Recommendations for Fully Vaccinated People
COVID-19 Homepage
Performing Broad-Based Testing for SARS-CoV-2 in Congregate Settings
Logistical considerations and tips for administrators of congregate correctional, detention, and homeless service settings
CDC is reviewing this page to align with updated guidance.
Summary of Recent Changes
Introduction
This tool is intended to help public health departments, healthcare providers, and administrators of congregate settings prepare for broad-based viral testing in correctional facilities and homeless service settings, after known or suspected exposure to the virus that causes COVID-19 or when there is moderate to substantial transmission in the community. For information about testing in nursing homes, please see the considerations for Performing Facility-wide SARS-CoV-2 Testing in Nursing Homes. This document is intended to accompany CDC’s Overview of Testing for SARS-CoV-2 and interim considerations for facility-wide testing in specific settings.
CDC provides guidance for SARS-CoV-2 testing strategies for congregate settings, including correctional and detention facilities and homeless shelters and encampments. The present document is intended to complement the setting-specific guidance and provide considerations to inform planning for testing scenarios.
- Interim Guidance for SARS-CoV-2 Testing in Homeless Shelters and Encampments covers guidance for testing as a prevention measure in homeless shelters and encampments.
- Interim Guidance for SARS-CoV-2 Testing in Correctional and Detention Facilities covers guidance for testing as a prevention measure in correctional and detention facilities.
Supplies needed
- Personal Protective Equipment (PPE) for staff: N95 equivalent or higher-level respirator (or mask if respirators are not available), masks, gloves, gowns, eye protection (goggles or disposable face shields that cover the front and sides of the face), and physical barriers (for example: plexiglass).
- Masks for people being tested.
- Sanitation and hygiene: Cleaning and disinfection supplies; biohazard waste (red) trash bags and boxes; regular trash bags and cans; touchless dispensers with hand sanitizer;[ 1 ] handwashing station with potable water, soap, and paper towels; and supplies for cleaning a spill of transport media or biological specimens.
- Thermometers: Non-contact digital thermometers and extra batteries.
- Registration and interview materials:[ 2 ] Folding chairs, folding table, clipboards, pens, markers, specimen sticker labels,[ 3 ] paper forms, laptops or tablets, software,[ 4 ] and access to power.
- Test kits: Plastic specimen transport bags, sterile swabs, specimen collection vials with transport media, and prefilled labels.
- Educational materials: Information in appropriate languages and for appropriate literacy levels on COVID-19 testing, test results and what they mean, information on quarantine and isolation, and how to slow the spread of COVID-19.
- General supplies: Tape to mark lines for at least 6 feet of separation, signs to direct flow, cooler and ice packs, on-site refrigeration with temperature monitor, first aid kit, portable pulse oximeter, and portable blood pressure cuff/monitor for use by the on-site medical team.
Supply Notes:
- Alcohol-based hand rub with 60%-95% alcohol.
- Use items made of materials that can be cleaned between individuals.
- Ideally, preprinted with space for date, name, date of birth, ID number, and specimen type.
- Contact tracing software being used by public health authority or spreadsheet with fields for demographic information, location and date of testing, and results.
Planning
- Coordinate planning between healthcare providers, the local health department, and the laboratory that will perform the testing.
- Adapt all plans to the type of specimen being collected:
- Determine whether you will conduct SARS-CoV-2 nucleic acid or antigen test and what specimens to collect.
- Some tests are point-of-care tests, meaning results may be available at the testing site in less than an hour. Other tests must be sent to a laboratory to analyze, a process that may take 1-2 days once received by the lab.
- If relevant, discuss with the receiving laboratory the requirements for supplies, storage, and transportation of specimens.
- If testing is not urgent, discuss considerations for what day the specimen collection will be performed, as labs usually prefer to not receive specimens near the end of the week.
- Develop a plan for staffing and training the interview and testing teams (see example in Tables below).
- PPE requirements vary based on the staff’s role in specimen collection and whether they will be at least 6 feet away from the person being tested (see example in Tables below):
- Gloves and mask are needed for staff who will not be directly involved in specimen collection or who will be greater than 6 feet away from person being tested.
- Gown, NIOSH-approved N95 equivalent or higher-level respirator (or mask if a respirator is not available), gloves, and eye protection are needed for staff collecting specimens or working within 6 feet of the person being tested.
- Consider whether you can minimize the number of staff needed and amount of PPE used by having individuals collect their own specimens while being supervised by healthcare providers who are at least 6 feet away.
- Ensure that all staff involved in specimen collection are appropriately trained and wear PPE as appropriate to their role (see example in Tables below).
- Training includes proper use of PPE, including donning and doffing; symptom screening procedure; and proper technique for specimen collection.
- For staff having direct contact with people being tested or specimens, gloves should be changed and hands sanitized after each person tested (see example in Tables below). Staff not having regular direct contact with people being tested or specimens should change their gloves and sanitize their hands after contacting individuals or potentially contaminated surfaces, or as specified in example Tables below.
- Staff should change or clean and sanitize eye protection when it is soiled (such as after a patient sneezes or coughs onto it) or whenever they touch it or take it off.
- Staff should change their respirators and masks whenever they are soiled or become wet or whenever they touch them or take them off.
- Staff should change their gown when it becomes soiled or when they have more than minimal contact with the person being swabbed. They may wear the same gown to swab more than one person, provided they minimize contact with the person being swabbed.
- Consider the physical space where the testing will be performed (see below).
- Clearly communicate to potential participants who is eligible for testing and any limits on your capacity for testing.
- The U.S. Department of Health and Human Services is required to report de-identified, disaggregated race and ethnicity data, in addition to other data elements, for people tested for or diagnosed with COVID-19. These data help to improve our understanding of the impact of COVID-19 on racial and ethnic minority populations.
- Determine how you will ask and record race and ethnicity on anyone receiving a test.
- Ensure these data are reported to public health authorities with the person’s test results.
- Carefully consult CDC guidance on infection control practices for managing patients with suspected or confirmed COVID-19 and for specimen collection and handling. Collecting nasopharyngeal specimens can induce coughing or sneezing, which can spread COVID-19.
- Anticipate how to address individuals’ mobility issues and language barriers.
- Develop a plan for isolating individuals who are symptomatic or whose test results are returned positive.
- Develop a risk communication plan for addressing individuals’ concerns about confidentiality, potential stigma or undesirable outcomes based on test results (being moved to new location, separated from family, etc.), and any distrust. Plan a response to situations when individuals refuse testing.
- Develop a plan for communicating results with people who’ve been tested and public health authorities.
- Develop a plan for collaborating with public health authorities on case investigation and contact tracing.
- Develop a plan for coordinating with local EMS and healthcare providers in case individuals need medical attention.
- Develop a plan for disposing of biohazard waste (used specimen collection materials; soiled gloves, masks, gowns, etc.).
Physical space
- In general, an outdoor location for mass testing events is preferred because it has better ventilation and more room for social distancing. Provide climate-controlled or climate-protected rest areas (large enough for social distancing) for staff.
- If an outdoor location is not feasible, large indoor spaces (for example gymnasiums) are best, where sufficient space can be maintained between stations (i.e., periphery greater than 6 feet apart).
- For indoor specimen collection activities, designate separate spaces for each specimen collection testing station, either rooms with doors that close fully or protected spaces removed from other stations by distance and physical barriers, such as privacy curtains and plexiglass.
- To prevent inducing coughing/sneezing in an environment where multiple people are present and could be exposed, avoid collecting specimens in open-style housing spaces with current residents or in multi-use areas where other activities are occurring.
- To improve indoor ventilation, review considerations on the Ventilation in Buildings page.
- Do not keep testing and other supplies in the immediate specimen collection area to avoid the possibility of contamination test materials. Consider having each person carry their prefilled specimen bag (containing a swab and labeled sterile viral transport media container) from the check-in area to the specimen collection area.
- Clean and disinfect all surfaces often using an Environmental Protection Agency-registered disinfectant from List N:
- At least hourly for surfaces within 6 feet of where specimen collection was performed;
- Anytime the surface is visibly soiled or within 6 feet of an uncovered cough or sneeze;
- At the end of shift for all surfaces and equipment in the specimen collection area.
Flow for testing multiple people in succession
- Provide masks for those undergoing testing in the area being used for the testing event. The following categories of people are exempt from the requirement to wear a mask:
- A child under the age of 2;
- A person with a disability who cannot wear a mask, or cannot safely wear a mask, for reasons related to the disability;
- A person for whom wearing a mask would create a risk to workplace health, safety, or job duty as determined by the relevant workplace safety guidelines or federal regulations.
- As able, all participants undergoing testing should wear a well-fitting mask that covers the nose and mouth throughout the process, only removing it during swabbing.
- Develop a plan of how individuals will flow through functional stations in one direction (see example in Figure below).
- Designate stations with clear functional roles, define responsibilities for staff in each station, and provide PPE supplies and training to staff as appropriate to their role (see example in Tables below). To prevent contamination, testing staff in full PPE should not leave the testing area.
- Pilot the processes and flow before the actual testing event. Staff could be tested at this time.
- Place touchless hand sanitizers between each station and at the facility’s entrance.
- Coordinate so that the flow of individuals is steady, moves in one direction, and does not lead to crowding.
- Minimize the amount of time an individual spends in the testing area.
- Individuals awaiting testing should not wait within 6 feet of where specimen collection is being done or downstream from the area if the indoor space has directional airflow.
- Have the person being swabbed face away from others so that if they cough or sneeze, the respiratory droplets will not be directed toward another person or a space where others will walk.
- Keep people at least 6 feet apart and use physical barriers where appropriate. In situations where people will form lines, encourage people to stay at least 6 feet apart by providing signs or other visual cues, such as tape or chalk marks.
- If participants are already cohorted (by residence or work group), test them together to limit their exposures to people in other groups.
- Process families together and consider extra space that might be needed to accommodate multiple people being tested.
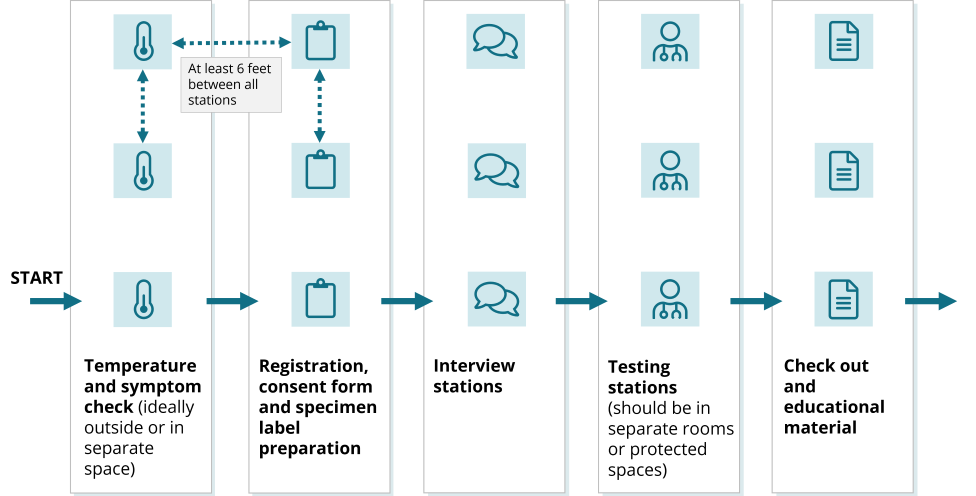
Figure. Example of layout and flow of individuals being screened. Station tables should always be at least 6 feet apart. Keep as much distance as possible between staff and participants. Use physical barriers (plexiglass, for example) where appropriate. Place chairs at an angle to reduce face-to-face exposure.
Role
Role
Personal Protective Equipment
Personal Protective Equipment
Duties
Duties
Temperature check and consent form
Temperature check and consent form
2–3 people working in parallel
2–3 people working in parallel
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
- Instruct the individual to sanitize hands and recommend wearing a mask
- Check and record temperature on interview form or electronic record
- Add date, location, and other details to interview form
- Hand consent and interview form to participant
- Instruct the individual to sanitize hands and recommend wearing a mask
- Check and record temperature on interview form or electronic record
- Add date, location, and other details to interview form
- Hand consent and interview form to participant
Registration, consent form, and test kit labeling
Registration, consent form, and test kit labeling
2–3 teams of 2 people (registrar and labeler); roles can be combined if fewer staff or individuals to be tested
2–3 teams of 2 people (registrar and labeler); roles can be combined if fewer staff or individuals to be tested
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
- Collect signed consent forms
- Enter first and last name (with spelling), date of birth, race, ethnicity, and contact phone number or email address onto documents or electronic record
- Record information on where the individual has been in the last 48 hours to facilitate contact tracing if the individual’s test results are positive and there is concern that the individual could be lost to follow-up
- Write date, first and last name, date of birth, specimen type (such as NP, NS, OP) on label
- Attach sticker label to the specimen collection vial
- Hand bag with specimen vial to participant and direct participant to interview station
- Clean and disinfect clipboards and pens between participants
- Collect signed consent forms
- Enter first and last name (with spelling), date of birth, race, ethnicity, and contact phone number or email address onto documents or electronic record
- Record information on where the individual has been in the last 48 hours to facilitate contact tracing if the individual’s test results are positive and there is concern that the individual could be lost to follow-up
- Write date, first and last name, date of birth, specimen type (such as NP, NS, OP) on label
- Attach sticker label to the specimen collection vial
- Hand bag with specimen vial to participant and direct participant to interview station
- Clean and disinfect clipboards and pens between participants
Interview and symptom screening
Interview and symptom screening
5-6 people
5-6 people
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
- Complete the form or electronic record with the participant following the script
- Keep the form and direct the participant to testing station
- Clean and disinfect participant side of table following each interview
- Complete the form or electronic record with the participant following the script
- Keep the form and direct the participant to testing station
- Clean and disinfect participant side of table following each interview
Guide
Guide
1–2 people
1–2 people
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Help direct participants between stations
Help direct participants between stations
Floater
Floater
1 person
1 person
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Troubleshoot issues that arise for any of the stations
Troubleshoot issues that arise for any of the stations
Testing staff and duties
2-3 teams of 3 people each
Role
Role
Personal Protective Equipment
Personal Protective Equipment
Duties
Duties
Bagger
Bagger
3 people
3 people
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
- Stand just outside the testing station
- Receive bag with vial from participant; verify name and date of birth
- Remove specimen transport bag and hand vial and swab to snipper
- After specimen has been collected, hold specimen transport bag open for snipper to drop vial into the bag, ensuring the vial touches only the inside of the bag
- Holding the outside of the bag, double check that the vial is closed tightly
- Seal the bag, removing as much excess air as possible
- Store vial and bag in cooler with frozen ice packs
- Note: Specimens should be transferred from small coolers to refrigeration unit frequently to maintain temperature control
- Stand just outside the testing station
- Receive bag with vial from participant; verify name and date of birth
- Remove specimen transport bag and hand vial and swab to snipper
- After specimen has been collected, hold specimen transport bag open for snipper to drop vial into the bag, ensuring the vial touches only the inside of the bag
- Holding the outside of the bag, double check that the vial is closed tightly
- Seal the bag, removing as much excess air as possible
- Store vial and bag in cooler with frozen ice packs
- Note: Specimens should be transferred from small coolers to refrigeration unit frequently to maintain temperature control
Swabber
Swabber
3 people
3 people
- Hand tissue to participant and instruct them to blow their nose and deposit in biohazard (red) waste
- Provide instructions and explain testing procedure
- Take swab from snipper and collect specimen
- Insert swab with specimen into vial
- Instruct participant to sanitize hands and check out
- Hand tissue to participant and instruct them to blow their nose and deposit in biohazard (red) waste
- Provide instructions and explain testing procedure
- Take swab from snipper and collect specimen
- Insert swab with specimen into vial
- Instruct participant to sanitize hands and check out
Snipper
Snipper
3 people
(if using a breakable swab, then 2-person teams are sufficient, i.e., combine snipper and swabber roles)
3 people
(if using a breakable swab, then 2-person teams are sufficient, i.e., combine snipper and swabber roles)
- Take vial and swab from bagger and hand swab to swabber
- Cut swab after specimen has been collected
- Replace the vial lid and ensure lid is sealed tightly
- Drop vial into specimen transport bag held open by bagger
- Clean scissors with alcohol wipe, leave scissor blades open to air dry
- Clean space between tests
- Take vial and swab from bagger and hand swab to swabber
- Cut swab after specimen has been collected
- Replace the vial lid and ensure lid is sealed tightly
- Drop vial into specimen transport bag held open by bagger
- Clean scissors with alcohol wipe, leave scissor blades open to air dry
- Clean space between tests
Specimen transporter
Specimen transporter
1 person
(can be combined with floater if fewer staff or individuals to be tested)
1 person
(can be combined with floater if fewer staff or individuals to be tested)
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Periodic collection of bagged specimens from testing stations to on-site refrigeration if available or larger cooler. Temperature control should be monitored.
Periodic collection of bagged specimens from testing stations to on-site refrigeration if available or larger cooler. Temperature control should be monitored.
Check out
Check out
1-2 people
1-2 people
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Gloves, mask if more than 6 feet away from person being tested [ 2 ]
Provide instructions on follow-up and how to get results
Provide instructions on follow-up and how to get results
Notes:
- Fewer and smaller teams might be appropriate, depending on the scale of specimen collection or number of staff available. Notes on possible role-sharing are included in the tables. Having participants collect their own specimens is another way to minimize the number of staff needed and amount of PPE used.
- If working within 6 feet of person being tested, then use gown, respirator, eye protection, and gloves.
- N95 or equivalent or higher-level respirator (or mask if a respirator is not available).
- Goggles or disposable face shields that cover the front and sides of the face.
After testing is complete
- Ensure correct doffing of PPE through monitoring by other staff (“buddies”).
- Clean and disinfect all tables, chairs, pens, clipboards, keyboards, thermometers (also see section above on Physical Space).
- Dispose of biohazard waste according to local policies.
- Maintain proper storage, shipping, transportation of specimens. Shipping of specimens should preferably occur early in the week so that the laboratory staff can receive and process.
- Communicate results to participants – work with local health departments to determine plans for communication. If individuals will be difficult to reach (no contact phone number), identify an alternate mechanism for participants to receive results, such as providing a contact (hotline) number to the participants with instructions on when to call for results.