Antibiotic Use in the United States, 2020 Update: Progress and Opportunities
Introduction
Antibiotic stewardship, or improving how antibiotics are prescribed and used, is critical for optimizing treatment of patients who have infections, protecting patients from harm, and combating antibiotic resistance. In 2019, the Centers for Disease Control and Prevention (CDC) released “Antibiotic Use in the United States, 2018 Update: Progress and Opportunities [PDF – 24 pages],” which included information on how antibiotics were being used across all healthcare settings and highlighted data, resources, and examples of advancement of stewardship activities. This update highlights new opportunities and further progress in antibiotic stewardship, and the importance of integrating sepsis early detection and management since the release of the last report in 2019. During the intervening months, the COVID-19 pandemic has changed healthcare delivery in ways that have had an impact on antibiotic prescribing and presented new challenges that will be important to address for continued progress. Continuing to leverage data for action to inform stewardship activities and collaborate with partners is a priority for CDC to preserve existing gains and continue to make progress to improve antibiotic use.
This report contains:
- Data describing U.S. outpatient antibiotic prescribing rates and implementation of hospital antibiotic stewardship programs by state, including considerations for antibiotic stewardship during the COVID-19 pandemic.
- NHSN Antimicrobial Use Option updates and success stories.
- Recently published literature highlighting progress made and opportunities for improvement in improving antibiotic stewardship in outpatient and emergency department settings.
- New and updated resources for health departments, facilities, and healthcare professionals to implement antibiotic stewardship.
- Examples of key partner contributions to improve antibiotic prescribing practices across the United States and internationally.
CDC will continue to lead U.S. efforts to improve antibiotic use in humans, as outlined in the new National Action Plan for Combatting Antibiotic-Resistant Bacteria, 2020-2025 [PDF – 47 pages]. CDC’s work includes improving antibiotic use in inpatient and outpatient settings, promoting antibiotic use best practices, strengthening antibiotic use surveillance, integrating diagnostic stewardship and sepsis early recognition, and collaborating with partners to develop new antibiotic use guidelines.
Antibiotic Resistance and Patient Safety Portal
The Antibiotic Resistance and Patient Safety Portal is a resource to explore and visualize data on outpatient antibiotic prescribing, hospital antibiotic stewardship implementation, antibiotic resistance, and healthcare-associated infections.
Explore here: https://arpsp.cdc.gov/
CDC works to improve antibiotic use by collecting, analyzing, and publishing data to support antibiotic stewardship efforts in state and local health departments, in healthcare facilities, and by individual prescribers.
Community Antibiotic Prescriptions by State – 2018 – Previous and Revised Methodology
Antibiotics continue to be prescribed unnecessarily in the United States. Though improvements in prescribing have been seen in recent years, prescribing rates still vary widely by state and region, suggesting there are continued stewardship opportunities. These maps display prescription rates of all antibiotic classes per 1,000 population dispensed in outpatient pharmacies across U.S. states in 2018, using previous and revised methodology.
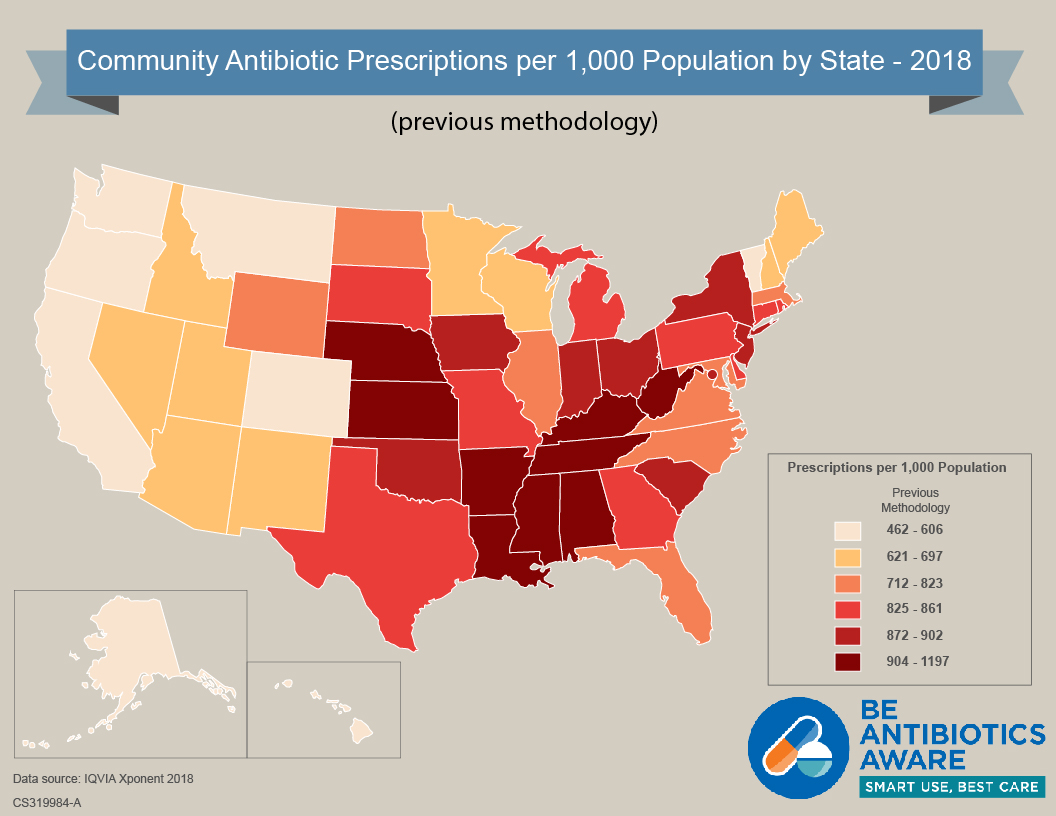
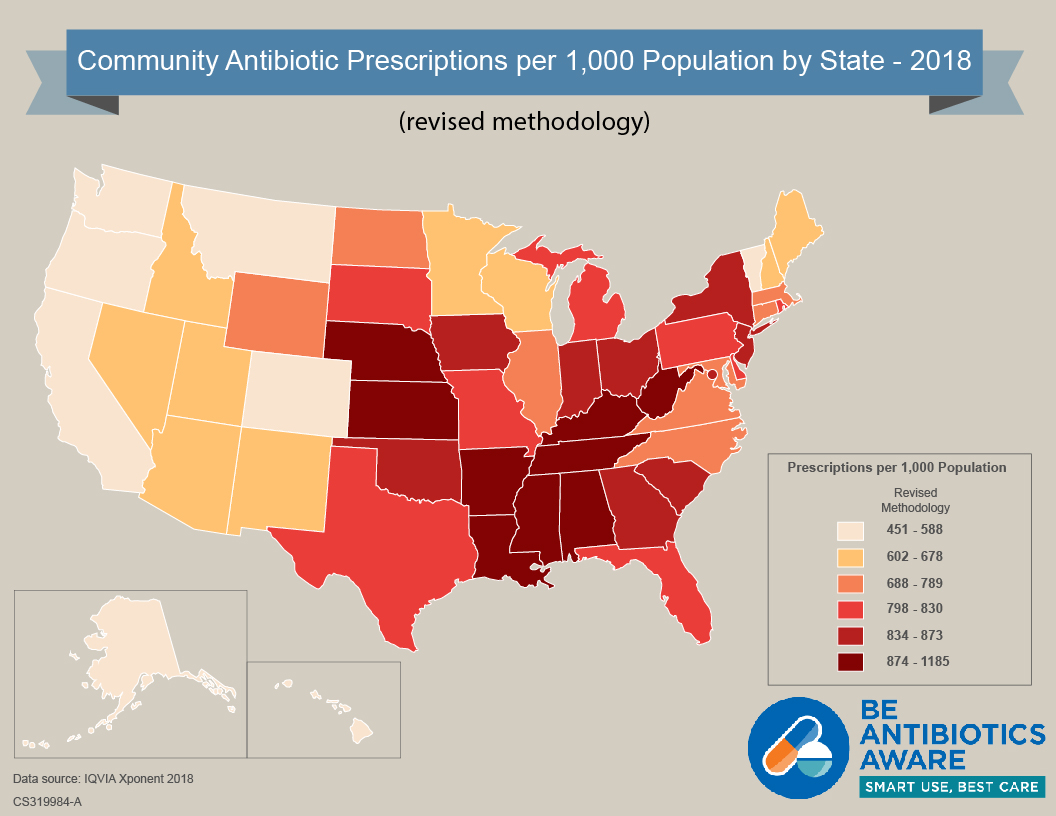
Community Antibiotic Prescriptions by State – 2018 – Previous and Revised Methodology [XLS – 15 KB]
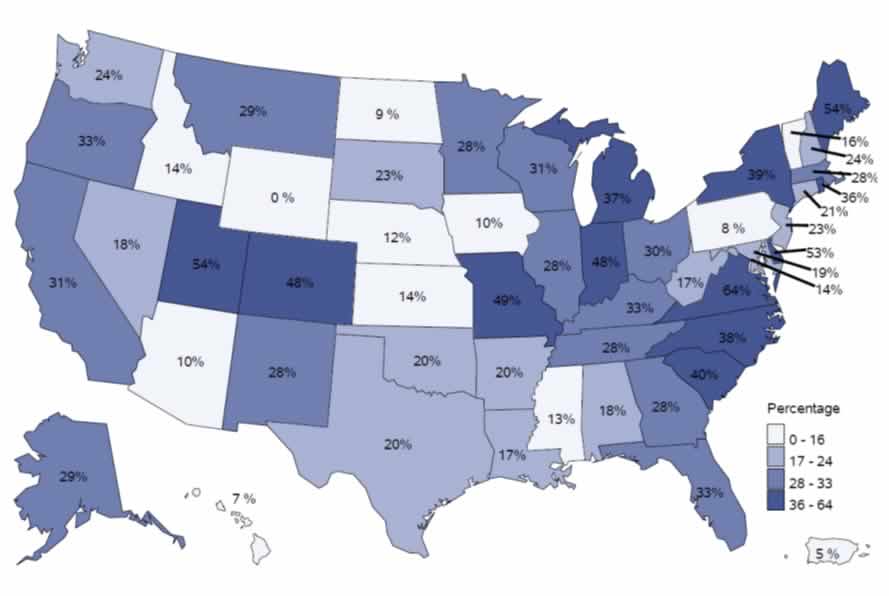
Percentage of Hospitals Meeting all 7 Core Elements, by State – 2019
CDC’s Core Elements of Hospital Antibiotic Stewardship provide a framework for implementation of antibiotic stewardship programs. Partners across the country are using the Core Elements to guide antibiotic stewardship efforts in hospital settings. The Core Elements form the foundation for antibiotic stewardship accreditation standards from the Joint Commission and DNV-GL. The 2019 hospital Conditions of Participation from the Centers for Medicare and Medicaid Services (CMS) created a federal regulation for hospital antibiotic stewardship programs and also reference the Core Elements. This map shows the percentage of hospitals meeting all 7 Core Elements, by state, in 2019. CDC continues to improve assessment of the quality of antibiotic stewardship programs in hospitals.
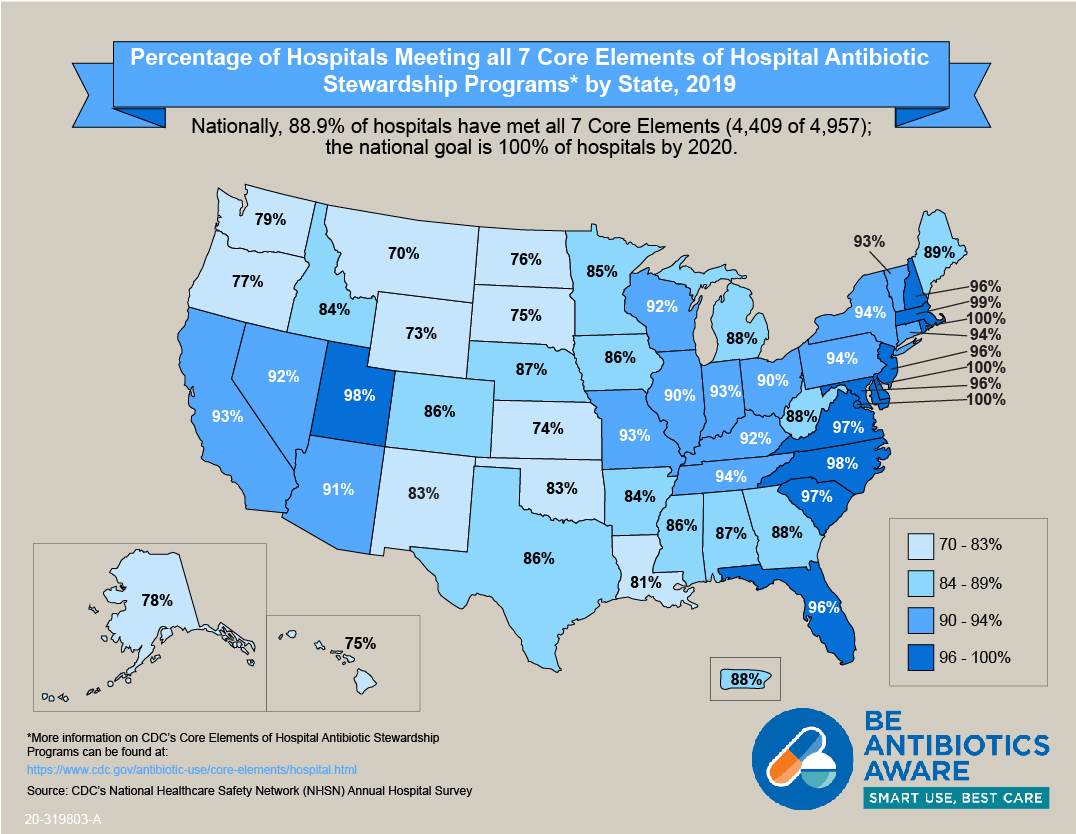
Percentage of Hospitals Meeting all 7 Core Elements, by State – 2019 [XLS – 15 KB]
National Healthcare Safety Network Antimicrobial Use and Resistance (AUR) Module
The NHSN AUR Module [PDF – 57 pages] provides a mechanism for facilities to monitor antibiotic use and/or resistance data to reduce antibiotic-resistant infections through antibiotic stewardship and interrupt transmission of resistant pathogens. One output measure included in NHSN’s Antimicrobial Use (AU) Option of the AUR Module is the Standardized Antimicrobial Administration Ratio (SAAR). The SAAR is a risk-adjusted benchmarking measure of antibiotic use and can help inform stewardship efforts by enabling hospitals to see how their SAARs compare to other facilities. Nearly 2000 acute care hospitals across the United States have submitted at least one month of data to the AU Option as of October 2020.
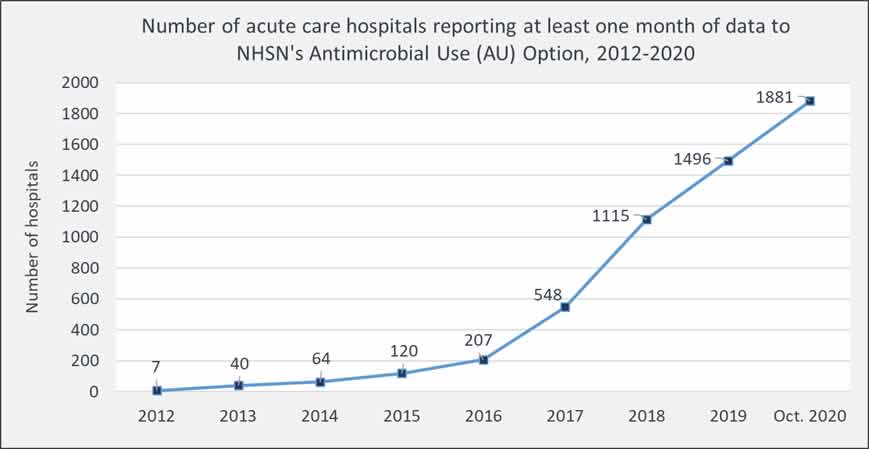
Percentage of acute care hospitals reporting at least one month of data to NHSN’s Antimicrobial Use Option as of October 2020
The 2019 NHSN AU Option Report provides the first summary of NHSN AU data and outlines the following best practices for using AU data in acute care hospitals for action:
- Submit monthly hospital AU data to the NHSN AU Option to guide tracking and reporting for antibiotic stewardship programs.
- Review NHSN AU data at least quarterly to track SAAR/AU data over time to both inform and assess stewardship interventions.
- Report SAAR/AU data on a regular basis to senior leadership, hospital board, hospital committees (e.g., antibiotic stewardship, infection control, pharmacy, & therapeutics), and providers.
- Consider establishing facility-specific SAAR target goals for quality improvement.
- Consider creating and/or participating in the NHSN AU Option Group Function as part of a healthcare system, health department, and/or collaborative.
Refer to AU Option case examples for demonstrations on how facilities are using AU data for action.
New CDC studies showing opportunities for improving antibiotic use:
These new studies are focused on urgent care settings, appropriate antibiotic selection in outpatient settings, and antibiotics and opioid prescribing for dental complaints in emergency departments. All of these studies are examples of how data can be used to inform action at the community, facility, or individual healthcare provider level.
Antibiotic Prescribing Variability in a Large Urgent Care Network: A New Target for Outpatient Stewardship
Stenehjem E, Wallin A, Fleming-Dutra KE, Buckel WR, Stanfield V, Brunisholz KD, Sorensen J, Samore MH, Srivastava R, Hicks LA, Hersh AL. Clin Infect Dis. 2020 Apr 10;70(8):1781-1787.
This study showed that in more than one million urgent care encounters, antibiotics were prescribed during more than one-third of encounters. Clinician prescribing for respiratory encounters varied dramatically, ranging from 3% to 94%, suggesting the need for antibiotic stewardship interventions tailored to the urgent care setting.
First-Line Antibiotic Selection in Outpatient Settings
Palms DL, Hicks LA, Bartoces M, Hersh AL, Zetts R, Hyun DY, Fleming-Dutra KE.
Antimicrob Agents Chemother. 2019 Oct 22;63(11). pii: e01060-19. doi: 10.1128/AAC.01060-19. Print 2019 Nov.
This study compared antibiotic selection for pharyngitis, sinusitis, and acute otitis media in retail clinics, emergency departments, urgent care centers, and offices. The recommended, first-line antibiotics were prescribed in only 50% of patient visits for these conditions, indicating there is room for improvement in antibiotic selection for these common outpatient conditions.
Antibiotic and opioid prescribing for dental-related conditions in emergency departments: United States, 2012 through 2014
Roberts RM, Bohm MK, Bartoces MG, Fleming-Dutra KE, Hicks LA, Chalmers NI.
J Am Dent Assoc. 2020 Mar 15; 1(3):174-181.
It has been documented that patients visiting the emergency department for nontraumatic dental conditions often receive treatment for pain or possible infection, but are referred for dental treatment elsewhere. This study showed that antibiotics and opioids are commonly prescribed during these visits and are potentially avoidable. Access to preventive and acute oral health care for routine dental symptoms, such as dental caries (cavities), may reduce unnecessary prescriptions.
The COVID-19 Pandemic and Antibiotic Prescribing
CDC is monitoring the effects of the COVID-19 pandemic on antibiotic prescribing practices across healthcare. Changes in prescribing have been observed during the pandemic. Changes in healthcare access, patients choosing not to visit healthcare settings for non-urgent medical needs, and lower overall infection rates due to school closures and social distancing are all likely playing a role. Healthcare delivery changes, particularly the expansion of telehealth, will require identification and monitoring of new data sources and consideration for tailored antibiotic stewardship strategies. Data on the “Intersection of Antibiotic Resistance (AR), Antibiotic Use (AU), and COVID-19 [PDF – 24 pages]” were presented during the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria (PACCARB) meeting on September 9-10, 2020.
Outpatient Antibiotic Prescribing
Preliminary data suggest that outpatient antibiotic prescribing decreased during April and May 2020 compared with the same time period in 2019. This is likely due to changes in healthcare access, fewer people seeking healthcare for mild illness, and fewer infections overall due to school closures and social distancing.
Estimated number of outpatients with dispensed antibiotic prescriptions, United States, 2019-2020
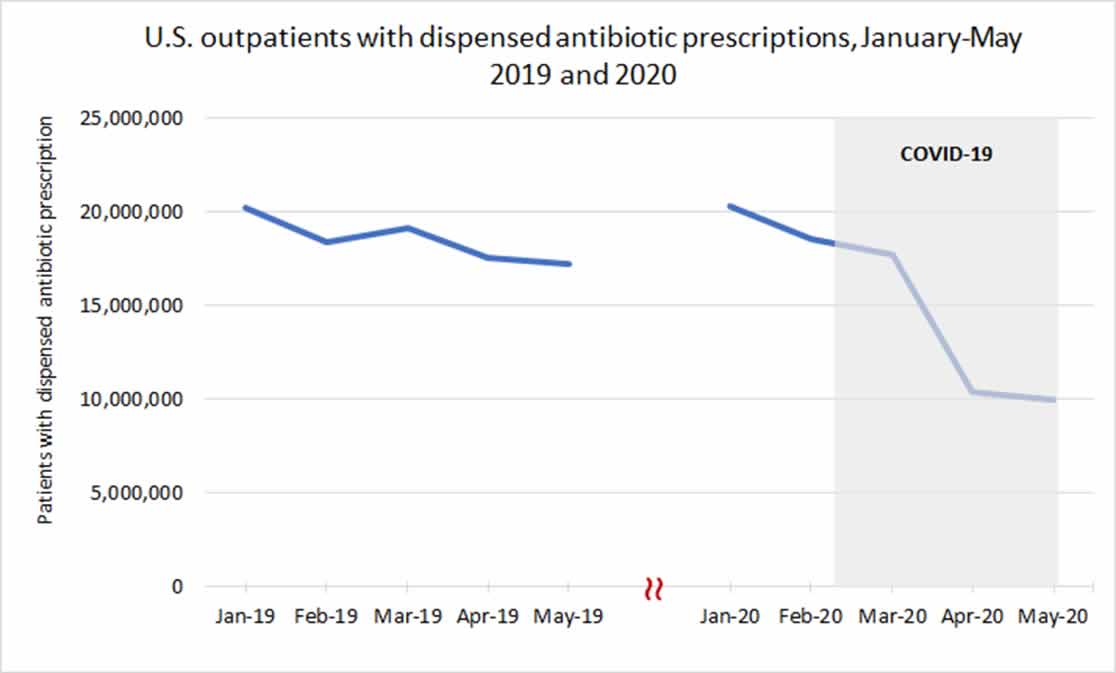
Data Source: IQVIA Total Patient Tracker
Inpatient Antibiotic Prescribing
Preliminary data suggest that inpatient antibiotic prescribing peaked in April 2020 but stabilized as the COVID-19 pandemic has continued. Antibiotics prescribed for treatment of community-acquired pneumonia, including ceftriaxone and azithromycin, have increased during the pandemic.
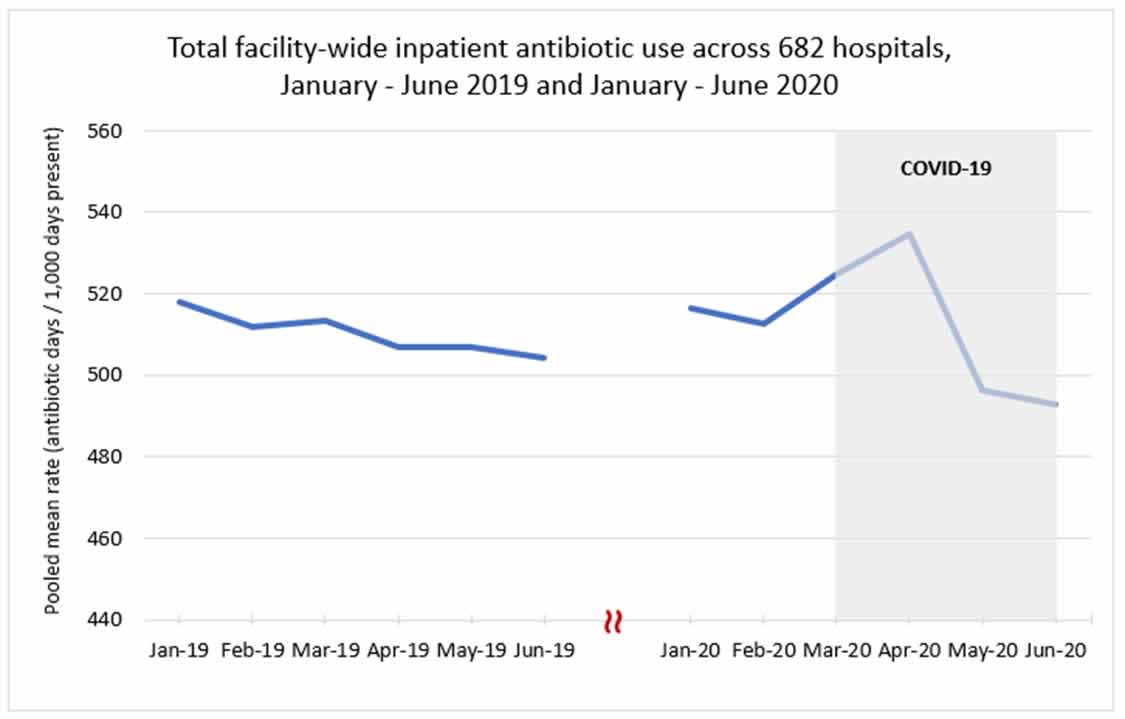
Data Source: CDC National Healthcare Safety Network Antimicrobial Use Option
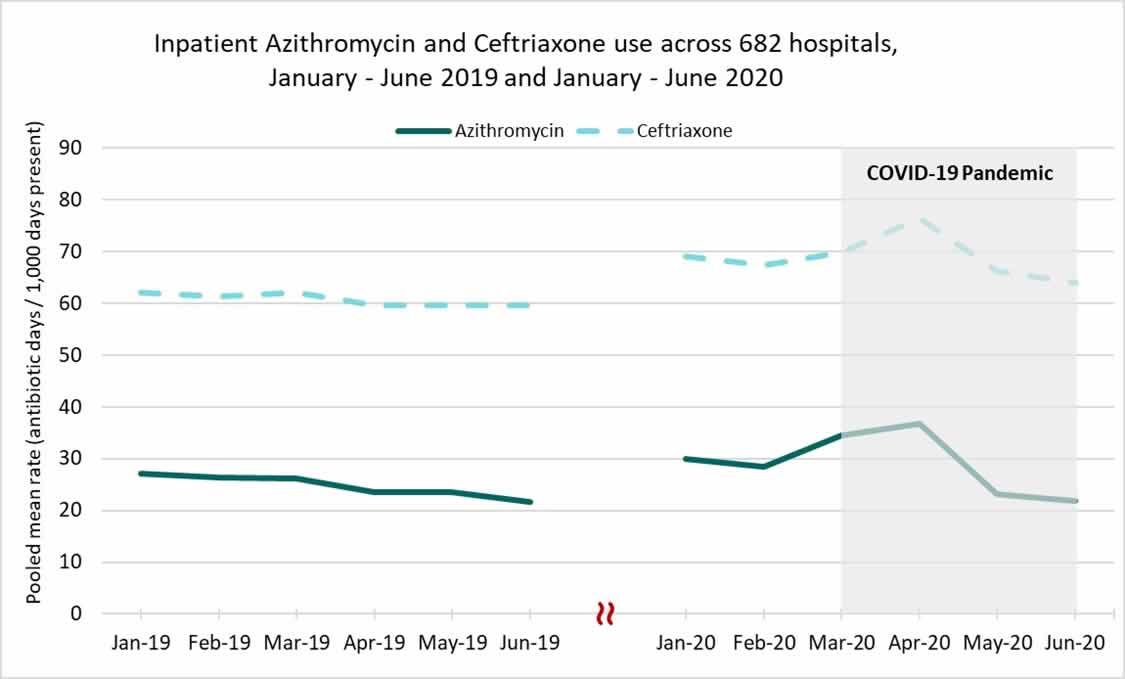
Data Source: CDC National Healthcare Safety Network Antimicrobial Use Option
Nursing Home Antibiotic Prescribing
Preliminary antibiotic prescribing data from nursing homes suggest a modest decrease in prescribing from January to June 2020 compared to 2019. However, similar to inpatient settings, an increase in prescribing of antibiotics used to treat pneumonia, particularly ceftriaxone and azithromycin, was observed from February to March 2020.

Data Source: PharMerica long-term care pharmacy prescription dispense data
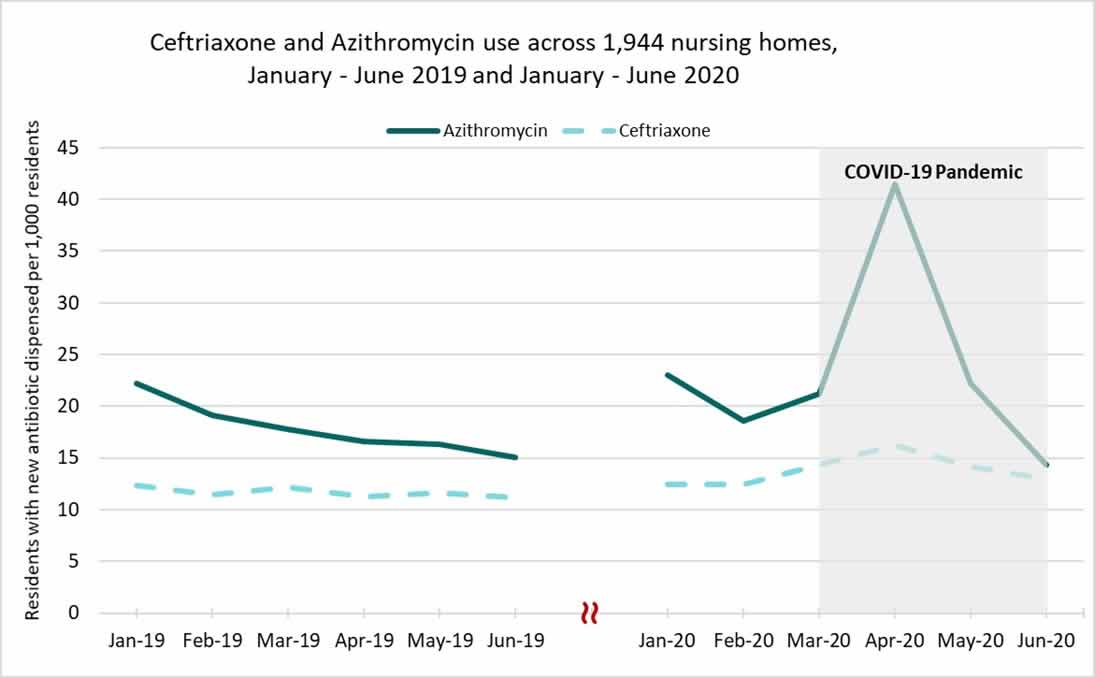
Data Source: PharMerica long-term care pharmacy prescription dispense data
Antibiotic stewardship efforts continue to be critically important to ensure patient safety in the changing landscape of healthcare during the COVID-19 pandemic. CDC Studies are ongoing to evaluate the effect of the COVID-19 pandemic on antibiotic use, antibiotic resistance, and antibiotic-associated adverse events.

CDC’s 2019 AR Threats Report presents data on the top 18 pathogens that require attention now, emphasizing that antibiotic resistance is a One Health problem affecting humans, animals, and the environment (soil, water).
CDC Antibiotic Stewardship Resources
CDC has many resources available on antibiotic use and stewardship for healthcare professionals, healthcare facilities, partners, and patients. Included in this section are updated and new resources.
Updated Web Pages and Resources
CDC’s Antibiotic Prescribing and Use website has been updated for easier navigation and includes these new resources:
- Information for patients on how to treat common illnesses, including whether antibiotics are recommended
- Six hospital pharmacy posters for pharmacists, describing 5 ways hospital pharmacists can be antibiotics aware
Core Elements of Antibiotic Stewardship
CDC’s Core Elements of Antibiotic Stewardship offers healthcare professionals and antibiotic stewardship leaders a set of key principles to guide efforts to improve antibiotic use, in order to protect patients and improve outcomes. This framework complements existing guidelines and standards from key healthcare partner organizations. The following Core Element documents are available for healthcare professionals and facility use in implementing antibiotic stewardship activities:
- **UPDATED** Core Elements of Hospital Antibiotic Stewardship Programs
- Implementation of Antibiotic Stewardship Core Elements at Small and Critical Access Hospitals
- Core Elements of Outpatient Antibiotic Stewardship
- Core Elements of Antibiotic Stewardship for Nursing Homes
- Core Elements of Human Antibiotic Stewardship Programs in Resource-Limited Settings
Be Antibiotics Aware and Get Ahead of Sepsis

What is Diagnostic Stewardship?
Diagnostic stewardship ensures that patients get the right test at the right time. It should ensure that tests happen when they are needed, that specimens are collected properly, and that results are given to providers in a timely manner to guide patient treatment. Guidelines developed for the treatment and management of infections should include criteria for the appropriate use of laboratory tests.
CDC educates the public and healthcare professionals (HCP) about improving antibiotic use through the award-winning national educational effort, Be Antibiotics Aware. Together with the Get Ahead of Sepsis educational effort, CDC is promoting the importance of antibiotic stewardship to ensure appropriate and timely antibiotic use in sepsis management. Antibiotics can save lives and are critical tools for treating infections, including those that can lead to sepsis. However, any time antibiotics are used, they can cause side effects or adverse events, such as Clostridioides difficile (or C. diff) infection and contribute to the development of antibiotic resistance. Improving the way healthcare professionals prescribe antibiotics, and the way we take antibiotics, helps keep us healthy now, helps fight antibiotic resistance, and ensures that these life-saving drugs will work when they are needed most, including for treating infections associated with sepsis.
CDC Training on Antibiotic Stewardship
CDC recently updated its antibiotic stewardship online training course that offers participants more than 10 hours of free continuing education . It can be accessed in multiple modules. Course objectives include informing healthcare professionals about proper antibiotic prescribing in all healthcare settings and the threat of antibiotic-resistant organisms, as well as encouraging open discussion among healthcare professionals and patients. Updated content includes new information on Serious and Urgent antibiotic resistance threats, guidelines and resources for dental prescribing, and the newly updated Core Elements of Hospital Antibiotic Stewardship Programs.
CDC collaborations with partners to improve antibiotic use across all healthcare settings
CDC continues to prioritize partner engagement and involvement in antibiotic stewardship activities spanning the health care continuum. Partners within health systems, including those in the community, long-term care, and acute care, all play a central role in implementing stewardship activities. Professional associations, payers, and state and local health department partners also make critical contributions to antibiotic stewardship efforts.
The following highlights a sample of the many important stewardship partners CDC works with regularly: Many of these partners also participated in the AMR Challenge, a yearlong effort by the U.S. government to accelerate the fight against antimicrobial resistance (AMR) from September 2018-September 2019. The Challenge resulted in more than 350 organizations across the globe committing to slow AMR. Partners participating in the AMR Challenge are marked with an *.
Henry Ford Healthcare System*
Henry Ford Health System, a Detroit -based integrated non-profit health system with six hospitals across southeast Michigan, developed an innovative process to improve the use of antibiotics at hospital discharge. The Antimicrobial Stewardship (AMS) team previously identified prolonged antibiotic therapy at discharge to be a challenge. The AMS Transitions of Care (TOC) process was implemented in November 2018 to optimize antimicrobial drug selection, dose, and duration at hospital discharge for patients with uncomplicated infections. The AMS TOC process at Henry Ford Health System is led by AMS pharmacists and clinical pharmacy staff practicing on the patient care wards. The pharmacists work with bedside nurses to identify patients likely to be discharged on oral antibiotics and collaborate with physicians to apply local guidelines for appropriate drug therapy and total duration. The pharmacists prepare the discharge prescription in the electronic medical record, including the appropriate stop date, and assess for barriers to medication access. The strategy demonstrated an improvement in optimal discharge antibiotics from 36% before to 77% after implementation. Patients receiving optimal antibiotics were also less likely to experience adverse drug events.
The full program overview and examples are available here.
PointClickCare*
PointClickCare, an electronic health records company for long-term care facilities, partnered with CDC to analyze millions of deidentified antibiotic orders and admission records in thousands of long-term care facilities across the United States. They have used antibiotic orders to describe prescribing practices, indications for antibiotic prescribing, and variability of antibiotic use rates across long-term care facilities to identify opportunities for optimizing prescribing practices.
PharMerica*
PharMerica, a long-term care pharmacy, partnered with CDC to provide and analyze antibiotic dispense data in more than one thousand long-term care facilities across the United States. Long-term care pharmacy antibiotic data was used to describe prescribing practices and track antibiotic use at the national level. PharMerica provided CDC with timely medication dispensing data to explore the effect of COVID-19 on prescribing practices in long-term care settings.
Society of Infectious Disease Pharmacists (SIDP)*
SIDP partnered with CDC and the American Society of Health-System Pharmacists to promote posters supporting “5 Ways Hospital Pharmacists Can Be Antibiotics Aware.” The campaign was highlighted on the SIDP Breakpoints Podcast to more than 1,000 subscribers as well as shared on social media platforms. Feedback was overwhelmingly positive, with members saying, “They are a great reminder how we as pharmacists can help in the fight against antibiotic resistance daily!” Links to the posters and SIDP’s activity guide are available here.
American Dental Association*
The American Dental Association (ADA) committed to creating and disseminating guidelines to help clinicians appropriately prescribe antibiotics for dental pain and swelling. These guidelines were released in 2019. The ADA also commits to publishing a survey of current antibiotic prescribing practices among dentists to demonstrate the need for such guidance.
Doctor on Demand*
Doctor on Demand is a national virtual medical care practice providing video-based encounters across all 50 states, delivering one million face-to-face doctor visits addressing a variety of urgent and chronic care issues. Doctor on Demand committed to lowering unnecessary antibiotic prescribing by 20% by December 2019 for acute upper respiratory infections including bronchitis, sinusitis and pharyngitis, and requiring two hours of continuing education training for all healthcare professionals.
The Pew Charitable Trusts*
The Pew Charitable Trusts has been a long-time CDC partner in the effort to better understand and improve antibiotic use in the United States. Pew strives to reduce inappropriate antibiotic use across healthcare settings by supporting efforts to track prescribing and establish data-driven targets for improving antibiotic use. In January 2020, Pew hosted the Tracking and Reporting Outpatient Antibiotic Use: Developing and Disseminating Effective Antibiotic Prescribing Feedback Convening. The convening brought together CDC subject matter experts, private payers, and representatives from state Medicaid and state health departments to develop antibiotic prescribing metrics for widespread use. As a direct result of this meeting, CDC is developing a comprehensive Payer Toolkit which will help insurers better track, report, and improve antibiotic use within their health plans.
Urgent Care Association (UCA)*
The Urgent Care Association co-hosted an Antibiotic Stewardship Summit in 2018 with Antibiotic Resistance Action Center (ARAC) and hosted the first annual Fall Urgent Care Clinical Consortium in September 2019. UCA has incorporated antibiotic stewardship as an essential component of their accreditation standard and, as of January 2019, they require all accredited urgent care centers to have at least one stewardship quality initiative as part of the overarching quality plan. Using CDC’s Core Elements of Outpatient Antibiotic Stewardship as a framework, UCA developed an Antibiotic Stewardship Commendation program, which is now open to all member organizations. UCA is pleased to have established a “Commitment to Antibiotic Stewardship” statement for the industry accompanied by a Read it. Sign it. Live it. Campaign.
Antibiotic resistance is one of the most critical health challenges we face today, with the potential to have a devastating long-term impact on a global scale. Responsible prescribing and accountability by the medical community are imperative to avoid catastrophic treatment failure.” – J.D. Zipkin, MD, MA, FAAP, FACP, Chief Medical Officer, GoHealth Urgent Care
State and Payer Partners
Aetna*
As one of the nation’s leading diversified healthcare benefits companies, Aetna, a CVS Health company, prioritized antibiotic stewardship as a way to improve health and lower avoidable costs. In partnership with CDC’s 6|18 Initiative, Aetna identified an audit and feedback intervention combined with peer comparisons as a method to improve antibiotic use in the outpatient setting, guided by the CDC Core Elements of Outpatient Antibiotic Stewardship. Aetna implemented the intervention over a three-year time period using existing and validated quality measures from the Healthcare Effectiveness Data and Information Set (HEDIS). The specific measure used for this intervention was the Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis, which indicates the percentage of healthy adults 18-64 years of age with a diagnosis of acute bronchitis and no other diagnoses that would warrant antibiotics who were not dispensed an antibiotic prescription. Healthcare professionals who practiced in ambulatory settings (excluding emergency departments) were included in this intervention. HEDIS data on the bronchitis measure were analyzed and used to categorize participating healthcare professionals into the following groups:
- High-prescribers: those who had at least five qualifying Aetna member patients and confirmed antibiotic prescriptions for more than 50% of patients diagnosed with acute bronchitis, and
- Champions: those who had at least three qualifying Aetna member patients and no antibiotic prescriptions.
In Year 1 of the initiative, Aetna identified healthcare professionals across the country who fell into these two categories based on the 2016 HEDIS measure. Letters signed by Aetna’s Chief Medical Officer were sent to both high-prescribers and champions. In Years 2 and 3, Aetna continued to notify healthcare professionals nationally and expanded the intervention with tailored letters from five collaborating state health departments. Through Aetna’s participation in CDC’s 6|18 Initiative and in collaboration with state health departments, Aetna successfully implemented the intervention in multiple states by sending over 4,500 letters to clinicians over three years.
Between 2016 and 2019, Aetna has observed an approximate 6% increase (+2% year-over-year improvement) in HEDIS performance in the percentage of adults not dispensed an antibiotic prescription for acute bronchitis. Health plans have the unique opportunity to leverage data in order to improve patient safety and outpatient antibiotic use. This intervention demonstrates that simple, low-cost, and evidence-based interventions can effectively reduce unnecessary antibiotic prescribing.
Florida Department of Health
Aetna mailed out letters to 120 high-prescribers and 6 champions. The Florida Department of Health (FLDOH) personalized the letter by including a signature from Dr. Carina Blackmore, the State Epidemiologist and Director of the Division of Disease Control & Health Protection. The letter also included materials from CDC’s Office of Antibiotic Stewardship Be Antibiotics Aware campaign.
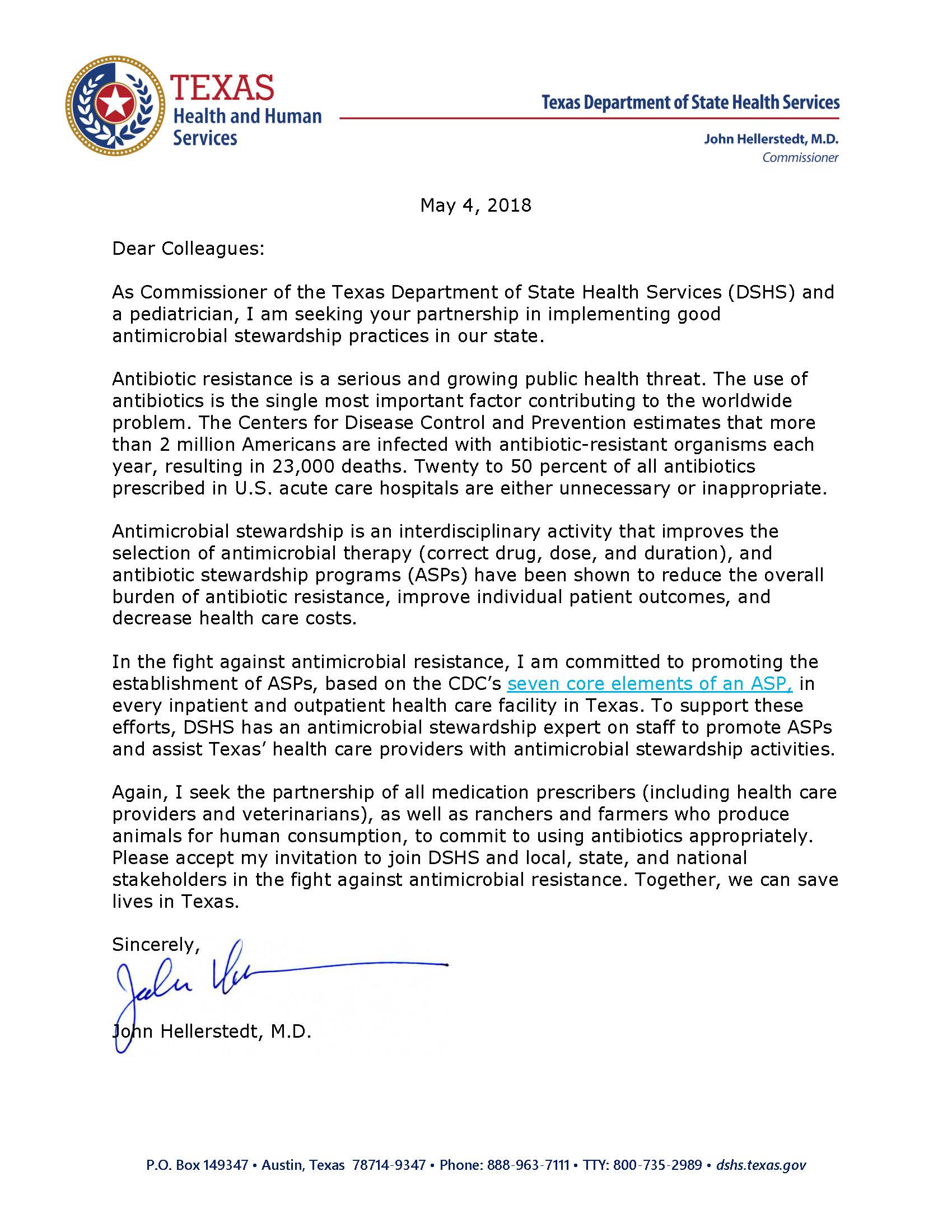
Texas Department of Health Commitment Letter
Aetna mailed out letters to 211 high prescribers and 14 champions. The Texas Department of Health (TDH) developed their own commitment letter with a signature from Dr. John Hellerstedt, the Commissioner of the Texas Department of State Health Services (DSHS). The commitment letter from TDH and DSHS was sent to clinicians in Texas along with the letter from Aetna.
Arkansas
Under CDC’s 6|18 Initiative, Arkansas’s Medicaid Agency and Department of Health partnered to improve outpatient antibiotic prescribing by analyzing data to target education and outreach to Patient-Centered Medical Home (PCMH) healthcare professional. The team assessed healthcare professionals’ antibiotic prescribing practices using episodes of care data available from Medicaid and the Healthcare Effectiveness Data and Information Set (HEDIS) measure for acute bronchitis as a complementary measure. Initial analysis showed variation in behavior and performance by health care site with an approximate four-fold difference in prescribing rates.
Kentucky – University of Louisville and Kentucky Department for Medicaid Services
The Child and Adolescent Health Research Design and Support (CAHRDS) Unit of the Department of Pediatrics of the University of Louisville School of Medicine was established to advance child and adolescent health by applying best evidence and research methods to various aspects of health and health care. In 2014, the University of Louisville formed a State University Partnership (SUP) with the Kentucky Cabinet for Health and Family Services, Department for Medicaid Services. The CAHRDS Unit performed a statewide analysis of antibiotic prescribing in children using Medicaid data. From 2012 to 2017, the total number of antibiotic prescriptions, rates of antibiotic prescriptions, and total antibiotic prescription spending increased. General practitioners (GPs) and nurse practitioners (NPs) prescribed the most antibiotic courses and several demographic differences in prescribing were observed; children residing in non-metro areas received more antibiotics. Additionally, a heat map revealed that some areas in Eastern Kentucky have three times the prescribing rate of the national average and other areas in Kentucky. Pharmacy claims were used to identify the top pediatric prescribers, and interviews were concentrated in Eastern Kentucky, the region with the highest prescribing rates in the state. Additionally, the CAHRDS Unit launched the Kentucky Antibiotic Awareness (KAA) Campaign 2017 during 2017 US Antibiotic Awareness Week, with the goal of reducing inappropriate antibiotic use across Kentucky. The KAA campaign created several educational resources for clinicians and patients, including an outpatient antimicrobial stewardship implementation workbook, commitment posters, and a children’s coloring book. In order to disseminate these resources and provide educational opportunities and CE activities to healthcare professionals, KAA has partnered with a variety of entities, including the Kentucky Department for Public Health, Centers for Medicare & Medicaid Services (CMS) Quality Improvement Organizations, healthcare systems, and professional societies.
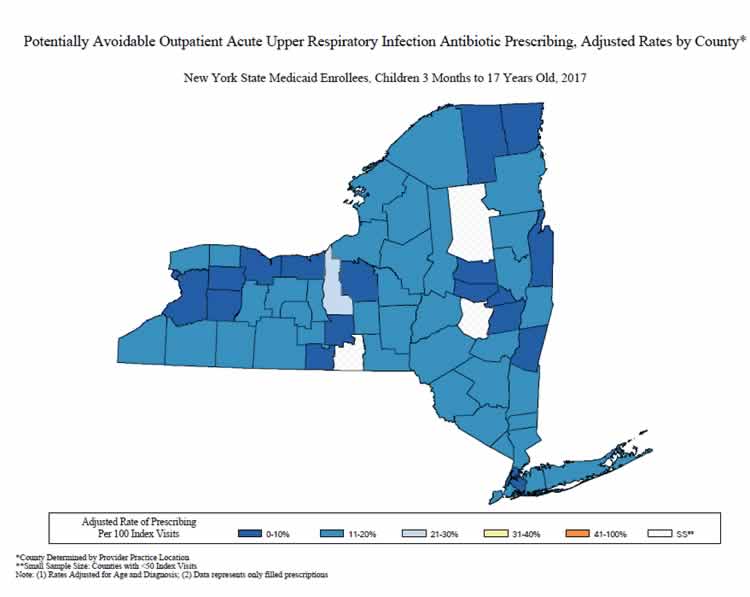
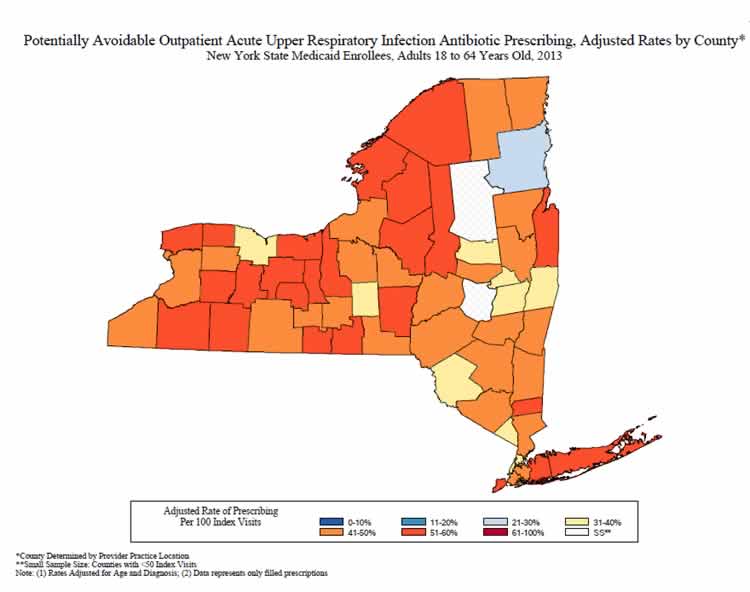
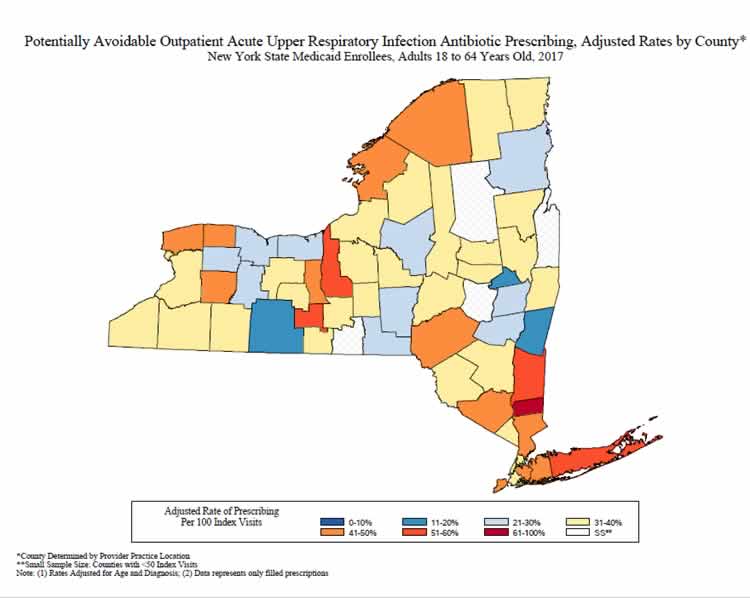
The New York State Department of Health (NYSDOH) identified antibiotic overprescribing for respiratory tract infections as an important issue. Analysis of New York State Medicaid claims data for calendar year 2013 showed that 45% of adult patients seen in outpatient settings for acute respiratory tract infections for which an antibiotic is not usually indicated filled a prescription following the visit. The rates of potentially avoidable antibiotic prescribing were mapped by the county of visit after adjusting for differences in age, principal diagnosis (acute bronchitis vs. cold/acute URI), and visit type (emergency department, institutional outpatient, professional outpatient). The NYSDOH Be Antibiotics Aware campaign used these data to drive improvement in outpatient settings through targeted outreach to healthcare professionals, development of clinician resources to support appropriate use of antibiotics, and by presenting the data to clinicians to demonstrate the need for improvement. A letter, signed by the NYSDOH Commissioner of Health and co-branded with the CDC campaign logo, was sent to over 2,900 healthcare professionals to promote appropriate antibiotic use. NYSDOH and the local county health departments have implemented interventions in pediatric offices, outpatient clinics, urgent care clinics, and schools, in addition to distributing over 105,000 educational materials. A follow-up analysis of Medicaid claims and pharmacy data identified a decrease in antibiotic prescribing over time, both among adult (18+ years old) and pediatric (3 months to 17 years old) populations. Fewer adults who were seen for acute URI had antibiotics prescribed in 2017 (37.4 per 100 visits) when compared to 2010 (46.5 per 100 visits). Over 12,000 fewer visits for acute URI had an antibiotic prescribed in 2017 than in 2010. Similar decreases were noted in antibiotic prescribing for acute URI with fewer children receiving an antibiotic when visiting the doctor for acute URI in 2017 (10.1 per 100 visits) than in 2010 (15.1 per 100 visits). NYSDOH continues to evaluate antibiotic prescribing data and take a multipronged approach to improving antibiotic prescribing and use in healthcare settings.
Sample of Pediatric Acute URI Antibiotic Prescribing Maps – 2013, 2017
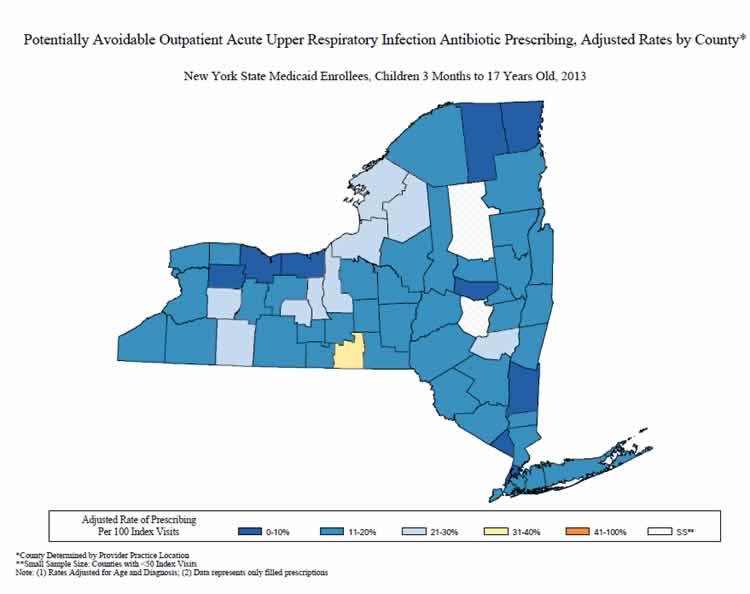
Sample of Adult Acute URI Antibiotic Prescribing Maps – 2013, 2017
Physicians for a Healthy California – Project AWARE
As the charitable arm of the California Medical Association (CMA), Physicians for a Healthy California (PHC) is dedicated to improving community health, building a diverse physician workforce and promoting health equity. To combat the growing threat of antibiotic resistance, PHC launched the Alliance Working for Antibiotic Resistance Education (AWARE) Project in 2000, a long-term, statewide effort to promote the appropriate use of antibiotics and decrease the spread of antibiotic resistance in outpatient clinical settings . Building upon the Core Element of Outpatients Antibiotic Stewardship of education and expertise, AWARE developed and disseminated the AWARE Toolkit, which includes a compendium summarizing key guidelines for 8 adult and 7 pediatric acute illnesses and patient education posters on appropriate antibiotic use and symptom management. The Toolkit is also available through the AWARE mobile app, which is currently being used in 22 countries. Additionally, in 2014, AWARE initiated a letter campaign with the purpose of promoting adherence to appropriate prescribing guidelines among physicians with high antibiotic prescribing rates. AWARE partnered with 10 large health plans across California to identify the highest 20% of antibiotic prescribers by volume. Each high prescriber was mailed a curated stewardship packet that included a cover letter, educational resources, and the AWARE toolkit. The cover letter introduced the purpose and goals of the AWARE project and summarized the educational content included in the mailing. The letter was also signed by the chief of the AWARE Steering Committee. Clinicians were not notified of their high-prescriber status but were referred to the AWARE website for additional clinical resources and patient education materials. Over the course of five years, AWARE mailed over one million toolkits to high prescribers in California, Oregon, Arizona, and Texas.