CDC Responds to a Dangerous Fungus Here and Abroad
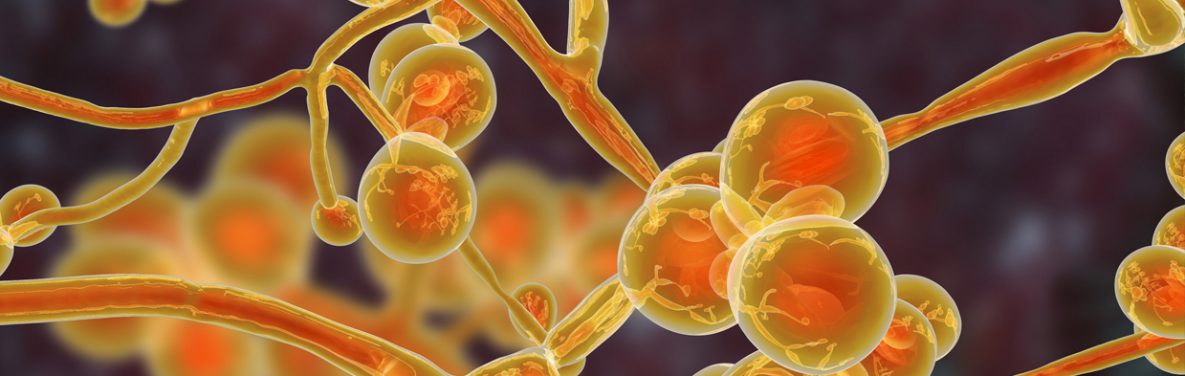
3D illustration of Candida auris, a drug-resistant fungus
Candida auris, or C. auris, is a drug-resistant fungus that is causing severe infections and deaths in hospitals around the world. Most strains detected so far have been resistant to at least one drug, and more than one third were resistant to two of the three major drug classes used to treat fungal infections. Particularly concerning, some strains have been found to be resistant to all three drug classes. This level of resistance has never been seen in other Candida infections.
CDC’s mycotics (fungal disease) experts are tracking this emerging phenomenon and working with countries to prevent, detect and respond to this threat.
C. auris was first reported in 2009 in Japan. To date, it has been detected in more than 20 countries, including the United States. Using whole genome sequencing, CDC scientists identified four different groups of C. auris that have emerged since 2009 in different parts of the world. In response, CDC is working with other countries to improve detection and implement aggressive control measures.
CDC’s work in Panama and Colombia highlights these collaborative efforts. In 2017, CDC confirmed the first case of C. auris in Panama. The Panama Ministry of Health requested CDC’s assistance to prevent C. auris from becoming a common cause of infection and to minimize deaths from this multidrug-resistant fungus. Together, CDC and Panama worked to
- identify links between patients with C. auris infections,
- uncover how the fungus was being transmitted,
- collect samples from the environment to determine if C. auris was present, and
- test people who had been in close contact with infected patients.
CDC has also worked closely with the Colombia National Institute of Health to investigate and contain cases of C. auris infections in Colombian hospitals. This collaborative work involved establishing public health surveillance for C. auris infections and using whole genome sequencing to track the spread of these fungal infections across Columbia.
Specialized laboratory methods are needed to accurately identify C. auris. Conventional laboratory techniques could lead to misidentification and inappropriate management of patients, making it difficult to control the spread of C. auris in healthcare settings. CDC worked with Panama and Colombia to use specialized methods to test patients’ blood and skin swabs to determine if patients are infected or colonized with C. auris. CDC also worked with these countries to develop recommendations for hospitals to control the spread of drug-resistant pathogens like C. auris and provided screening guidance to help hospitals identify patients colonized with C. auris – meaning those patients who carry C. auris on their body but do not have symptoms – so they can take aggressive steps to control the spread of infection to other patients.
To increase awareness of the emergence of C. auris in the region and share lessons learned from other countries, CDC is supporting regional and country-level meetings with leadership and technical representatives from ministries of health across Central America and the Dominican Republic. Also, CDC is working with the Pan-American Health Organization (PAHO) and the Council of Ministers of Health of Central America and Dominican Republic (COMISCA) to help countries to strengthen their capacity to conduct laboratory tests and surveillance for
C. auris and to take appropriate steps to respond when patients become infected with this potentially deadly fungus.
In the United States, 361 patients in 11 states have been reported as having laboratory-confirmed C. auris infection, and another 699 patients have been reported as having C. auris colonization, as of July 31, 2018. Working with seven state health departments that serve as the regional laboratories of the Antibiotic Resistance Laboratory Network, CDC scaled up specialized testing for C. auris. These strengthened testing capabilities—combined with efforts to increase clinicians’ knowledge and awareness about C. auris and to improve hospital infection control and prevention—will pave the way for the rapid identification and containment across all US healthcare settings.
Disease knows no borders, as demonstrated by the emergence and movement of C. auris around the world. The challenge of an emerging threat like C. auris requires an urgent and comprehensive response at all levels – local, state, federal, and international. CDC will continue to work with partners here and abroad to innovate and respond to the most serious emerging, drug-resistant infections.
To view a printable version of this page: CDC Responds to a Dangerous Fungus Here and Abroad [1 page]
