Summary of Flu Progress since 2009
10 years ago, an influenza (flu) virus emerged that had never been seen before in humans. This novel H1N1 flu virus was first detected in April of 2009 in the United States, and spread quickly around the world. On June 11th, 2009, the World Health Organization declared the start of the first flu pandemic in 40 years. CDC estimates that between 151,700 and 575,400 people died worldwide from the 2009 H1N1 virus infection during the first year the virus circulated. That H1N1 virus has continued to circulate worldwide annually since it emerged in 2009.
The 10-year commemoration of the 2009 H1N1 flu pandemic is an opportunity to reflect on that event in history as well as to acknowledge the importance of ongoing efforts to improve domestic and global capacity to detect and respond to novel flu viruses. Since 2009, substantial advances have been made in influenza science and preparedness. Here’s a summary of progress made in the last 10 years:
Monitoring and Detection
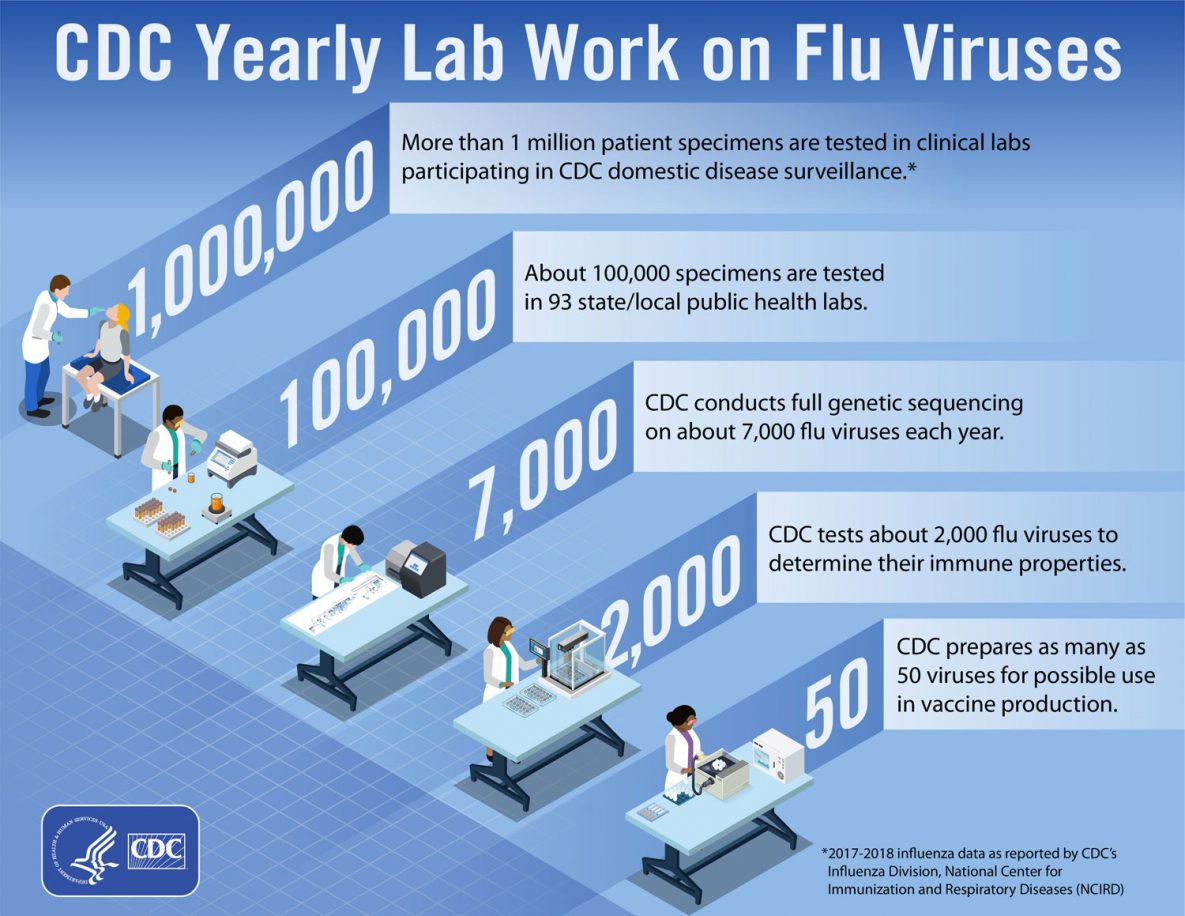
Since the 2009 flu pandemic, CDC has expanded and improved flu surveillance systems and practices.
- CDC implemented a standardized sampling strategy for flu across public health and clinical laboratories that is nationally representative and that ensures efficiency and data confidence. This means that that a new flu virus with pandemic potential can be detected more easily and rapidly.
- All flu virus samples (about 6,000 to 8,000 samples) submitted to CDC now undergo full genetic sequencing as a first step. This provides a complete picture of the many different flu viruses that are circulating in people, enables faster outbreak response, and greatly expands the global flu genetic database.
- CDC partners with three state laboratories that now act as regional reference centers doing genetic sequencing using CDC’s standard testing practices. Data from these three National Influenza Reference Centers (NIRCs) are then uploaded to a CDC-supported “cloud” computing platform, making it instantly accessible to authorized CDC scientists. The creation of these regional hubs has expanded capacity, improved continuity of operations, and accelerated overall response time.
- CDC-developed Reverse Transcription-Polymerase Chain Reaction testing (rRT-PCR) has become the gold standard in flu virus testing among public health labs, resulting in data that are more reliable and available more quickly. CDC makes these test kits available to qualified laboratories through the web-based International Reagent Repository, an online service that supports global surveillance for flu and which can rapidly surge to support demand for testing during a pandemic.
- A systematic assessment of the performance of Rapid Influenza Diagnostic Tests (RIDTs) led to improvements in the use and development of rapid flu virus tests. Working with FDA, CDC supports annual testing of all commercial flu tests to assure that they continue to meet new testing standards.
- Testing for potential flu virus resistance to antiviral drugs, which used to happen only at CDC, has expanded to 19 other laboratories. This expansion increases capacity for testing and accelerates response time. Additionally, CDC is constantly evaluating new flu viruses to determine if they are susceptible to commercially-available and experimental antiviral drugs.
Risk Assessment
CDC developed tools to help assess the public health risk associated with specific flu viruses to inform public health actions.
- New risk assessment tools are available, including one that assesses the potential pandemic risk posed by a novel flu virus prior to its emergence, and another that determines severity after emergence. The first informs pre-pandemic preparedness activities and the second would inform the public health response during an outbreak.
- CDC developed models to estimate the total numbers of U.S. flu illnesses, hospitalizations and deaths (as well as flu illnesses, hospitalizations and deaths prevented by flu vaccination). These models present a fuller picture of the burden of flu and the benefits of vaccination, and are used to inform policy and communications related to seasonal and pandemic flu.
- CDC-led forecasting activities are improving pandemic preparedness through ground-breaking work in predicting the timing, peak, and intensity of regular flu seasons. Flu forecasting uses traditional surveillance data and multiple other data sources in a way that allows researchers to more quickly recognize patterns of flu activity.
Prevention & Treatment

CDC performs genome sequencing to compare the genetic sequences of vaccine viruses with those of circulating viruses.
Substantial progress has been made in the prevention and treatment of seasonal flu in the decade since the 2009 flu pandemic.
- There is more capacity to make vaccines, and new vaccine technologies have been introduced (e.g., cell-grown and recombinant flu vaccines).
- Investments have been made and research is ongoing to develop a universal flu vaccine that would provide longer-lasting, broader protection against a wider array of flu viruses.
- Progress in synthetic biology means that vaccine viruses can now be created in the lab using genetic sequencing data. CDC uses this technology to rapidly generate vaccine viruses against newly emerging avian and swine flu viruses that periodically cause illness in humans.
- There are more drugs to treat flu, including a new class of influenza antiviral drugs, and better availability of these drugs—in part because of the availability of generic options.
- Our ability to measure how well flu vaccines are working has expanded and improved, including now being able to tell how well flu vaccines are working to prevent more serious outcomes like hospitalization or death.
- Updated pre-pandemic planning guidance reflects lessons learned from the 2009 H1N1 pandemic response. For example, there is new, more detailed guidance on the use of non-pharmaceutical interventions to slow the spread of flu during a pandemic.
International Work
In 2019, the World Health Organization launched a 10-year global strategy calling on countries and partners including CDC to align their global and national capacities for flu prevention, rapid detection and response. The strategy aims to reduce the burden and impact of seasonal, zoonotic and pandemic flu.
CDC’s International Influenza Program works with a wide range of partners, like the World Health Organization, National Ministries of Health and others, to build global capacity for pandemic flu response.
- CDC supports the expansion of the WHO’s Global Influenza Surveillance and Response System (GISRS), growing by more than 26% since 2014.
- Since 2009, CDC has worked with 37 countries to fund improvements in detecting and studying flu viruses, helping to strengthen their public health infrastructure.
Substantial progress aside, pandemic flu remains one of the greatest public health challenges of our time. It is impossible to predict when the next pandemic will occur or its impact. CDC is committed to an ongoing process of advancing the science of influenza prevention and preparedness to protect against seasonal flu as well as to prepare for the next pandemic.