[SPEAKER]
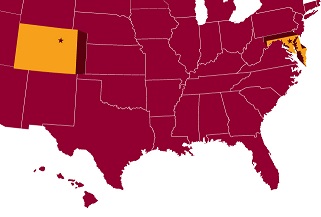
The first of the three studies used before the Minnesota legislature was conducted in Baltimore among Medicaid patients with diabetes. Although this published study did not meet the standards of a randomized controlled trial, the average annual savings of $2,245 per patient was sufficiently dramatic to convince legislators that investing in CHWs was cost-effective. The study also found improved quality of life among patients.
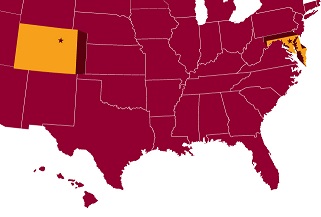
The second study was conducted by Denver Health, the public safety net system for the greater Denver area, which serves 25% of the region’s population. Conservatively estimating Minnesota’s rate of return at half that found in the Denver study, the Minnesota Department of Human Services predicted a net savings to the state of 14 percent above the cost of providing CHW services. This is a 1.14:1 return on investment. The Denver study also found increased use of primary and specialty care and reduced use of urgent, inpatient, and outpatient behavioral health care.
Finally, advocates in Minnesota used a study of asthma management in Hawaii as evidence that employing CHWs could reduce the state’s asthma-related costs and improve quality of life for people with asthma. The Hawaii program reduced emergency room visits related to asthma and reduced overall costs of care for participating patients by 75 percent.
 The following evidence came from studies used in Minnesota:
The following evidence came from studies used in Minnesota: