Reported Cases of Lyme Disease by Year — United States, 1992–2003.
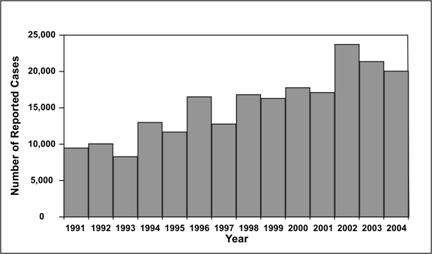
Data Source: Centers for Disease Control and Prevention. Summary of notifiable diseases — United States, 2003. Published April 22, 2005, for MMWR 2003;52(No. 54):9,17,71–72.
Figure 1.26 Number of Reported Cases of West Nile Encephalitis — New York City, 1999
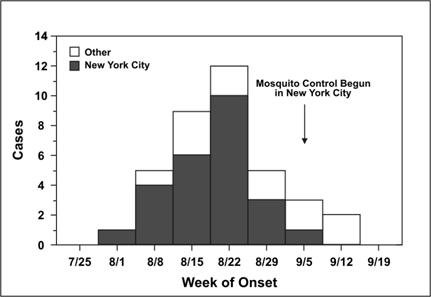
Source: Centers for Disease Control and Prevention. Outbreak of West Nile-Like Viral Encephalitis — New York, 1999. MMWR 1999;48(38):845–9.
 Exercise 1.11
Exercise 1.11
For each of the following situations, identify the type of epidemic spread with which it is most consistent.
- Point source
- Intermittent or continuous common source
- Propagated
- ____ 21 cases of shigellosis among children and workers at a day care center over a period of 6 weeks, no external source identified incubation period for shigellosis is usually 1—3 days)
- ____ 36 cases of giardiasis over 6 weeks traced to occasional use of a supplementary reservoir (incubation period for giardiasis 3–25 days or more, usually 7–10 days)
- ____ 43 cases of norovirus infection over 2 days traced to the ice machine on a cruise ship (incubation period for norovirus is usually 24–48 hours)
References (This Section)
- Centers for Disease Control and Prevention. Hepatitis A outbreak associated with green onions at a restaurant–Monaca, Pennsylvania, 2003. MMWR 2003; 52(47):1155–7.
- Cobb S, Miller M, Wald N. On the estimation of the incubation period in malignant disease. J Chron Dis 1959;9:385–93.
- Kelsey JL, Thompson WD, Evans AS. Methods in observational epidemiology. New York: Oxford University Press; 1986. p. 216.
- Lee LA, Ostroff SM, McGee HB, Jonson DR, Downes FP, Cameron DN, et al. A. outbreak of shigellosis at an outdoor music festival. Am J Epidemiol 1991. 133:608–15.
- White DJ, Chang H-G, Benach JL, Bosler EM, Meldrum SC. Means RG, et al. Geographic spread and temporal increase of the Lyme diseas. epidemic. JAMA 1991;266:1230–6.
- Centers for Disease Control and Prevention. Outbreak of West Nile-Like Viral Encephalitis–New York, 1999. MMWR 1999;48(38):845–9.
- Centers for Disease Control and Prevention. Prevalence of overweight and obesity among adults with diagnosed diabetes — United States. 1988–1994 and 1999–2002. MMWR 2004;53(45):1066–8.
- National Center for Health Statistics [Internet]. Atlanta: Centers for Disease Control and Prevention [updated 2005 Feb 8]. Available from: https://www.cdc.gov/nchs/products/pubs/pubd/hestats/overwght99.htm.
Figure 1.21
Description: Epidemic curve (histogram) shows the presumed index case of Hepatitis A, followed 4 days later by a steep increase in cases which tapers off to 0. Cases who were food handlers and secondary cases are also shown. Return to text.
Figure 1.22
Description: Histogram shows the number of cases of diarrhea by date of onset. Arrows also show when water main breaks, a boil water order, and water chlorination occur. Bloody and nonbloody diarrheal illness is indicated by different colors. Overall increases and decreases in cases is easily seen. Return to text.
Figure 1.23
Description: Histogram shows the number of measles cases peaks around November 23 then declines. It peaks again on December 5 and declines until it peaks a third time. Return to text.
Figure 1.24
Description: Histogram shows the number of Shigella cases among staff and attendees in stacked bars. The first case occurs in a staff member on day 1. The number of cases among staff and attendees is seen in relationship to the festival dates. Return to text.
Figure 1.25
Description: Histogram shows a general increasing trend in the number of reported cases of Lyme disease. Return to text.
Figure 1.26
Description: Histogram shows reported cases of West Nile Encephalitis in New York City and other locations. In NYC, cases drop to 0 after mosquito control activities are begun in the city. Reported cases in other locations continue at about the same rate. Return to text.